- Submissions

Full Text
Developments in Anaesthetics and Pain Management
Comparison of Caudal Administration of Bupivacaine, Bupivacaine with Fentanyl and Bupivacaine with Tramadol for Post Operative Analgesia in Children.
Pavithra V1*, Monal Ramani2, Pratham Bysani3 and Deepti Srinivas4
1Dept of Anesthesiology, MS Ramaiah Medical College, India
2Department of Anesthesiology, BJ Medical College, India
3BMCRI, India
4NIMHANS, India
*Corresponding author: Pavithra V, Department of Anaesthesiology, BJ Medical College, Ahmedabad, India
Submission: April 06, 2018;Published: May 17, 2018

ISSN 2640-9399 Volume1 Issue3
Abstract
Objective: To compare the effectiveness of caudal bupivacaine, bupivacaine plus fentanyl and bupivacaine plus tramadol for post operative analgesia in children.
Materials and Methods: The study was conducted on 75 children of ASA I and II physical status aged 1 to 12 years undergoing elective infraumbilical surgeries. Patients were divided into 3 groups and the following were given in the caudal epidural space after the induction of anesthesia:
a. Group I: 0.125% Inj. Bupivacaine 1 ml/kg
b. Group II: 0.125 Inj. Bupivacaine 1 ml/kg plus Inj. Fentanyl 1 mcg/kg
c. Group III: 0.125% Inj. Bupivacaine 1 ml/kg plus Inj. Tramadol 2 mg/kg
Results: Group III had a lower pain score, prolonged mean duration of analgesia, less requirement for rescue analgesics compared to the other two groups.
Conclusion: Addition of Tramadol to Bupivacaine provides prolonged and good quality post operative analgesia in comparison with Bupivacaine alone or with Fentanyl in Caudal Block in the post operative period.
Keyword: Caudal; Bupivacaine; Fentanyl; Tramadol; Pediatric; Analgesia; Haemodymamic; Anesthesiologist; Infraumbilical; Glycopyrrolate; Capnography; postoperative analgesia; Enantiomer; Infraumbilical surgeries; Norepinephrine; Pethidine; Ropivacaine; Midazolam; Glycopyrrolate; Sevoflurane; Opioid receptors; Atracurium; Substantialgelatinous; fluctuation
Abbreviations: ASA: American Society of Anesthesiologist; ECG: electrocardiogram; NIBP: Non Invasive Blood Pressure; MOP: Modified Objective Pain Score.
Introduction
Postoperative analgesia through the caudal epidural route with bupivacaine in children is firmly established in infra umbilical surgery [1,2] The mean duration of surgical analgesia provided by bupivacaine is limited [3] Different drugs such as tramadol, fentanyl, clonidine, and midazolam with bupivacaine prolong the postoperative analgesia. Tramadol is a centrally acting analgesic effect via Opioid receptors [4]. The main site of action of epidural administered fentanyl is the substantial gelatinise on the dorsal horn of spinal cord [5]. We evaluated the duration of postoperative analgesia, intraoperative hemodynamic changes, sedation score and any side effect while using caudal block with bupivacaine, tramadol and fentanyl in paediatric patients undergoing infraumbilical surgeries
Aims and Objectives
- To compare the duration of post operative analgesia.
- To evaluate the effect on haemodymamic changes in the intra operative and post operative period.
- To study the perioperative complications.
- To compare the total number of rescue analgesics used during the 24 hour post operative period in each group.
Material and Methods
After obtaining Institutional Ethical Committee approval, written and informed consent were obtained from parents. This is a prospective, randomized, controlled, single-blind study. We recruited 75 children of either sex with American Society of Anesthesiologist (ASA) physical status I and II, aged 1-12 years, weighing 5-30 kg who were scheduled for elective infra umbilical surgeries of similar duration under general anaesthesia. Patients are having a local infection at the caudal site, neurological disorder, the history of allergic reaction to local anaesthetics, sacral/ vertebral abnormalities, and bleeding diathesis were excluded from the study.
