- Submissions

Full Text
Developments in Clinical & Medical Pathology
Self-Explanatory Non-Funded Project Study of Dysmenorrhea and Impact on Quality of Life in Rajgad Dnyanpeeth's College of Pharmacy-Savitribai Phule Pune University Pune
Rahul Hajare*
Biologics Development, Indian Council of Medical Research, India
*Corresponding author: Rahul Hajare, Biologics Development, Indian Council of Medical Research, New Delhi, India
Submission: February 17, 2018;Published: March 13, 2018
ISSN:2690-9731 Volume1 Issue1
Abstract
Dysmenorrhea, painful menstruation, is a common chronic condition of pain that affects a wide range of young women capable of reducing their quality of life, decrease their ability to function at a 100 percent and ultimately causing a reduction in productively for the affected person for a period of time. Many studies have shown that the level of knowledge about dysmenorrhea is unsatisfactory especially in young women and that it indeed has the ability to disrupt a peaceful flow in rhythm and pattern of women in executing daily activities, the aim of this study is therefore to determine the true extent at which dysmenorrhea interferes with daily activities in privately managed self-finance pharmacy institution.
Keywords: Dysmenorrhea; Physiotherapy; Nausea; Insomnia; Stomach cramps
Introduction
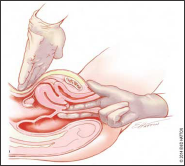
Primary dysmenorrhea is a pelvic pain syndrome during menstruation with no obvious signs of pathology especially in the pelvic region but with registered prostaglandin induced uterine contractions. Hence, there are symptoms like nausea and vomiting; also the pain subsides with time. In primary dysmenorrhea, palpation of the pelvic region should be painless and without pathological changes Secondary dysmenorrhea, testifies to the presence of pathology or disorder that is the lead causative factor for the pain, and this condition may continue even after menses. Conditions that are often seen as the underlying causes in secondary dysmenorrhea include endometriosis (Figure 1), pelvic inflammatory disease, and use of intrauterine device. In secondary dysmenorrhea, physical examination always reveals a tenderness of the pelvic region and possibly a deformed pelvic architecture. Quite a number of women (40%) complain of dysmenorrhea among which10%are unable to carry out daily activities between one to three days of each menstrual cycle [1,2]. Dysmenorrhea may have adverse influence over daily activities and function of women causing educational and career absenteeism. Dysmenorrhea may be influenced by different factors like, social status, nutrition, smoking, alcohol consumption, daily activity, psychological factors. Avoidance of food containing arachidonic acid such as dairy products, animal fat and reducing the intake of salt in the period of menstruation can reduce the pain of dysmenorrhea [3,4]. The results of some studies indicated that such healthy behaviors as bathing with warm water in the first days of menstruation, physical activity, consumption of fruits, vegetables and grains, and avoidance of salt and sugar can decrease the pain of dysmenorrheal (Table 1).
Table 1: Risk factors for dysmenorrhea.

Figure 1: Rectovaginal examination method to detect endometriosis.
Materials and Methods
Inclusion and exclusion criteria
The study population was comprised of pharmacy students of the RD College of Pharmacy-Savitribai Phule University, Pune within the age range of 16-45 years.
Study design and data collection instrument
Data collection was done using an 18-item self-administered questionnaire developed to capture the aim of this study between December and November, 2017. The questionnaire was translated to Marathi language and thereafter translated back into English language by a different person in order to assess validity. We evaluated menstrual history as well as physical and psychological symptoms, the study also evaluated the impact of dysmenorrhea on quality of life. 368 questionnaires were administered, 317 were filled and returned, 31 questionnaires were not returned while 20 questionnaires were incorrectly filled (response rate: 86%). The respondents were allowed a free hand in their responses to questions and only guided upon request. Respondents were also assured about the confidentiality of their information.
Data analysis
Data was entered and analyzed using Statistical Package for Social Sciences 11.5 (SPSS 11.5) [5,6]. Descriptive statistics of socio-demographic information, menstrual history and symptoms of participants regarding dysmenorrhea as well as impact on quality of life were determined and reported in the forms of mean, standard deviation, proportions and percentages.
