- Submissions

Full Text
Developments in Anaesthetics & Pain Management
A Randomized Control Trial of Multimedia Interventions to Improve Pain Education among Veterans with Chronic, Non-Cancer Pain
David Cosio
Department of Anesthesiology/Pain Clinic, Jesse Brown VA Medical Center, USA
*Corresponding author: David Cosio, Department of Anesthesiology/Pain Clinic, Jesse Brown VA Medical Center, USA
Submission:December 02, 2022;Published: December 21, 2022

ISSN: 2640-9399 Volume2 Issue3
Abstract
The current study explored how the effects of an empirically supported, patient pain education intervention translated into multimedia (such as a DVD, a booklet, or both) in a randomized control trial. A sample of 76 Veterans who were elected to complete the pre-and post-intervention measures were evaluated. The primary outcome analysis was a 3x2 Repeated Measures (RM) Multivariate Analyses of Variance (MANOVA), with “Intervention Arm” as the between-subjects factor and “Time” as the withinsubjects factor. A significant univariate main effect was obtained for the primary measures of pain intensity (now), but the scores worsened as opposed to improving. There was no significant univariate main effect for the primary measures of readiness to adopt self-management approach. Significant univariate main effects were also obtained for the secondary measures of factual knowledge (decreased) and in depression scores (increased), which indicate a significant deterioration in those areas. There was no significant univariate main effect obtained for the secondary measures of pain knowledge, pain experience, and attitudes or beliefs about pain. The current study underlines the potential negative aspects to using multimedia to replace personal interaction from providers.
Keywords: Chronic pain; Veterans; Pain education; Multimedia; Psychoeducation
Introduction
Education is the best analgesic. Research has shown that patients who receive clear information regarding pain and treatment are more likely to be satisfied with their care and symptom improvement, adhere to treatment recommendations, and use self-management strategies [1]. Educating patients on chronic pain and self-management improves knowledge, pain outcomes, and compliance [2,3]. Without proper pain education, patients may be misinformed or maintain unrealistic expectations regarding their pain prognosis and treatment [4,5]. Furthermore, patients who maintain impractical beliefs and attitudes about their pain are less likely to engage in self-management behaviors and more likely to seek more invasive interventions for pain relief [6]. Pain is one of the most common reasons Veterans consult with their primary care providers [7] and is one of the most prevalent symptoms reported by returning Veterans [8]. Forty-eight percent of Veterans within the Department of Veteran Affairs (VA) healthcare settings experience pain on a regular basis [9]. One study found that U.S. soldiers screened within 90 days of returning from a one-year combat tour in Iraq were two-to-four times more likely to have a migraine as compared to the general population [10]. An estimated 17.6% of Gulf War Veterans have also shown symptoms associated with fibromyalgia [11]. Veterans are often more complex in their presentation of chronic pain than the general population due to difficulties returning to civilian life and the influence of their past military service on their pain experience [12]. In fact, past research has found that past military service may contribute to a hypersensitivity to pain symptoms [13-15].
The VA has proven to be an ideal setting to develop and implement formal, selfmanagement education programs [16]. Cosio D et al. [17] developed and implemented an in-person pain health education program to address an identified need for patient pain education within the VA [17]. Past findings indicate that Veterans who elected to complete the program reported a statistically significant difference in pain intensity, readiness to adopt a self-management approach, experience of pain, and depressive symptoms, but failed to show a change in knowledge acquisition [18]. Additional studies have found improvement in knowledge acquisition with the incorporation of audience response technology [19]; patient satisfaction [20]; and provider satisfaction with this particular program [21]. However, some Veterans report scheduling conflicts, such as employment or collegiate careers, which impede them from participating in formal face-to-face pain health education programming. Low-intensity interventions, such as Digital Video Discs or Digital Versatile Discs (DVDs) and written education materials, may be able to improve Veterans’ pain intensity and readiness to adopt self-management approach, but could also be used to help prepare these patients for more intensive self-management interventions [22].
