- Submissions
Full Text
Developments in Anaesthetics & Pain Management
Addiction and Compliance
Keith A Raymond*
Emergency Medicine Physician, Austria
*Corresponding author: Keith A Raymond, Emergency Medicine Physician, Muckendorf, Austria, Europe
Submission: August 14, 2017;Published: November 02, 2017

ISSN 2640-9399 Volume1 Issue1
Introduction
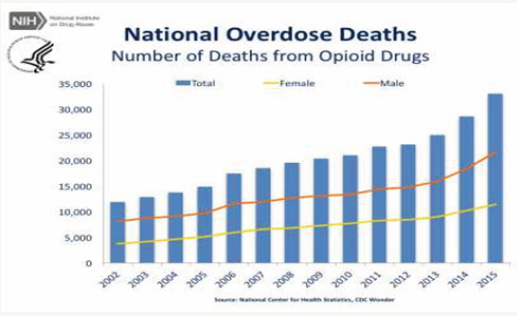
At the end of my clinical hours here in Europe, I met with some patients to discuss current events. They were completely unaware, and even surprised by, the opiate problem in the United States. It certainly is not a problem here in Austria, much less the rest of Europe. In Portugal, where illicit drugs were decriminalized in 2001, the drug overdose death rate was 3 per million in 2015. In the UK during the same year, it was 45 opiate related deaths per million [1]. For 2015, the NIH reported about 100 deaths per million in the US from opioid overdose. This is one overdose death per 5914 opiate prescriptions written in that year. The numbers in the US are worth reflection and appear suspect [2]. This suggests most of these deaths are due to diversion not prescription. To put these numbers in perspective, the number of people that died with Alzheimer’s disease in 2015 was 93,500 vs. opioid related deaths in the same year of 35,000 in the USA [3].
The UN World Drug Report of 2016 considered EU opiate consumption by country, using annual questionnaires. All countries showed decreases of use during the period from 1999 - 2014 except one, Italy. Heroin use in Italy doubled, from 0.4 percent of the population to 0.8 percent for ages 15 to 64. In 2015, 1.4 percent of male Italians, and 0.6 percent female Italians had injected drugs (refugees are included) (Figure 1).
Figure 1: In the US, the graph below demonstrates opioid overdose deaths.
Opiates and Compliance
This is not to recommend that opiates should be decriminalized in the US to reduce the overdose numbers. What it does suggest is that illegal opiate acquisition is much higher than prescription access due to diversion. Therefore, cracking down on physicians will only drive the opiate related deaths higher by un-supervised use, while increasing suffering of those with legitimate need. Recent literature is reflecting a physician backlash, while other doctors are shirking their responsibility to their patients by avoiding controlled substance prescriptions due to fear of investigation.
What is often not discussed is patient compliance, or the new terminology drug adherence, in this context. It has been the bane of physician existence since the time of Hippocrates. If the patient does not experience immediate and sustained benefit they may discontinue the prescribed care plan. Even if they do obtain benefit they may stop the medication preemptively, commonly seen with antibiotics, leading to incomplete infection elimination and drug resistant organism selection. To give you an idea how pervasive the issue is a study published in 2016 in MMWR indicated that 26% of Medicare Part D beneficiaries were non-adherent to their anti-hypertensive medication regimen. Money was not the issue, but the individual perception of absence of benefit certainly was [4]. Now, the availability of drug adherence studies with opiate prescriptions is lacking. Perhaps we can extrapolate from a study from 2014 that showed that consumption of opiate substitution treatment medicines along with other narcotic drugs were significantly more often reported for levomethadone (91.1%) and methadone (87.5%) than for buprenorphine (65.8%) (χ2 = 44.47, df = 2, p < 0.001) in Germany [5]. The assumption that compliance with opiate prescriptions is much higher than other medications may be patently false, although this is the common belief, at least in the USA. I suspect that opiate adherence is only slightly higher than other non-narcotic medications. In my experience, non-addicts will use opiates for pain only so long as the pain is intense. They may then choose over the counter remedies such as ibuprofen, naproxen, or aspirin if mild pain persists.