An intravenous access was secured, and glycopyrrolate injection (0.004mg/kg) and ondansetron injection (0.15mg/kg) were administered. Standard monitoring including an electrocardiogram (ECG), non invasive blood pressure (NIBP) measurement, pulse oximetry, capnography, and temperature were applied. All patients were induced with either inhalational agent sevoflurane (1-6%) with 50% nitrous oxide in oxygen. In the left lateral position, caudal block was performed using 22-gauge epidural needle under complete aseptic precautions. After confirmation and negative aspiration for blood and cerebrospinal fluid, the drugs (bupivacaine/tramadol/fentanyl) were introduced into the caudal space slowly with continuous ECG monitoring.
- Figure 1
- Patients were randomly allocated into 3 groups and the following drug was administered caudally:
- Group 1: Inj.Bupivacaine 0.125% 1ml/kg
- Group 2: Inj.Bupivacaine 0.125% 1ml/kg + Inj .Fentanyl 1 mcg/kg
- Group 3: Inj.Bupivacaine 0.125% 1ml/kg + Inj. Tramadol 2 mg/kg
- HR, BP and SpO2 were recorded before induction, 5 minutes after caudal analgesia and every 15 minutes during the surgery.
- At the completion of surgery, patients were extubated and were observed for 2 hours in the recovery room for vitals.
- The following parameters were noted for:
- Post operative pain assessed at 30mins, 2 hours, 4,8,12,24 hours after recovery from anesthesia using Modified objective pain score (MOPS).
- Time at which post operative rescue analgesia was first received and the number were noted
- Sedation score at 1hr and 4 hours after recovery from analgesia using objective score based on the eye opening.
- Incidence of adverse effects was evaluated.
The anaesthesiologist performing the caudal block was blinded to the identity of the drug used. The patients were repositioned supine. This was followed by insertion of Igel. Intraoperative, no analgesic was supplemented. Anaesthesia was maintained with assisted ventilation using sevoflurane initially with 2% and then after decreasing up to 0.6% with hemodynamic stability or controlled ventilation using injection Atracurium (0.5mg/kg) with 50% nitrous oxide in oxygen and sevoflurane decreases up to 0.6% with hemodynamic stability. Glucose/saline solution was infused as per requirement, and perioperative blood loss was replaced as per requirement.
During surgery, adequate analgesia was assessed by hemodynamic stability, as indicated an increase in heart rate and systolic blood pressure of no more than 15% compared with baseline values obtained just before the surgical incision with decreased requirement of sevoflurane concentration, at approximately 0.6%. An increase in heart rate and systolic blood pressure within 20min of skin incision indicated failure of caudal anaesthesia. At the end of surgery, the residual neuromuscular block was antagonized with glycopyrrolate injection 0.008mg/kg and neostigmine injection 0.05mg/kg intravenously. Intraoperative required concentration of sevoflurane was recorded at every 15 min. Heart rate, NIBP, SpO2, EtCO2, and temperature were recorded at every 15min interval till the end of surgery and every hourly interval postoperatively till rescue analgesic was given. Duration of surgery, duration of anaesthesia, and perioperative complications such as brady/tachycardia, hypo/hypertension, vomiting, and urinary retention were recorded.
In the recovery room, hemodynamic parameters, sedation, and pain score were recorded at hourly interval till rescue analgesic was given. Postoperative sedation was assessed by using four point sedation score (0 - spontaneous eye opening, 1 - eye open on speech, 2 - eye open on shake, 3 - unarousable), and pain was evaluated by using FLACC (F=Face, L=Leg, A=Activity, C=Cry, C=Consolability), score (maximum score of 10) at 1h interval for first 3h and thereafter every 2h interval till score >4, and rescue analgesic was given. The use of FLACC is a valid and reliable tool for assessing procedural pain in children aged 5-16 years [6-8]. The Collected data were presented as a mean ± standard deviation, numbers, and percentages as appropriate. A value of P<0.05 was considered as a statistically significant difference with ANOVA being done for statistical analysis among the 3 groups, a student test for analgesics between any 2 out of 3 groups for various parameters and chi square test for complications.