One of the earliest studies investigating multimedia for use in educating patients about patient-controlled analgesia found the intervention made a significant difference in pain knowledge, produced better outcomes in pain relief, and received the endorsement of patients on its usefulness [4]. Several other studies in health education, such as fall prevention [23]; laparoscopic cholecystectomy [24]; COPD [25]; and cancer pain [26], have also been conducted, and provide support for the use of DVD-based interventions to address health education needs. One published venture in multimedia-based education and non-cancer pain is its application to improve readiness to self-manage joint pain [22]. The current study explored how the effects of an empirically supported, patient pain education intervention translated into multimedia (such as a DVD, a booklet, or both) in a randomized control trial. Primary outcome measures of the current study were whether the use of multimedia promoted a decrease in pain intensity and an increase in readiness to adopt a self-management approach among Veterans with chronic, non-cancer pain. Secondary outcomes included whether Veterans who participated in a low-intensity, pain education intervention using multimedia would increase in factual pain knowledge; experience decreases in intractable pain; demonstrate positive changes in their attitudes or beliefs about their own pain problem; and demonstrate a decrease in depressive symptoms.
Methods
Participants
Figure 1:Flowchart of study participants.
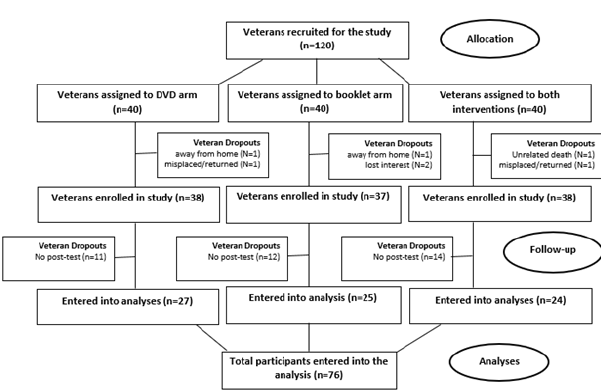
A total of 120 Veterans with mixed, idiopathic (back, neck, extremity, head, and fibromyalgia), chronic pain voluntarily participated in a multimedia-based, patient pain education program at a Midwestern VA Medical Center between January 3, 2017-October 1, 2018. All the Veterans were recruited from the pain clinic during their weekly patient intake orientations, of which seven (6%) dropped out of the study due to being away from home (N=2), misplacing materials/returned to sender (N=2), losing the desire to participate (N=2), and unrelated death (N=1). Potential candidates had several characteristics, including having failed medical/surgical treatment; exhibited an overreliance on medications/ therapies; displayed pronounced inactivity; suffered from significant depression or anxiety related to his/her pain; demonstrated inadequate coping skills; and/or appeared receptive to adopting a self-management approach to pain management. The current study had two exclusion criteria-Veterans must not have been able to attend the face-to-face intervention due to a conflict in their schedule (e.g., employment or collegiate career) and must have had access to a DVD player. After the Veteran was identified, a research team member approached the candidate and explained the potential risks and benefits of participating in the current study. Veterans were given an opportunity to ask any questions at that time. Participants were free to withdraw from the study at any time. Upon completing the informed consent and HIPAA Authorization forms, Veterans were randomly assigned to one of three conditions. A third of the sample were assigned to the DVD arm of the intervention (N=40), a third to the booklet arm (N=40), and a third to both (N=40). Participants were asked to complete the pre-intervention assessment when they received their assigned pain education materials. Participants were instructed to review the pain education materials within three months’ time in order to correspond with the timeline of the in-person intervention. After three months, the Veterans were mailed their post-intervention assessment which included the same battery of measures. Three follow-up reminder calls were made, duplicate questionnaires were mailed, and return envelopes were provided to improve the response rate. Upon completion of each assessment, Veterans received a gift card and were allowed to keep the pain education materials given as part of the low-intensity intervention. Approximately 63% of the sample (N=76) completed both the preand post-intervention assessments, while 37% did not (N=44) (Figure 1). This is within an acceptable range of response rates, which past research approximates 60% for most research should be the goal [27]. A limited medical records review was conducted as part of the current study to retrospectively determine the age at time of treatment, sex, and race/ethnicity of the participants. The current study was reviewed and approved by the affiliated university’s Institutional Review Board (IRB) and the VA’s Research and Development Office. The study used a single-blind design in which investigators, but not participants, were aware of the condition to which the participant had been assigned. The content of each intervention condition is described below.
