- Submissions

Full Text
Developments in Anaesthetics & Pain Management
Provision of Anaesthesia for Shoulder Surgery- A Case Load Analysis
Zhaosheng Jin1,2*, Tim Jackson1,2 and Joanna Umo-Etuk1
1 Barking, Havering and Redbridge NHS trust, UK
2 Central London School of Anaesthesia, UK
*Corresponding author: Zhaosheng Jin, Barking, Havering and Redbridge NHS trust, Central London School of Anaesthesia, UK
Submission: July 23, 2018;Published: August 16, 2018

ISSN: 2640-9399 Volume1 Issue4
Abstract
Over the years a number of techniques have been developed to address the postoperative analgesic requirement in shoulder surgeries. The introduction of catheter based technique for interscalene block now enables longer lasting analgesic effect and is now considered to be the gold standard postoperative analgesia in complex shoulder surgery. However, its use is often limited by the staffing and resources constraints. In this case load analysis, we seek to investigate the anaesthetic practice of our busy district general hospital and how it compares to the gold standard treatment.
Introduction
The shoulder is an anatomically complex joint involving bone, cartilage, capsule, tendon and muscle. Pathology could develop from any of these structure and lead to surgical intervention. In shoulder surgery physiotherapy forms a vital part of the postoperative rehabilitation however it is often limited by significant postoperative pain [1].
More recently a number of techniques have been used to manage the postoperative pain in shoulder surgery, this include intra-Articular local anaesthetics, supraclavicular axillary and interscalene nerve blocks. It has been shown that interscalene and supraclavicular block in shoulder surgery has been associated with significantly reduced Perioperative Opioid requirement and Opioid related adverse effects, as well as significantly faster postoperative recovery [2-5]. However, the limitation of such technique is the relatively short duration of its analgesic effect.
The development of the catheter based technique for the interscalene block now allows for continuous administration of local anaesthetic agent and as a consequence, a significantly longer analgesic duration. In a number of clinical trials and metaanalysis, interscalene catheter technique has been demonstrated to have significantly better analgesic effect than single interscalene injection [6,7]. It is considered to be the gold standard in terms of Perioperative analgesia for complex shoulder surgery. However, due to the higher skill requirement for insertion of the catheter, as well as need for 24-hours-a-day follow up service, its use is not widely implemented. In this case load analysis, we will investigate how the resources and anaesthetic practice of our high throughput, publically funded district general hospital compare to the gold standard treatment.
Methods
This is a retrospective case load analysis of shoulder surgeries done over a two month period. The inclusion criteria are all adult major shoulder surgeries, which included Subacromial decompression; Rotator cuff repair; Shoulder replacements; Acromioclavicular joint resection. The data collection process is authorised by the hospital clinical audit department, all case details are anonymised, the case list and the corresponding medical notes were obtained from the hospital records department. According to a pre-designed Proforma, patients’ medical histories, surgical, anaesthetic and recovery (Post-anaesthesia care unit) records were reviewed; information regarding the type of surgery, anaesthetic modality, nerve block technique employed and Perioperative Opioid use were collected. The Opioid doses were all converted to equivalent morphine dose using the Opioid equivalency chart [8]. The Perioperative Opioid dosages of the different cohorts were compared using the unpaired T-test. The correlation between the volume/ total dose of local anaesthetic used for the nerve block, and the Perioperative Opioid dosages were tested using the spearman’s rank correlation coefficient.
Results
A total of 36 cases were identified and 33 sets of case notes were successfully retrieved. Of the 31 analysed cases, 28 cases were done under GA with single shot nerve block, 3 were done under GA without nerve block. Of the 28 surgeries with nerve block, 24 were done with interscalene block and 4 with supraclavicular block (Figure 1). In all cases the choice of local anaesthetic agent was Bupivacaine, however we noticed wide range of local anaesthetic concentration by the anaesthetists responsible (0.25%, 0.375% or 0.5%) and total local anaesthetic volume (7ml to 25ml) were administered for the nerve block.
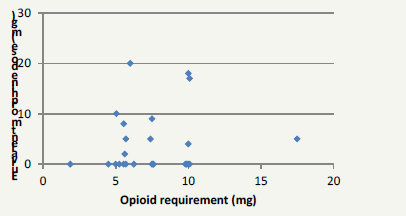
Compared to surgeries with nerve block, those without were associated with significantly higher Perioperative Opioid requirement (4.2mg vs 22.3mg respectively, P< 0.05, (Figure 2). Interestingly, there was considerable variation in the Perioperative Opioid requirement amongst patients who had the surgery with nerve block (Figure 3). The different local anaesthetic concentration was not associated with significant difference in the Perioperative Opioid requirement. The Perioperative Opioid requirement did not correlate with the volume of local anaesthetic used or the total dose of anaesthetic used (Figure 4).
