- Submissions

Full Text
Developments in Anaesthetics & Pain Management
Ventricular Arrhythmias During Liver Transplant in a Patient with Prolonged QT Interval
Hussein Sadkhan* and Raed Alkurwi
Department of Anesthesia and Perioperative Medicine, Canada
*Corresponding author: Hussein Sadkhan, Department of Anesthesia and Perioperative Medicine, Canada
Submission:April 18, 2022;Published: April 26, 2022

ISSN: 2640-9399 Volume2 Issue3
Abstract
Cardiac arrhythmias occur commonly during liver transplantation surgery. Certain medications commonly used during liver transplantation can trigger ventricular arrhythmias due to recognized or unrecognized prolongation of the QT interval. We herein present a case report of a patient with QT interval prolongation on preoperative ECG who developed repetitive ventricular arrhythmias during liver transplantation. We will explore anesthesia management and how some medications can contribute to triggering an arrhythmia.
Keywords:Arrhythmia; Intraoperative complications; Liver transplantation
Introduction
Cardiac arrhythmias occur commonly during liver transplantation surgery, and most notably, such events can be due to a patients’ comorbidities, for example, liver cirrhosis. A prolonged QT interval is one of the less well-identified comorbidities in patients with or without liver cirrhosis. Preoperative identification of prolonged QT intervals is an essential and crucial factor to consider in careful monitoring and intraoperative anesthesia management towards prevention and early treatment of complications. Certain medications commonly used during liver transplantation can trigger ventricular arrhythmias due to recognized or unrecognized prolongation of the QT interval. The patient involved in this case report has provided written consent to report this information.
Case Report
A 38-year-old female (height 180cm, weight 84kg) was scheduled for orthotopic liver transplantation due to alcoholic liver cirrhosis. She had a history of end-stage liver disease with MELD score of 21. She presented with hepatic encephalopathy and mild ascites. Her past medical history was otherwise significant for recurrent pancreatitis and previous cholecystectomy. An ECG was performed one month before surgery and demonstrated a prolonged corrected QT (QTc) interval of 490 milliseconds. There was no data about the QT interval before one month compared to the other readings. However, there was no time to investigate and correct this before the surgery. The surgery was on an emergency basis, where this patient had no offer from a living donor. An ECG done immediately preoperatively showed a QTc of 530ms. Preoperative transthoracic echocardiography revealed normal left and right ventricular systolic function and no regional wall motion abnormalities. There was mild pulmonary hypertension. Preoperative sodium was 133mmol/L, potassium was 4.4mmol/L, calcium was 3.36mmol/L, and magnesium was 0.84mmol/L. On entry into the operating room, her vital signs were within normal limits.
General anesthesia was induced with midazolam 2mg, fentanyl 200mcg, lidocaine 60mg, and propofol 100mg IV. Rocuronium was used for muscle relaxation. Isoflurane was used to maintain the anesthesia. Arterial and central venous accesses were established without difficulty. A vasopressin infusion was started at a rate of 2u/hr. The vasopressin infusion is routinely used in our institution during liver transplants as it helps maintain the hemodynamics and reduce portal hypertension. Transesophageal Echocardiography (TEE) probe was inserted. The patient was stable for the first 90 minutes of general anesthesia. At the end of the dissection phase of her liver transplant and approximately 2 hours after the vasopressin infusion had been started, we noted multiple Premature Ventricular Contractions (PVCs) on the monitor screen that progressed to narrow-complex supraventricular tachycardia.
Initially, two boluses of amiodarone 150mg and multiple boluses of esmolol 20mg were administered. A few minutes later, the patient had two polymorphic ventricular tachycardia episodes consistent with Torsade De Pointes (TdP), each lasting 3-5 seconds and terminated spontaneously. The patient was given 4g of IV magnesium sulphate, lidocaine 100mg, and a lidocaine infusion of 2mg/kg/hr. These concomitantly administered drugs ceased the TdP temporarily. After approximately 10 minutes, the patient again had frequent, short, self-terminating episodes of TdP, which were terminated with intermittent doses of 500mg to 1g boluses of IV magnesium. Around fifteen episodes occurred during the transplant, and a total of 12g of magnesium were administered. Although the patient was hypotensive during each episode, her systolic blood pressure remained above 65mmHg, and she did not require cardioversion. The vasopressin infusion continued till the end of surgery. The surgery took around 10 hours, and blood loss was about 2 Liters. After the surgery, the patient was transferred to the Intensive Care Unit (ICU) with continuous lidocaine infusion (60mg/hr). She was hemodynamically stable without any pressors, including vasopressin. Following admission to the ICU, the QT interval started to become less in length, and no TdP occurred postoperatively; however, ICU telemetry was still showing multiple PVCs. The patient stayed in the ICU for five days and then shifted to Multi-Organ Transplants Unit (MOTS) for another five days, then she was discharged home.