Interventions
DVD Intervention. The DVD arm of the intervention consisted of a three-disc set which included the thirteen edited classes previously filmed in the face-to-face Pain Education School program. The original, face-to-face Pain Education School was developed and implemented in a Department of Veterans Affairs (VA) Medical Center using the National Center for Health Promotion and Disease Prevention’s step-by-step guidelines in Veterans with chronic, non-cancer pain [17]. The face-to-face program consists of an introduction class followed by twelve hour-long classes offered weekly that are led by guest speakers from over twenty different disciplines within the facility. The face-to-face program lasts approximately three months’ time. Thirteen modules were created from the face-to-face intervention in order to provide the participant a menu of pain treatment options, including an introduction module followed by segments on Pain Clinic/Osteopathic Manipulation, Medication Management, Smoking Cessation/Addiction Services, Nutrition Services/MOVE! Weight Loss Program, Physical Medicine and Rehabilitation, Recreation Therapy/Sexual Health, Cognitive Behavioral Therapy (CBT)/Acceptance and Commitment Therapy Groups, Suicide Prevention and Mental Health/Vocational Rehabilitation, Hypnosis/Biofeedback, Healing Touch/Spirituality, Sleep Clinic/Insomnia CBT Group, and Acupuncture and Traditional Chinese Medicine. Each clip on the DVD from each discipline (30- 45 minutes each) shared information about chronic, non-cancer pain from their perspective, what treatments are available in their service, and how to access their respective clinics. Booklet Intervention. The booklet arm of the intervention only included the written materials (PowerPoint presentations) used with Veterans who participated in the same face-to-face intervention. The third arm of the intervention included both aspects aforementioned.
Measures
As part of the introduction to the intervention, all participants completed a standard set of pre-intervention assessment measures. The battery of measures in the current study included the Numeric Rating Scale (NRS-11), the Readiness Questionnaire, Patient Pain Questionnaire (PPQ), the Pain Information & Beliefs Questionnaire (PIBQ), and the Patient Health Questionnaire (PHQ- 2). These measures were chosen based on their brevity and ease of administration, as well as their reliability and validity in prior research. All participants were asked to complete the same battery of measures at post-intervention. Numeric Rating Scale (NRS- 11). The NRS-11 is an 11-point scale for self-reporting of pain for adults and children over 10 years old (National Institutes of Health, 2003). Scores range from 0 to 10, with “0” meaning no pain, “1 to 3” mild pain, “4 to 6” moderate pain, and “7 to 10” severe pain. Past research suggests that the difference expected from adding education materials is relatively small, approximately one point on the 0-10 rating scale. The NRS-11 has historically been tested with established test-retest reliability [18]. Readiness Questionnaire. Veterans were asked to select one statement out of five items that best describes their stage of readiness to adopt a self-management approach to their pain. Scores ranged from “1 to 5” with larger numbers indicating more readiness to adopt a self-management approach. The measure was sampled from the stages of change from the Transtheoretical Model, the intended domain of content which provides content validity. The Readiness Questionnaire has historically been tested with established temporal stability [18]. Patient Pain Questionnaire (PPQ). The PPQ is a 16-item ordinal scale that measures the knowledge and experience of a patient in managing chronic, or persistent, pain. The PPQ includes seven items that measure the Veteran’s experience with pain. Nine items of the PPQ measure pain knowledge but focused mainly on pain medication. All items were formatted such that “0” was the most positive outcome and “10” was the most negative outcome. Knowledge subscale scores ranged from “0 t 90,” and experience subscale scores ranged from “0 to 70.” The PPQ tool has historically been tested with established reliability and validity [2].
Pain Information and Beliefs Questionnaire (PIBQ):
The PIBQ assesses two constructs independently, factual knowledge and attitudes/beliefs. The first section was composed of 19 dichotomously scored (true-or-false) questions in which patients were instructed to identify facts about intractable pain. The second section was composed of 9 items in which the patient indicated the extent of agreement on a 6-point rating scale, with each statement reflecting an attitude or belief about the patient’s own pain problem. The PIBQ was originally developed using factor analysis. The PIBQ tool has historically been tested with established reliability [28].