Ethical aspects
All participants in the study were informed about the study objectives of the and all information about the instrument were explained to them by well-trained students. Ethical clearance was obtained from all the concerned college bodies for conduction of the present study [7].
Results
Baseline
The average participant's age was 20 years+/-1.206 years (ranging from 17-30 years). 24% (76) were found to be less than 20 years of age whereas only 8% (25) were above 22 years of age. Most of the responders, 68% (216) fell within the age group of 20-24. The mean BMI of the participants was 22.03+/-2.27kg/m2 (ranging from 16.8kg/m2 to 33.04kg/m2). Most of the participants had a normal BMI (18.5-25) which was around 69% of the total participants. Participants in the underweight and overweight categories had almost equal distribution with 17% were and 14% respectively.
Menstrual characteristics
The prevalence of dysmenorrhea was very high with 68.4% (217) with about 20% of the participants who experienced pain, rating their pain as '8' (slightly severe). The average age of menarche was 12.98+/-1.10years, (10 to 15 years). Majority of the women, i.e. 68% (216), had started menstruating between 12-13 years of age.
Association of age with dysmenorrhea
There was a significant association between age of menarche and occurrence of dysmenorrhea (x2 =11.34 df=2 and p value=0.003). The age group of 12-13 years was taken as the reference category; a bivariate analysis showed that females who had menarche at 15 years and above had a higher chance (32%) of reporting dysmenorrhea when compared with participants who were in the age category of 12-13 years. The observed difference was statistically significant (RR: 1.24; 92% CI: 1.03-1.50). Also, we found that participants who had menarche at 11 years or below had a 21% chance of reporting dysmenorrhea when compared with those in the reference category. This difference was also found to be statistically significant (R.R: 1.20; 92% CI; 1.12-1.49).
Length of the menstrual cycle
Average duration of the menstrual cycle among the 317 respondents was 28.52+/- 2.37days (22-40 days). Majority of the women had menstrual cycle duration of 28 to 30 days; 56.7% (180), which is considered as normal. Considering that a very small number (2.1%) had menstrual duration of 35 days or more, we did not evaluate any association between cycle duration and dysmenorrhea.
Family history
Most of the participants did not report family history of dysmenorrhea; 60.5% (192). Of the 24.3% (77) women who reported family history of dysmenorrhea, 82% (260) experience dysmenorrhea themselves. A bivariate analysis was performed and proved to be statistically significant (x2=32.5 df=1 and p value=0.000). We therefore concluded that participants with a family history of dysmenorrhea had a 1.52 higher chance of experiencing the same condition when compared to women without a family history (RR: 1.32; 92% CI=1.18 -1.53) [7].
Premenstrual symptoms
Premenstrual symptoms were grouped as physical and psychological. It should be noted that some participants reported more than one physical and psychological symptoms and these were reflected in the percentages.
Physical symptoms
253 (79.8%) participants out of the 317 total participants, indicated experiencing physical premenstrual symptoms. Backache and stomach cramps were reported by 52.3% and 50% respectively while cold sweats was reported by only 6.8% of the women. We found an association between physical symptoms and dysmenorrhea (x2=125.36 df=1 and p value=0.000). We also found that women who had physical premenstrual symptoms had 54.3 higher chance of experiencing dysmenorrhea when compared with no physical symptoms and this difference was found to be statistically significant (RR 54.65, 93% CI=10.46- 204.63). Most of the participants that had dysmenorrhea experienced some form of premenstrual physical symptoms.
Psychological symptoms
298 (94%) of the 317 participants reported to have experienced some form of psychological symptoms. Out of these, 61% (182) of the participants had experienced irritability whereas 25.6% (76) reported insomnia as the main problem. Women who did not experience any form of psychological symptoms were taken as the reference category and others were compared to this. Our results were as follows: women who experienced irritability were 1.34 times more likely to have dysmenorrhea when compared to women with no psychological symptoms and the difference was statistically significant (RR: 1.34, 93% CI: 1.32-2.16). Women who experienced insomnia were 1.87 times more likely to have dysmenorrhea when compared to women who did not experience psychological symptoms and the difference was statistically significant (RR: 1.87, 93% CI: 1.84-2.35). Women who experienced anxiety as their main symptom were 2.0 times more likely to have dysmenorrhea when compared to reference category and this was also statistically significant (RR: 2.0, 93% CI: 1.94-2.62).
