- Submissions

Full Text
Developments in Anaesthetics and Pain Management
Nutritional Support in Children with Chronic Kidney Disease
Ebru Canakci1*, Ahmet Karatas2 and Cagri Akalin3
1Department of Anesthesiology and Reanimation Ordu University ,School of Medicine ,Turkey
2Department of Internal Medicine,Division of Nephrology, Ordu University ,School of Medicine ,Turkey
3Department of General Surgery Ordu University ,School of Medicine ,Turkey
*Corresponding author: Ebru Canakci, Department of Anesthesiology and Reanimation, Turkey
Submission: May 11, 2018;Published: May 31, 2018

ISSN 2640-9399 Volume1 Issue3
Abstract
Chronic kidney disease (CKD) is an important cause of morbidity and mortality in children. Children with CKD are considered at high risk for proteinenergy malnutrition. The children on dialysis, especially those on chronic ambulatory peritoneal dialysis (CAPD), need a higher protein intake. Growth and development retardation occur in 36% of the children with CKD. Diet therapy is very important during infancy when nutritional requirements and growth rate are very high. It is considered that the outcomes of chronic kidney disease (CKD) during childhood could significantly affect nutritional status and that it would usually cause the growth rate to decrease. Continuous muscle protein metabolism in CKD leads to the loss of muscle proteins. Protein intake should be sufficient so that it provides growth and development and preserves positive nitrogen balance and also 60-70% of it should be of high biological value. As a result nutritional support in children with CKD is very important. Children with CKD should be directed to dietitian support. Nutritional support should be in the light of scientific guidelines.
Keyword: Pediatric Chronic Kidney Disease; Malnutrition; Protein Energy Wasting
Abbreviations: CAPD: Chronic Ambulatory Peritoneal Dialysis; CKD: Chronic Kidney Disease; BMI: Body Mass Index; UPS: Ubiquitin Proteasome System; DRI: Dietary Reference Intake
Introduction
CKD is an important cause of morbidity and mortality in children [1]. Children with CKD are considered at high risk for protein-energy malnutrition. Their daily calorie and protein requirements should be met from the nutrients with high biological value. The children on dialysis, especially those on chronic ambulatory peritoneal dialysis (CAPD), need a higher protein intake. It is difficult to ensure this when anorexia is superimposed on the catabolic response resulting from the uremic condition of the child. In developed countries, when oral feeding is inadequate, it can be provided via the percutaneous entero-gastrostomy stoma for this feeding infusion [1].
Growth and development retardation occur in 36% of the children with CKD [2]. Hormonal dysregulation, especially the change in the release of growth hormone, insulin, leptin, ghrelin, and other inflammatory cytokines generate the mechanisms effective in growth retardation and cachexia. In conclusion, the potent catabolism created by these hormones and cytokines is difficult to challenge for both the patient and healthcare team. Diet therapy is very important during infancy when nutritional requirements and growth rate are very high [3,4].
It is considered that the outcomes of chronic kidney disease (CKD) during childhood could significantly affect nutritional status and that it would usually cause the growth rate to decrease [5]. The protein-energy loss secondary to metabolic and hormonal imbalances is associated with the increased morbidity and mortality in children with CKD [5]. The diagnostic and prognostic accuracy of the biochemical markers for the assessment of malnutrition is weak compared to the anthropometric measurements. Body mass index (BMI) is accepted as a prognostic indicator of mortality for the children with CKD as well as adults [5]. However, the validity of BMI and other anthropometric measurements is discussed to a great extent, because CKD is associated with the imbalances of hydration status [5].
The loss of cellular protein increases morbidity and mortality in the children with CKD. In this case, the questions of “How does the protein loss takes place?” and “What is the precaution?” come to mind. Metabolic acidosis, impaired insulin/IGF-1 signaling, inflammation, defective hypothalamic appetite regulation are the factors responsible for the synthesis and break-down of micro RNA cellular protein [6].
Continuous muscle protein metabolism in CKD leads to the loss of muscle proteins. The catabolic pathways causing protein wasting include the ubiquitin-proteasome system (UPS), caspase-3 lysozymes, myostatin activation and Stat -3 inhibition. These pathways stimulate the cellular signaling pathways activating myostatin which accelerates the metabolic acidosis, defective insulin signaling, inflammation, UPS-mediated catabolism.The inhibition of this pathway can prevent the loss of muscle proteins. Myostatin inhibition may provide new treatment directions to prevent the muscle protein waste in CKD or disorders associated with its complications [6].
Height-for-age index (=Z score) is an indicator of linear growth retardation and long-term nutritional deficiency among children. Height Z score demonstrated significant positive correlation with energy intake whereas protein intake showed a positive correlation with BUN and a significant negative correlation with serum bicarbonate [7].