Patient Health Questionnaire (PHQ-2):The PHQ-2 inquires about the frequency of depressive symptoms over the past two weeks, scoring each as 0=“not at all” to 3=“nearly every day.” Scores ranged from “0 to 6.” A PHQ-2 score>3 has a sensitivity of 83% and a specificity of 92% for major depression [29].
Data analyses
The current study used a randomized control trial design. Oneway analyses-of-variance identified differences on demographic and outcome variables at baseline. Paired-samples t-tests were conducted to evaluate the effect of the intervention on the outcome variables from baseline to post-treatment. The primary outcome analysis was a 3x2 Repeated Measures (RM) multivariate analyses of variance (MANOVA), with “Intervention Arm” as the betweensubjects factor and “Time” as the within-subjects factor. The dependent variables were the primary outcome variables of pain intensity and readiness to adopt self-management approach, and the secondary variables of pain knowledge, pain experience, factual knowledge, attitudes and beliefs, and depressive symptoms. Data were collected using paper measures and analyzed using PSPP, a free alternative to IBM’s SPSS® [30]. The intervention outcome analyses used an intent-to-treat approach. A last-observationcarried- backward approach was used for missing pre-intervention assessment data [31], and a baseline-observation-carried forward approach was used for missing post-intervention assessment data [32]. A multivariate power analysis was calculated with an anticipated effect size of R2= 0.06, a p ≤ 0.05, and a sample size of N=120, and the power was appraised to be 80%.
Result
Sample characteristics
Of the 120 Veterans referred to the study, 113 were enrolled and 76 completed both the pre-and post-intervention measures (Figure 1). Veterans had mixed idiopathic chronic, or persistent, noncancer pain conditions, including back pain, neck pain, extremity pain, head pain, and fibromyalgia/soft tissue pain. Most veterans were African American (N=59, 49.1%), but 51 (42.5%) were Caucasian, eight (6.7%) identified as being Hispanic/Latino, and two (1.7%) were identified as “other” races. Most were males (N=99, 82.5%), but there were also a large number of female veterans (N=21, 17.5%). The average age of the Veterans was 56 years old, and the youngest returning Veterans (17-24 years old) were not a well-represented age group. The average baseline pain score was “5.56,” which falls within the moderate pain level. The average Veteran reported being in the contemplation-preparation stage of readiness to adopt a self-management approach. Veterans exhibited a moderate level of pain knowledge and negative experiences due to pain at baseline. On average, Veterans were most likely to be able to reca factual information and endorse items consistent with strategies of conservative pain management. The average Veteran did not experience a major depressive episode over the previous 2 weeks.
Baseline differences
There were no significant baseline differences in arm of intervention (p=0.491) or sex (p=0.730) among completers versus non-completers. However, African American participants (73%) were the most likely to complete both assessments and Veterans from “other” races were the least (p=0.023). There were no significant differences in demographics or baseline scores among the three arms of the intervention (ps>0.127), except those who were given the DVD were in more agreement with strategies of conservative pain management when compared to those who were also given the book (p=0.003). There were no significant differences in demographics or baseline scores between the sexes (ps>0.079) or among races (ps>0.062).
Primary outcomes
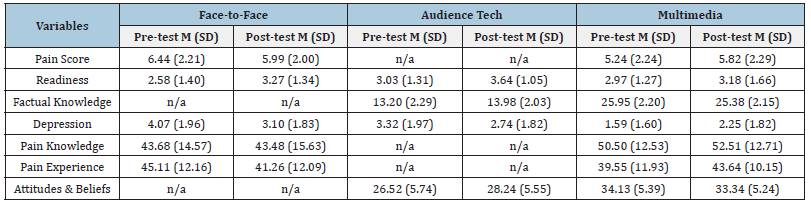
There was no significant interaction effect of “Intervention Arm x Time,” Wilks’ λ=0.743, F(14,134)=1.535, p=0.107, which indicates that the three arms of multimedia were not significantly different on their impact on the dependent measures aforementioned. There was a significant main effect for “Time,” Wilks’ λ=0.726, F(7,67)=3.608, p=0.002, n2=0.274. A significant univariate main effect was obtained for the primary measures of pain intensity (now), F(1,73)=6.272, p=0.014, n2=0.079; but the scores worsened as opposed to improving. There was no significant univariate main effect for readiness to adopt self-management approach, F(1,73)=1.519, p=0.222.