Observation & Results
- INTRA OP PULSE RATE: Remained stable without any significant fluctuation in all three groups
- POST OPERATIVE MOP (modified objective pain score) SCORE: Significant difference was seen among Group 3 and the other groups
- Group 3 shows a significant difference for FIRST RESCUE ANALGESIC & MEAN DURATION OF ANALGESIA with the least no. of rescue analgesics than the other groups
- ONSET OF PAIN is seen in between 8-12 hrs in Group 3 as against 4-8 hrs in the other groups
- MEAN SEDATION SCORE is on higher side at 4-8 hrs postoperatively than other groups
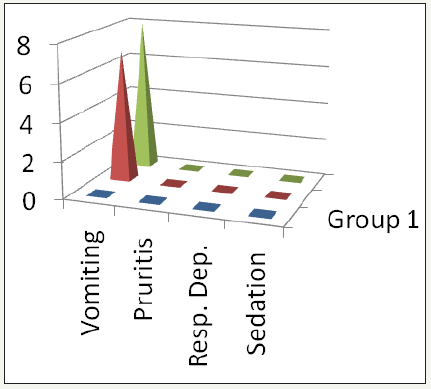
- Among post complications, vomiting was 32% in Group 3, 28% in Group 2 & 0% in Group 1
(Figure 1 to 6 & Table 1)
Figure 1:
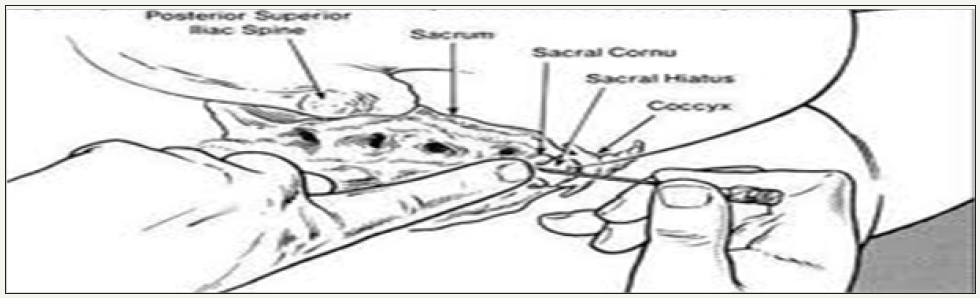
Table 1:
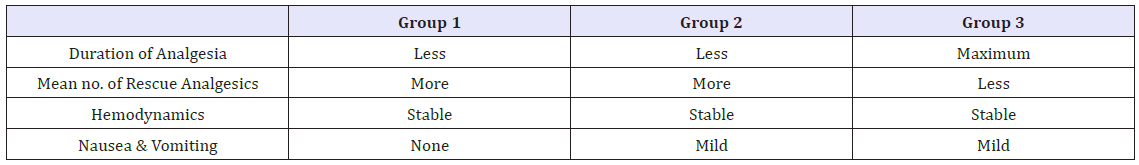
Figure 2:
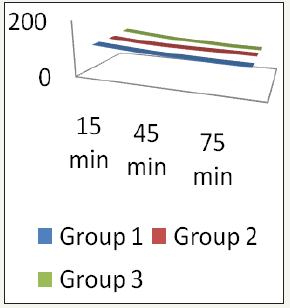
Figure 3:
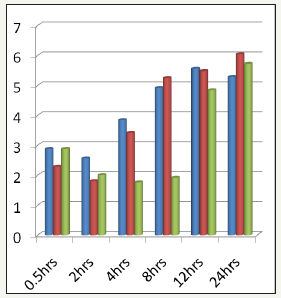
Figure 4:

Figure 5:
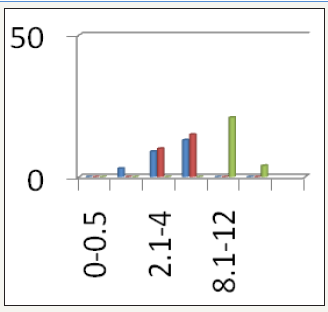
Figure 6:
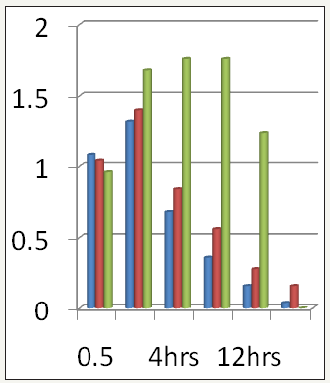
Figure 7:
Discussion
Pain after surgery is inevitable, and the relief of postoperative pain has been consistently and systematically inadequate. A caudal block is one of the common regional aesthetic techniques used in paediatric age group undergoing infraumbilical surgery [6]. It is generally considered a simple, safe procedure with more reliability, and predictability of the cephalic spread of local aesthetic solution in children than in adults. It produces minimal hemodynamic changes and provides some pain-free period intraoperative and postoperatively in infraumbilical surgeries in children [1,2,9].