According to the NKF-KDOQI guidelines, an height-for-age value below the standard deviation of -1.88 or third percentile indicates the growth retardation with a level of evidence. The same guideline recommends the use of recombinant growth hormone in order to improve the short stature and to ensure proper growth for the patients who have the lowest limit of serum bicarbonate (22 mmol / L), who are between Grade 2 and 5 and who are not responsive to nutritional support and control of metabolic abnormalities for at least three months.
Protein intake should be sufficient so that it provides growth and development and preserves positive nitrogen balance and also 60-70% of it should be of high biological value. According to the NKF-KDOQI guideline, 100% dietary reference intake (DRI) should be provided for the children on hemodialysis plus an additional 0.1 g / kg /day should be added for losses during dialysis whereas 100% dietary reference intake (DRI) should be provided for the children on peritoneal dialysis and additionally, 0.15-0.3 g/kg/day should be added according to their chronological age for peritoneal losses. One hundred percent of the DRI’s recommended for healthy children should be provided in diet including thiamine, riboflavin, niacin, pantothenic acid, pyridoxine, biotin, cobalamin, vitamin C, retinol, α-tocopherol, vitamin K, folic acid, copper, zinc, and iron [8]. The macro-nutrient distribution of the energy source is demonstrated (Table 1) [6].
Table 1: Distribution of the Energy to Macro-Nutrients in the Children and Adolescents with CKD.
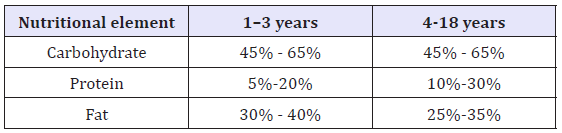
*Adapted from the source of K/DOQI clinical practice guidelines.
The daily fluid requirement in children with CKD should be calculated by taking the fluid excreted via urine and other losses into account. If there is oliguria or anemia in children, the fluid requirement must be calculated according to the following formulas:
Anuria: 24 x 0.5 x kg Oliguria: (24 x 0.5 x kg) + the urine amount excreted one day ago [7]. The requirement for the children and adolescents after transplantation is not different from that of the healthy children and adolescents. There is no need for multivitamin supplementation after a successful transplantation [7]. Intradialytic nutrition is recommended for the children on hemodialysis, those who cannot meet their requirements from oral or enteral nutrition, and when their BMI is below the 5th percentile according to their height-for-age. Two issues to be paid attention during intradialytic nutrition are hyperglycemia and hyperlipidemia. When hyperglycemia develops (blood glucose above 350 mg/ dL), glucose concentration should be reduced and insulin should be added. If hyperlipidemia is detected, lipid support should be discontinued [9]. As a result nutritional support in children with CKD is very important. Children with CKD should be directed to dietitian support. Nutritional support should be in the light of scientific guidelines.
References
- Col M Kanitkar (2009) Chronic Kidney Disease in Children: An Indian Perspective. Med J Armed Forces India 65(1): 45-49.
- Hussain F, Castledine C, van Schalkwyk D, Sinha MD, Lewis M, et al. (2010) UK Renal Registry 12th Annual Report chapter 15: clinical haematological and biochemical parameters in patients receiving renal replacement therapy in paediatric centres in the UK in 2008: national and centrespecific analyses. Nephron Clin Pract 115 (Suppl 1): 289-308.
- Mekahli D, Shaw V, Ledermann SE, Rees L (2010) Long term outcome of infants with severe chronic kidney disease. Clin J Am Soc Nephrol 5(1): 10-17.
- Fine RN (2010) Etiology and treatment of growth retardation in children with chronic kidney disease and end stage renal disease: a historical perspective. Pediatr Nephrol 25(4): 725- 732.
- Apostolou A, Printza N, Karagiozoglou Lampoudi T, Dotis J, Papachristou F (2014) Nutrition assessment of children with advanced stages of chronic kidney disease A single center study 18(3): 212-216
- Wang XH, Mitch WE (2007) Mechanisms of muscle wasting in chronic kidney disease. Nat Rev Nephrol Sep 10(9):504-516
- Rees L, Shaw V (2007) Nutrition in children with CRF and on dialysis. Pediatr Nephrol 22(10): 1689-1702.
- Haffner D, Schaefer F, Nissel R, Wühl E, Tönshoff B, et al. (2000) Effect of growth hormone treatment on the adult height of children with chronic renal failure. German Study Group for Growth Hormone Treatment in Chronic Renal Failure. N Engl J Med 343(13): 923-930
- Köksal G, Gökmen H (2000) Nutritional therapy in kidney disorders. In: Köksal G (eds.) Çocuk Hastalıklarında Beslenme Tedavisi. Baskı Ankara: Hatipoğlu Yayınları, pp. 679-703
© 2018 Ebru Canakci. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