Secondary outcomes
Significant univariate main effects were also obtained for the secondary measures of factual knowledge, F(1,73)=4.868, p=0.031, n2=0.063; and in depression scores, F(1,73)=11.274, p=0.001, n2=0.134. Factual knowledge scores decreased, and depression scores increased, which indicates a significant deterioration in those areas. However, depression scores still remained lower than the >3 threshold on the PHQ-2. There was no significant univariate main effect obtained for the secondary measures of pain knowledge, F(1, 73)=1.683, p=0.199; pain experience, F(1, 73)=2.861, p=0.095; and attitudes or beliefs about pain, F(1, 73)=1.178, p=0.281.
Discussion
Healthcare organizations typically consider the expenses being saved when using multimedia versus face-to-face interventions. These include expenditures, such as medical and resource costs, but also consist of the value of pain, suffering, and the loss in quality of life of Veterans. The use of multimedia in lieu of faceto- face interventions can also reduce costs due to Veterans’ absenteeism and lost workdays [4]. Other perceived advantages of using multimedia include having no time or spatial limits and learning can occur according to individual needs and progress. The current study assessed the effects of multimedia (such as a DVD, a booklet, or both) used in pain education interventions on a wide range of pain measures among Veterans with chronic, noncancer. The findings from the current study did not support the overall hypotheses that the effects from a face-to-face, patient pain education intervention may be translatable into multimedia. In fact, the findings suggest that using multimedia in lieu of face-toface education may be detrimental over time. More specifically, the current findings suggest that the use of multimedia had significant, moderate negative effects on pain scores and factual knowledge, and a large negative effect on depressive symptoms. This is surprising since the materials used are based on an empirically supported, face-to-face intervention that made significant improvements on all the measures used in the current study [18,19]. Please see side-by-side comparisons of the demographics and findings from all three studies in Table 1 & 2. There are several possible general explanations for these findings. Keep in mind that the participants of the current study had first been offered the chance to participate in the face-to-face version of the intervention but were noted being unable to attend due to a conflict in their schedule. It is plausible that these same conflicts may have limited the participants ability to participate in their assigned intervention.
Table 1: Side-by-side comparisons of the demographics from all three studies.
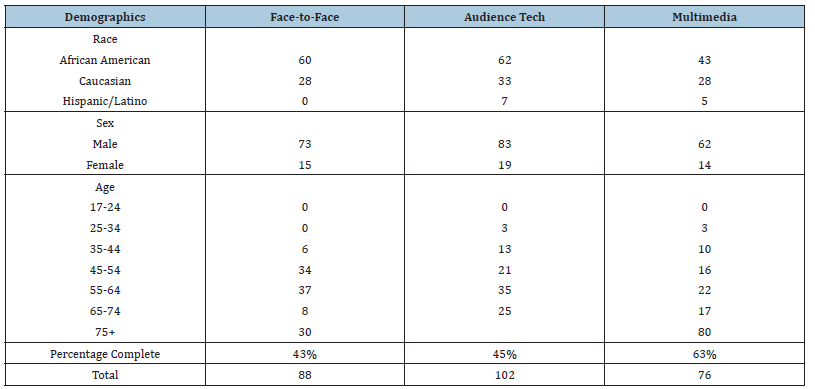
Table 2:Side-by-side comparison of the findings from all three studies.
In addition, we are uncertain whether some of the participants (regardless of intervention arm) may not have read/watched them or immediately discarded them [33]. Past research conducted by the Direct Marketing Association (DMA) has evaluated the effectiveness of patient information leaflets, a basic form of multimedia. According to DMA research, as many as 79% of recipients either keep, pass on to a friend, or glance over the contents of a leaflet distribution item. When these leaflets are directly mailed, they are glanced at by 79% of consumers but only 32% read them properly [34]. Previous studies have also found that patient information leaflets improve patients’ knowledge and adherence to treatment for acute diseases. However, their impact on adherence varies depending on the context, how the patient information leaflets are given, and the invasiveness of the intervention for chronic diseases [35]. It is also unclear whether the patients actually wanted the media (regardless of type) or were more so enticed by the nominal compensation given for research participation. Furthermore, the Internet and streaming services are becoming more important for everybody as it is one of the newest and most forward-facing forms of multimedia. Participants who follow health news regularly may likely have been exposed to inaccurate stories about disease prevention that conflicts with the information the current study disseminated. Furthermore, you can’t binge a painful education program. Pain management is self-management and requires that people who suffer from chronic pain be engaged and participants in their own care to see results.