Analgesic effect of caudal bupivacaine terminates early, and supplementary analgesics are required in the postoperative period. Various adjuvant drugs such as ketamine, midazolam, tramadol, fentanyl, clonidine, dexmedetomidine have been used to prolong the duration of analgesia for the caudal block [1,10]. In our study, single shot caudal epidural using 1 ml/kg of 0.25% bupivacaine with 2 mg/kg tramadol or 2μg/kg fentanyl with a maximum volume of 12 ml were given. Tramadol is a racemic mixture of two Enantiomer. The (+) Enantiomer has moderate affinity for the Opioid μ receptor, which is greater than that of the (−) Enantiomer. In addition, the (+) Enantiomer inhibits serotonin reuptake, and the (−) Enantiomer is a norepinephrine reuptake inhibitor. These complementary properties result in a synergistic antinociceptive interaction between the two. The resulting Opioid has a striking lack of respiratory depressant effect despite having analgesic potency approximately equal to that of pethidine [3] (Figure 7).
Fentanyl is a synthetic Opioid agonist. It exerts its analgesic action by binding to mu receptor, as well as to kappa and delta receptors within the spinal cord, producing spinal analgesia. It easily crosses the lumbar dura and penetrates quickly the lipid phase of the underlying tissue of the cord with minimal migration of opioids in rostral direction, hence, avoiding central nervous system depression of respiratory and cardiovascular system [1,11]. Caudal bupivacaine with tramadol 1 mg/kg provides prolonged, and good quality postoperative analgesia compared to plain bupivacaine in children [10-13]. Caudal tramadol 2 mg/kg with 0.5 mg/kg of 0.25% bupivacaine provided longer duration of postoperative analgesia up to 16 or 18 h without having significant side effects but with higher sedation score for 1h postoperatively [4]. Similarly in our study, the duration of postoperative analgesia was more than 10 h up to 18 h without significant side effects in caudal bupivacaine 0.25% 1ml/kg with tramadol 2mg/kg. Greater epidural use of tramadol 2mg/kg may be preferred to morphine 0.1mg/kg for postoperative analgesia in children undergoing urological surgery without any significant side effects [14].
Caudal tramadol 2 mg/kg combined with bupivacaine 0.25% 0.75 ml/kg provided longer duration of postoperative analgesia and reduced requirement for rescue analgesic compared with tramadol 1mg/kg or 1.5mg/kg in children undergoing inguinal herniotomy [15]. El Hamamsy et al. [3] observed analgesia for up to 4.5 and 5h with caudal fentanyl 2μg/kg and tramadol 2mg/kg, respectively. The mean duration of surgery was 140min. They also observed that if the period of time between performing the caudal injection and recovery of the child from anesthesia was <2h, the incidence of immediate pain (requiring rescue analgesia) was high (30%), demonstrating a slow onset of action of caudal tramadol. However, with a longer duration surgery, caudal tramadol produced good quality analgesia for an average of 10.7h. The slow onset of action of caudal tramadol may imply that there is little advantage in injecting tramadol into the extramural space. Bupivacaine tramadol may prove more useful in young children and infants than other opioids because of its lack of respiratory depressant effects. A bupivacaine-fentanyl mixture as a single caudal epidural injection does not change the onset, quality and duration of analgesia and sedation score [3].