Figure 1:Mode of anaesthesia
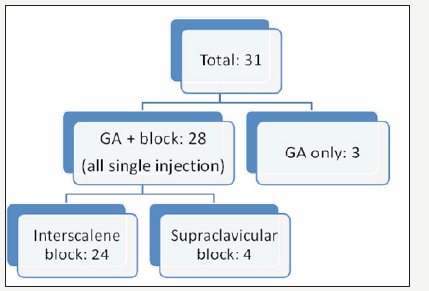
Figure 2: Perioperative Opioid requirement in cases with nerve blocks and cases with General anaesthetics (GA) only
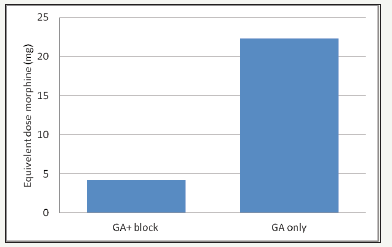
Figure 3:Box and whisker diagram of the Perioperative Opioid dosage in cases done with nerve blocks. Median=0, Q1=0, Q3=8, Range=0-20 mg.
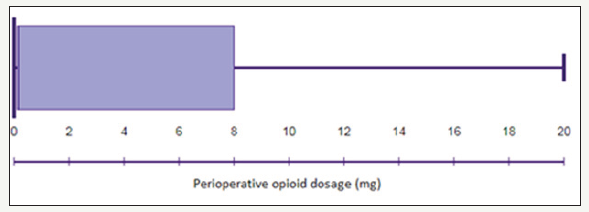
Figure 4: Local anaesthetic agent dose vs Perioperative Opioid requirement, R=0.13, very weak correlation.
Discussion
From our case analysis, over 90% of the shoulder surgeries were done with regional anaesthesia cover. Similar to most literature findings, cases done without regional anaesthesia were associated with significantly higher Opioid requirement. Cases done with regional anaesthesia had considerable variation in the Opioid requirement, with over half needing no Perioperative opioids, and 10% of the cases needing more than 15mg morphine or equivalent. This did not seem to be correlated with the volume or total dose of the local anaesthetics agent used for the nerve block. This could represent a combination of surgical and patient factors, but may also be due to ineffective block done by infrequent practitioners or by junior anaesthetists. As part of our quality improvement process, we will be proposing the need of a daily ‘duty regional Anaesthetist who is experienced in supervising trainees as well as assisting the occasional practitioner (replacing the routine anaesthetist). We hope this practice will improve the overall regional anaesthesia efficacy of the department.
Although continuous catheter based nerve block has been shown to provide significantly longer lasting analgesia and with minimal risks, it is unfortunately difficult to implement at a publically funded district general hospital due to a number of considerations. Staff, require training in safely using the catheter technique; the appropriate equipment, including the local anaesthetic pump need to be procured and funded; most importantly, there will need to be trained staff available 24 hours a day to review patients with nerve block catheters and make decisions about its management. These presents a number of financial, as well as administrative obstacles to the implementations of catheter based nerve block. While continuous catheter based nerve block is clinically superior, it’s likely that more cost effectiveness analysis are needed before it could be widely implemented in National Health Service (NHS) funded institutions.
References
- Beecroft cl, Syuk Doahams, Coventry dm, syuk doahams (2018) Anaesthesia for shoulder surgery. Continuing Education in Anaesthesia Critical Care & Pain 8(6): 193-198.
- Yan S, Zhao Y, Zhang H (2018) Efficacy and safety of interscalene block combined with general Anesthesia for arthroscopic shoulder surgery: A meta-analysis. J Clin Anesth 47: 74-79.
- Guo CW, Ma JX, Ma XL, Lu B, Wang Y, et al. (2017) Supraclavicular block versus interscalene brachial plexus block for shoulder surgery: A metaanalysis of clinical control trials. Int J Surg 45: 85-91.
- Bosco L, Zhou C, Murdoch JAC, Bicknell R, Hopman WM, et al. (2017) Pre or postoperative interscalene block and/or general Anesthesia for arthroscopic shoulder surgery: a retrospective observational study. Can J Anaesth 64(10): 1048-1058.
- Lehmann LJ, Loosen G, Weiss C, Schmittner MD (2015) Interscalene plexus block versus general anaesthesia for shoulder surgery: a randomized controlled study. Eur J Orthop Surg Traumatol 25(2): 255- 261.
- Kim JH, Koh HJ, Kim DK, Lee HJ, Kwon KH, et al. (2018) Interscalene brachial plexus bolus block versus patient-controlled interscalene indwelling catheter analgesia for the first 48 hours after arthroscopic rotator cuff repair. J Shoulder Elbow Surg 27(7): 1243-1250.
- Vorobeichik L, Brull R, Bowry R, Laffey JG, Abdallah FW (2018) Should continuous rather than single-injection interscalene block be routinely offered for major shoulder surgery? A meta-analysis of the analgesic and side-effects profiles. Br J Anaesth 120(4): 679-692.
- Committee PT (2009) Opiate equianalgesic dosing chart. University of North Carolina Hospitals, USA.
© 2018 Zhaosheng Jin. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