Opioid Supply and Demand
This is why many opioid prescriptions while filled; remain in storage in medicine cabinets once the acute phase of injury has been surmounted. Most non-addicts find the lack of mental clarity while on opiates or opioids interfere with daily life and function. Rather than faulting physicians for prescribing opioids, they should be faulted for prescribing suboptimal doses in excessive amounts. In the Emergency Department, the training to date has been to step up pain relief, simply stated, start low and go slow [6]. This idea has been extended to include prescribing practices. Even the CDC Opioid Prescribing Guideline of 2016 maintains this approach, ‘start with the lowest effective dose for chronic pain.’ What this means is incomplete pain relief for the majority of those with both acute and chronic pain, leading to additional dosing and potential addiction. This was recently reaffirmed by the FSMB Opioid Prescribing Guideline dated April 2017.
A superior pain management approach involves overwhelming the pain with opiates at high doses in the ED or clinic, then sending the patient home with up to three days of opiate medication, and a longer course of non-opiate analgesics. This leads to much lower total opiate dosing overall by not ramping up the dose to get them to relief. Further, the patient has complete pain control at the start and faster recovery. This is supported by pain research [7]. Once the pain cycle is broken, chance of reoccurrence is lower, and if it does occur it is of less intensity requiring minimal dosing to re-abolish. There is also a reduced risk of addiction using this approach.
Appropriate Pain and Pain Management
So why the schism between our understanding of pain and pain management? Perhaps we are stuck in old thinking patterns in this age of precision medicine. On the other hand, the correct use of opiates requires their use which is considered less than advisable in today’s anti-narcotic climate. So the recommendation is to seek less effective alternatives or presage inadequate opiate dosing schedules. Indeed, inadequate dosing is more likely the cause for addiction in this Opioid crisis. It also results in more cases of overdose due to the patients in pain taking matters into their own hands. Here is where compliance plays a roll. If the patient receives adequate analgesia they are more likely to follow the prescription. If they are given a short course, then switched to non-narcotic analgesia that meets their needs, compliance are assured. The alternative and current guidelines lead to excessive prescribing and inadequate pain relief.
I have met cancer and hospice patients that unreasonably fear addiction to opiates. These are folks that are the least likely to become addicts, yet have the greatest need. An attempt to instill this type of thinking into addictive personality types is ineffective. It is like showing bloody traffic accident films to kids ticketed for speeding; it increases rather than decreases risk and interest. Further research is needed to determine what the exact number of doses or a milligram of an opiate is needed to cause addiction. Then it would simply be a matter of limiting prescriptions below the addictive level. For example, the reason there are twenty cigarettes to a pack is that is the number needed to result in nicotine addiction. However, addiction itself is multi-factorial. There are some nonalcoholics that imbibe more alcohol than alcoholics. So knowing that addiction number for a specific opiate may be irrelevant.
If we can identify the addictive personality type in the ED via a questionnaire it also doesn’t mean we should deny them an opiate for pain relief. It means we need to revise our thinking about opiates and prescribe them based on science rather than on suspicions. We can treat pain, reduce the incidence of addiction, and maximize compliance if we continue to administer opiates wisely.
References
- Chris Ingraham (2015) The Independent, UK.
- 2015 207 million prescriptions were written for prescription opioid pain medications. (NIH statistics)
- Weuve J, Hebert LE, Scherr PA, Evans DA (2014) Deaths in the United States among persons with Alzheimer’s disease (2010–2050). Alzheimers Dement10(2): e40-e46.
- Ritchey M, Chang A, Powers C, Fleetwood L, Linda S, et al.(2016) Vital Signs: Disparities in Antihypertensive Medication Nonadherence Among Medicare Part D Beneficiaries-United States, 2014. Morb Mortal Wkly Rep 65(36): 967-976.
- Casati A, Piontek D, Pfeiffer-Gershel T (2014) Patterns of non-compliant buprenorphine, levomethadone, and methadone use among opioid dependent persons in treatment. Subst Abuse Treat Prev Policy 9: 19.
- Coluzzi F, Taylor R, Pergolizzi JV, Mattia C, Raffa RB (2016) Good clinical practice for opioids in pain management: the three Ts-titration(trial), tweaking(tailoring), transition(tapering). Rev Bras Anestesiol 66(3): 310-317.
- V Mehta, R M Langford (2006) Acute pain management for opioid dependent patients. Anaesthesia 61(3): 269-276.
© 2017 Keith A Raymond. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