Discussion
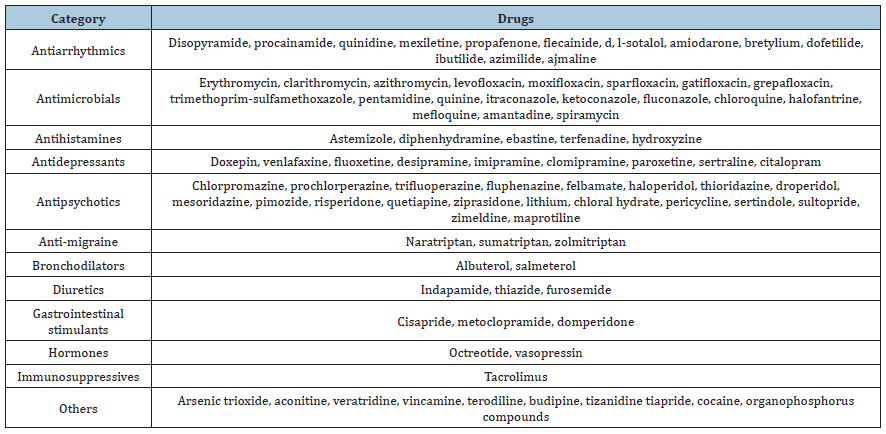
Long QT syndrome (LQTS) results in prolonged ventricular repolarization, characterized by a prolonged QT interval on the Electro Cardio Graphic (ECG). LQTS may be either congenital or acquired. Many factors can potentially prolong the QT interval, including electrolyte abnormalities, myocardial ischemia, alcohol toxicity, and autonomic imbalance with sympathetic nervous system hyperactivity [1]. A prolonged QT interval represents the most common Electro Cardio Graphic (ECG) abnormality in patients with liver cirrhosis [2]. There is an extensive list of drugs that induce QT interval prolongation and can contribute to a higher risk of torsade de points. Table 1 lists some of the most reported drugs [3].
Table 1:Lists some of the most reported drugs [3].
Our patient had multiple intraoperative PVCs and SVT that progressed to polymorphic ventricular tachycardia (TdP). The patient’s preoperative prolonged QT interval was likely secondary to the effect of cirrhosis. The medications used intraoperatively may have prolonged the QTc even further and thus precipitated TdP. Vasopressin is one of the commonly used pressors during liver transplantation in our institution, and that is for its main beneficial effect of reducing blood loss from splanchnic vasoconstriction as well as its role in reducing portal hypertension [4]. The vasopressin infusion may have contributed to the development of torsade de Pointes in this patient with a baseline prolonged QT interval. Amiodarone may also prolong the QT interval, and TdP may occur [5]. Some studies have shown lidocaine to successfully terminate TdP, while other trials and reports have implicated it as an etiologic factor [6]. Hypokalemia, hypocalcemia, and hypomagnesemia can lead to TdP, but our patients’ values were normal.
Magnesium sulphate is the treatment of choice for torsade de points, even if the serum level is normal: an initial bolus of 30mgkg-1 over 2-3min is usually sufficient and should be followed by an infusion at 2-4mgmin-1. The bolus can be repeated after 15min if bursts of TdP persist [7]. However, despite our patient having received the recommended dose, the TdP persisted, and she responded well to higher doses of magnesium.
Considerations during anesthesia for cirrhotic patients with
prolonged QT intervals may include:
1. Optimizing electrolyte balance.
2. Maintaining hemodynamic stability during liver
transplantation surgery.
3. Avoiding drugs that can prolong QT intervals.
We believe the vasopressin may have been the precipitating
factor in this case.
Conclusion
Preoperative recognition of QT interval prolongation and adequate monitoring and management to prevent fatal arrhythmias is essential in liver transplantation patients. However, no cut-offs for the QTc interval exist for determining who can safely go for transplantation. Therefore, the risk-benefit balance of potentially denying transplantation based on a single test parameter must be considered.
Funding Statement
The authors received no financial support for this article’s research authorship and publication.
References
- Shah SR, Park K, Richard Al Weis (2019) Long QT Syndrome: A comprehensive review of the literature and current evidence. Curr Probl Cardiol 44(3): 92-106.
- Day CP, James OF, Butler TJ, Campbell R (1993) QT prolongation and sudden cardiac death in patients with alcoholic liver disease. Lancet 341(8858): 1423-1428.
- Letsas KP, Efremidis M, Filippatos GS, Sideris AM (2007) Drug induced long QT syndrome. Hellenic J Cardiol 48(5): 296-299.
- Mauro VF, Bingle JF, Ginn SM, Jafri FM (1988) Torsade de pointes in a patient receiving intravenous vasopressin. Crit Care Med 16(2): 200-201.
- Di Micoli A, Zambruni A, Bracci E, Benazzi B, Zappoli P, et al. (2009) Torsade de pointes during amiodarone infusion in a cirrhotic woman with a prolonged QT interval. Digestive & Liver Disease 41(7): 535-538.
- Janeiro LF (1995) Torsades de pointes and long QT syndromes. Am Fam Physician 52(5): 1447-1453.
- Tzivoni D, Banai S, Scuger C, Benhorin J, Keren A, et al. (1988) Treatment of torsade de pointes with magnesium sulfate. Circulation 77(2): 392-397.
© 2022 Hussein Sadkhan. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