We observed analgesia for up to 11h and 18h with caudal fentanyl 2μg/kg and tramadol 2mg/kg, respectively. The time for onset of analgesia in both groups was respectively same. Prosser et al. [16] observed no significant effects of tramadol on prolongation of analgesic effects of bupivacaine when administered caudally after hypospadias surgery. Cook & Doyle [17] concluded that the addition of caudal fentanyl to local anaesthetics offered no advantage over the administration of local anaesthetics alone for short surgical procedures in children Doctor et al. [18] mentioned that addition of fentanyl 1 μg/kg to ropivacaine or bupivacaine administered through the caudal epidural route imparts no added advantage to bupivacaine except a less intense motor block in children undergoing surgery below the umbilicus. Kawaraguchi et al. [19] concluded that the addition of fentanyl 1mg/kg to ropivacaine 0.2% for caudal analgesia provides no further analgesic advantages to ropivacaine. Shukla et al. [5] observed a transient decrease of oxygen saturation to 91% in five cases and vomiting in eight patients out of 45 who received fentanyl 1 μg/kg with ropivacaine caudally. Patel [2] mentioned in his case series that fentanyl does not prolong the duration of analgesia but significantly increases the incidence of nausea and vomiting.
El Hamamsy et al. [3] observed that caudal fentanyl 2μg/kg produced useful analgesia for up to 4.5 h. However, the addition of fentanyl to local anaesthetics increased significantly the incidence of vomiting and desaturation compared with other groups who did not receive fentanyl. In our study, we observed that caudal fentanyl 2 μg/kg prolong the duration of analgesia with mild sedation in an immediate postoperative period without any side effects. Khalid mentioned postoperative analgesia up to 16 ± 4h with increased incidence of vomiting with tramadol 2 mg/kg [12]. Demiraran et al. reported statistically higher sedation scores in the morphine group compared with the tramadol group. The incidence of nausea and vomiting was 25% in the tramadol group [14]. Prakash et al. [15] concluded that the most frequently reported side effect of epidural tramadol is nausea. The longer time to first void in patients receiving tramadol 2mg/kg though statistically significant appears clinically acceptable. None of the patients required bladder catheterization [15]. In a study done by Prosser et al. [16], 35-40% patient required a urinary catheter in bupivacaine and tramadol groups. According to them first indication for additional analgesia was related to the acute attack of bladder spasm [16].
In our study, nausea and vomiting were observed in four patients of Group BT, and respiratory depression and pruritus were not observed in any patients of both the groups. About 70-75% patients in both groups were catheterized intraoperative. Remaining patients did not have a problem to void urine postoperatively. The addition of caudal epidural analgesia to general anaesthesia inhibits the stress responses from the lower part of the body during surgery and reduces the neuro hormonal responses. It was demonstrated that small doses of a mixture of bupivacaine 0.25% alone or with fentanyl 1μg/kg when administered through the caudal epidural does not have any beneficial effect on pain scores and catecholamine levels [20,21]. In our study intraoperative, there was a decrease in the heart rate and systolic blood pressure and decreases the requirement of end tidal sevoflurane concentration in both the groups.
Conclusion
It can be concluded that the addition of Tramadol 2mg/kg to Bupivacaine 0.125% 1ml/kg resulted in prolonged duration of analgesia in comparison to Bupivacaine alone or with Fentanyl 1mcg/kg in Caudal Block in the post operative period.
References
- Acharya R, Jena SK, Samal S, Mishra SN (2013) Postoperative analgesia in pediatrics patients through caudal block with bupivacaine and two different doses of fentanyl a comparative study. J Evol Med Dent Sci 2(39): 7568-7574.
- Patel D (2006) Epidural analgesia for children. Contin Educ Anesth Crit Care Pain 6(2): 63-66.
- El Hamamsy M, AbdElrahman A, AbdElazizEssa M, Zakaria D (2008) Prolongation of caudal analgesia in pediatric surgery: Comparison between dexmedetomidine, clonidine, tramadol, and fentanyl. Kasr EL Einy Med J 14: 1-10.