Treatment and dysmenorrhea
48.9% of respondents who had dysmenorrhea took some form of treatment. Among these, 70.2% women took medications: (24% took Analgesics, 27% took Antispasmodics and 19.2% took both). 53.7% of respondents did Physiotherapy, 87% used hot water bag while 32% women did both meditational and Physiotherapy treatment.
Quality of life and dysmenorrhea
In this bivariate analysis, 'normal' QOL (65%, 206) was regarded as the reference category and all other analysis was done in reference to this. 'Normal QOL' was taken as women who could attend classes or perform daily activities with minimal or little discomfort. Participants who experienced dysmenorrhea were 5.8 times more likely to stay in bed all day when compared to women who did not experience any form of dysmenorrhea and the difference was found to be statistically significant (RR: 5.8, 92% CI: 4.28 to 7.96) . We also noticed that participants who had dysmenorrhea were 5.24 times more likely to stay at home all day when compared to women who did not experience dysmenorrhea and the difference was found to be statistically significant (RR: 5.24, 92% CI: 4.28 to7.96) . Also, participants who reported dysmenorrhea were 5.09 times more likely to attend college after taking medication when compared to the reference category and the difference was found to be statistically significant (RR: 5.09, 92% CI: 4.20 8.29). Lastly, we found that participants who had dysmenorrhea were 4.78 times more likely not to attend classes without taking medication when compared to reference category and the difference was found to be statistically significant ( RR: 4.78, 92% CI: 3.98 to 7.43).
Discussion
Dysmenorrhoea is one of the most common problems affecting majority of women and substantially affects the overall quality of life of sufferers added to the constant embarrassment and disruption of routine life. Our study showed an overall prevalence of 217 (68.4%) for dysmenorrhea in girls aged 12-19 years. Such divergence between these studies is self-explanatory when noted that the participants in the former studies were adult women and not majorly adolescents like observed in our study, where dysmenorrhea is more prevalent at the extremes of reproductive life. The absence of a universally accepted method of defining dysmenorrhea may account for such disparities, as this affects the methods used in collecting data and the study definitions of dysmenorrhea and pain. Hence, the selected groups of women may account for the variation in these estimates. The average age of menarche in our study was 12.98+/-1.10 years, quite similar to findings observed in other studies. We observed that 49.6%, 30.4% and 20% of students had mild, moderate and severe pain respectively compared to a study done in Turkish University, which reported 66.6% participants having moderate and severe dysmenorrhea. Dysmenorrhea is generally associated with physical and psychological symptoms such as nausea, reduced appetite, irritability, headache, insomnia, diarrhea, nervousness etc. In our study, participants reported stomach cramps (50%), nausea (27.3), insomnia (25.6%) and irritability (61%) respectively. Irritability (61%) was the most common associated psychological symptom followed by difficulty in concentration (48.8%). High prevalence of dysmenorrhea as reported by our study makes dysmenorrhea a significant public health challenge among female population that demands considerable attention from policy makers. When analyzed, students with dysmenorrhea scored significantly lower in many of the SF-36 domains including physical functioning, general health perception, and vitality, consistent with recent studies by scientist, implying that women with dysmenorrhea and other related menstrual symptoms recorded lower health related quality of life values.
Conclusion
Dysmenorrhea is a common health problem and high gynecological referral rate due to its high prevalence rate. It exerts a significant effect on the daily activities and a detrimental effect on the quality of life among the female population.