When in reference to depressive symptoms, the average Veteran did not experience a major depressive episode over the previous two weeks at baseline in the current study. Previous studies used a sample of Veterans who suffered symptoms of depression (Table 2). In addition, the potential for worsened symptoms are considered to be amplified among chronic pain patients over time. Past research has also shown that active information (i.e., participation of subjects in planification of follow-up and consolidation) reduced levels of anxiety and depression, but without reducing the number of cases of depression. In contrast, passive information increased mood symptoms [36]. The current study used more passive information, despite the Veterans having a module (Module #14: Conclusion & Planning) which explained how subjects can be involved in the planification of follow-up and consolidation of modalities into their treatment plan.
Conclusion
The current study underlines the potential negative aspects to using multimedia. Multimedia instructional tools may be confusing, too involving, tiring, and imprecise [37]. Thus, the use of multimedia should not replace any personal interaction from providers and should only be considered to support additional learning. Future studies may want to explore the feasibility of using online learning management systems to implement hybrid learning and/or integrate learning tools. In addition, these systems can be examined to determine their effect on chronic pain scores and other secondary measures.
Acknowledgement
The author would like to thank the Midwest Pain Society for their generous grant support for the current study. The author would also like to thank all the Veterans who made this research possible. The author is thankful for the Jesse Brown VA Medical Center, Anesthesiology/Pain Clinic department for their vision and ongoing support of the Pain Education School program.
References
- Dorflinger L, Kerns RD, Auerbach SM (2013) Providers’ roles in enhancing patients’ adherence to pain self-management. Transl Behav Med 3(1): 39-46.
- Ferrell B, Rhiner M, Ferrell B (1993) Development and implementation of a pain education program. Cancer 72(11): 3426-3432.
- Riddell A, Fitch MI (1997) Patients’ knowledge of and attitudes toward the management of cancer pain. Oncol Nurs Form 24(10): 1775-1784.
- Chen H, Yeh M, Yang H (2005) Testing the impact of a multimedia video CD of patient controlled analgesia on pain knowledge and pain relief in patients receiving surgery. Int J Med Inform 74(6): 437-445.
- Ferrell BR, Borneman T, Juarez G (1998) Integration of pain education in home care. J Palliat Care 14: 62-68.
- Gottlieb BS (1986) Predicting outcome in pain programs: A matter of cognition. Paper Presented at the American Psychological Association Annual Convention, USA.
- Mitchinson A, Kerr E, Krein S (2008) Management of chronic noncancer pain by VA primary care providers: When does pain control a priority? American Journal of Managed Care 14(2): 77-84.
- Gironda R, Clark M, Massengale J, Walker R (2006) Pain among veterans of operations enduring freedom and Iraqi freedom. Pain Med 7(4): 339-343.
- Kerns R, Otis J, Rosenberg R, Reid M (2003) Veterans' reports of pain and associations with ratings of health, health-risk behaviors, affective distress, and use of the healthcare system. J Rehabil Res Dev 40(5): 371-379.
- National Headache Foundation (2013) War veterans’ health resource initiative.
- Yunus M (2012) The prevalence of fibromyalgia in other chronic pain conditions. Pain Res Treat 2012: 584573.
- Drake D, Beckworth W, Brown R, Lennox McNeary, David Cifu, et al. (2006) A profile of patients in a VA pain clinic. Federal Practitioner 23: 15-22.
- Dunphy R, Bridgewater L, Price D, Robinson M, Zeilman C, et al. (2003) Visceral and cutaneous hypersensitivity in Persian gulf war Veterans with chronic gastrointestinal symptoms. Pain 102(1-2): 79-85.
- Engel C, Jaffer A, Adkins J, Riddle J, Gibson R (2004) Can we prevent a second 'Gulf war syndrome'? Population-based healthcare for chronic idiopathic pain and fatigue after war. Adv Psychosom Med 25: 102-122.