- Samad R, Shah TH (2013) Comparison of caudal tramadol bupivacaine and ketamine bupivacaine for postoperative analgesia in children. J Surg Pak Int 18: 54-58.
- Shukla U, Prabhakar T, Malhotra K (2011) Postoperative analgesia in children when using clonidine or fentanyl with ropivacaine given caudally. J Anesthesiol Clin Pharmacol 27(2): 205-210.
- Nilsson S, Finnström B, Kokinsky E (2008) The FLACC behavioral scale for procedural pain assessment in children aged 5-16 years. Paediatr Anesth 18(8): 767-774.
- Turan G, Yuksel G, Ormancý F (2012) Preemptive analgesia with paracetamol and tramadol in pediatric adenotonsillecto. J Anesth Clin Res 3: 8.
- Beyaz SG (2011) Comparison of postoperative analgesic efficacy of caudal block versus dorsal penile nerve block with levobupivacaine for circumcision in children. Korean J Pain 24(1): 31-35.
- Ahmad S, Mohammad K, Ahmed M, Nazir I, Ommid M, et al. (2012) caudal analgesia in pediatric patients: Comparison between bupivacaine and ropivacaine. Internet J Anaesthesiol 30: 3.
- Yasser M, Khairat M (2004) A comparison of caudally administered single dose bupivacaine and bupivacaine tramadol combination for postoperative analgesia in children. JK Sci 6: 19-22.
- Campbell FA, Yentis SM, Fear DW, Bissonnette B (1992) Analgesic efficacy and safety of a caudal bupivacaine fentanyl mixture in children. Can J Anesth 39(7): 661-664.
- Mehmood MT, Ahmed J, Haque SN (2009) caudal bupivacaine tramadol low dose combination for post operative analgesia in pediatric patients. Pak J Surg 25: 88-92.
- Laiq N, Khan MN, Tahmeedullah, Gandapur YK, Khan S (2009) Comparison of caudal bupivacaine and bupivacaine tramadol for postoperative analgesia in children undergoing hypospadias surgery. J Coll Physicians Surg Pak 19(11): 678-681.
- Demiraran Y, Kocaman B, Akman RY (2005) A comparison of the postoperative analgesic efficacy of single dose epidural tramadol versus morphine in children. Br J Anesth 95(4): 510-513.
- Prakash S, Tyagi R, Gogia AR, Singh R, Prakash S (2006) Efficacy of three doses of tramadol with bupivacaine for caudal analgesia in paediatric inguinal herniotomy. Br J Anesth 97(3): 385-388.
- Prosser DP, Davis A, Booker PD, Murray A (1997) Caudal tramadol for postoperative analgesia in pediatric hypospadias surgery. Br J Anesth 79(3): 293-296.
- Cook B, Doyle E (1996) The use of additives to local Anesthetic solutions for caudal epidural blockade. PaediatrAnesth 6(5): 353-359.
- Doctor TP, Dalwadi DB, Abraham L, Shah N, Chadha IA, et.al. (2013) Comparison of ropivacaine and bupivacaine with fentanyl for caudal epidural in pediatric surgery. Anesth Essays Res 7(2): 212-225.
- Kawaraguchi Y, Otomo T, Ota C, Uchida N, Taniguchi A, et.al. (2006) A prospective double blind randomized trial of caudal block using ropivacaine 0.2% with or without fentanyl 1 micro kg 1 in children. Br J Anesth 97(6): 858-861.
- Koinig H, Krenn CG, Glaser C, Marhofer P, Wildling E, et al. (1999) The dose response of caudal ropivacaine in children. Anesthesiology 90(5):1339-1344.
- Gaitini LA, Somri M, Vaida SJ, Yanovski B, Mogilner G, et al.(2000) Does the addition of fentanyl to bupivacaine in caudal epidural block have an effect on the plasma level of catecholamines in children. Anesth Analg 90(5): 1029-1033.
© 2018 Pavithra V. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