Recommendation
Based on the findings of our study, the following recommendations are suggested
a) Increased educational programs to improve the level of awareness of dysmenorrheal.
b) University and educational inspectors may benefit from considering dysmenorrhea in the context of improving their University's attendance rates and academic performance.
c) Separate girl’s common room.
d) Appointment of full time nurse in appropriate scale.
e) Additional chemist shop reserve in Institution campus.
f) Transportation facility in reasonable cost.
g) Increase cleaning time of surface area of institution twicea day.
h) Create a space for biosafety theory class hours in time table to reduce the hesitation of awareness of dysmenorrhea and theirs associated problem. Includes a list of common questionnaires in common use.
i) Yoga session class twice a week with instructor may beneficial to reduce depression sign.
j) Appointment of Gynecologist with class hours basis and interactive session.
k) Diet awareness workshop in dysmenorrhea once in a semester
Limitation
This study was a cross-sectional study; hence, it precludes inferences of causality among such variables. Furthermore, the nature of self-reporting may have impacted the under-reporting of the conditions.
Controversies
The authors acknowledge there was no external financial support for this study. We also appreciate the anonymous reviewers for their consistency and constructive comments that helped strengthen this article.
Acknowledgment
This study has been guided by under supervision and guidance of Renowned Laboratory Scientist Respected Dr. Ramesh Paranjape' Retd Director and Scientist ‘G’ National AIDS Research Institute India. I express my sincere gratitude towards Respected Sir' for motivation and being great knowledge source for this research.
References
- Zhikun C (2008) Simulation and experimental study on the flexible spine of robot fish. Harbin Institute of Technology (Natural Science Edition), Harbin.
- Hong C (2006) Study on the Motion Mechanism of Cruise and Maneuvering of Biomimetic Robot Fish. University of Science and Technology of China, Hefei.
- JM Donley, Epulveda CAS, Konstantinidis P (2004) Convergent Evolution in Mechanical Design of Lamnid Sharksand Tunas. Letters to Nature 429: 61-65.
- Zuo C (2013) Design and experimental study of swing drive flexible robot fish. Harbin Institute of Technology, Harbin.
- Yaohui Y (2014) Research on the robot fish for mine flooding accident detection. China University of Mining and Technology, Beijing.
- Chunzhao G (2007) Optimization design and simulation of virtual fish-mimetic robot based on the fish body muscle model. University of Science and Technology of China, Hefei.
- Yingxiang L (2007) Two joint robot fish body and dynamics research. Harbin Institute of Technology, Harbin.
- Qian W (2009) Dynamic analysis of three-joint robot fish without lift potential swimming. Xi'an University of Technology, Xi'an.
- Shuxin Z, Qingsong H (2013) Three-dimensional modeling of carp and numerical calculation of flow field force. Journal of Shanghai Ocean University 22(6): 855-861.
- Guan Z, Gao W, Gu N (2010) 3D Hydrodynamic Analysis of a Biomimetic Robot Fish: Control, Automation, Robotics, and Vision. Singapore, pp. 793-798.
- Park HC, Lee E, Choi HS (2013) Application of FSI (Fluid Structure Interaction) to Biomimetic Robot Fish: International Conference on Ubiquitous Robots and Ambient Intelligence (URAI). Ramada Plaza Jeju Hotel, Jeju, Korea, pp. 439-441.
- Yadong H, Weijie Z, Shengkuan Y (2014) Design and magnetic circuit calculation of electromagnetic steering gear for underwater vehicle. Water Warfare and Ship Protection 22 (1): 49-51.
- Shumeng L, Bin L, Zhiyuan L (2011) Design and experimental study of driving coil of coil drivers. Foreign Electronic Measurement Technology 30 (8): 54-57.
- Xiaome D (2006) Research on a number of technical issues of miniature electromagnetic driver. Tianjin University, Tianjin.
- Guangming X, Chenguang H (2013) Autonomous biomimetic robot fish. Harbin Engineering University Press, Harbin, pp. 22-40
- Weiwei S (2009) Study and design of caudal fin propulsion system for biomimetic robot fish. Yanshan University, Hebei.
- Wenguang W (2010) Experimental study on the propulsion performance of the biomimetic tuna robot fish. China University of Science and Technology, Anhui.
- Chang L (2007) Study on modeling and control method of caudal fin robot fish. Harbin Institute of Technology, Harbin, p. 2.
© 2018 Rahul Hajare. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