- Ford J, Campbell K, Storzbach D, Binder L, Anger W, et al. (2001) Post-traumatic stress symptomatology is associated with unexplained illness attributed to Persian Gulf war military service. Psychosom Med 63(5): 842-849.
- Kinsinger L, Lewis S, Strickland R (2004) Put prevention into VA practice: A step-by-step guide to successful program implementation.
- Cosio D, Hugo E, Roberts S, Schaefer D (2012) A pain education school for veterans with chronic non-cancer pain: Putting prevention into VA practice. Federal Practitioner 29: 23-29.
- Cosio D, Lin E (2013) Effects of a pain education program for veterans with chronic, non-cancer pain: A pilot study. Journal of Pain and Palliative Care Pharmacotherapy 27: 340-349.
- Simmons E, Cosio D, Lin E (2015) Using audience response systems to enhance chronic, non-cancer pain knowledge acquisition among veterans. Telemed J E Health 21(7): 557-563.
- Watson E, Cosio D, Lin E (2014) A mixed-methods approach to veteran satisfaction with pain education. Journal of Rehabilitation Research & Development 51(3): 503-514.
- Watson E, Cosio D, Lin E (2015) Pain education across VA clinics: First study to examine provider satisfaction of a health education program catered to patients who suffer from chronic, non-cancer pain. Practical Pain Management 15(2): 50-58.
- Elander J, Robinson G, Morris J (2011) Randomized trial of a DVD intervention to improve readiness to self-manage joint pain. Pain 152(10): 2333-2341.
- Hill A, McPhail S, Hoffman T, Hill K, Oliver D, et al. (2009) A randomized trial comparing digital video disc with written delivery of falls prevention education for older patients in hospital. J Am Geriatr Soc 57(8): 1458-1463.
- Wilhelm D, Gillen S, Wirnhier H, Schneider A, Schmidt A, et al. (2009). Extended preoperative patient education using a multimedia DVD-Impact on patients receiving a laparoscopic cholecystectomy: A randomized controlled trial. Langen becks Arch Surg 394(2): 227-233.
- Stellefson M, Chaney B, Chaney J (2009) Examining the efficacy of DVD technology compared to print-based material in COPD self-management education of rural patients. California Journal of Health Promotion 7(2): 26-42.
- Capewell C, Gregory W, Closs S, Bennett M (2010) Brief DVD-based educational intervention for patients with cancer pain: Feasibility study. Pallative Medicine 24(6): 616-622.
- Fincham JE (2008) Response rates and responsiveness for surveys, standards and the Journal. Am J Pharm Educ 72(2): 43.
- Shutty M, Degood D (1990) Veteran knowledge and beliefs about pain and its treatment. Rehabil Psychol 35: 43-54.
- Kroenke K, Spitzer R, Williams J (2003) The patient health questionnaire-2: Validity of a two-item depression screener. Med Care 41(11): 1284-1292.
- (2015) GNU PSPP (Version 0.8.5). Free Software Foundation, Maryland, USA.
- Blankers M, Koeter M, Schippers G (2010) Missing data approaches in e health research: Simulation study and a tutorial for non-mathematically inclined researchers. J Med Internet Res12(5): e54.
- Liu-Seifert H, Zhang S, D Souza D (2010) A closer look at the baseline-observation-carried-forward (BOCF). Journal of Patient Preference & Adherence 4: 11-16.
- Grime J, Blenkinsopp A, Raynor DK, Pollock K, Knapp P (2007) The role and value of written information for patients about individual medicines: a systematic review. Health Expect 10(3): 286-298.
- DLM (2014) Leaflet marketing: The good, the facts, the stats.
- Sustersic M, Gauchet A, Foote A, Bosson JL (2017) How best to use and evaluate patient information leaflets given during a consultation: A systematic review of literature reviews. Health Expect 20(4): 531-542.
- Forster A, Brown L, Smith J, House A, Knapp P, et al. (2015) Information provision for stroke patients and their caregivers. Cochrane Database Syst Rev 11(11): CD001919.
- Antonietti A, Giorgetti M (2006) Teachers’ beliefs about learning from multimedia. Computers in Human Behavior 22(2): 267-282.
© 2022 David Cosio. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






