- Submissions

Full Text
Clinical Research in Animal Science
A Brief and Critical Review of Endemic Fluorosis in Domestic Animals of Scheduled Area of Rajasthan, India: Focus on Its Impact on Tribal Economy
Shanti Lal Choubisa*
Department of Advanced Science and Technology, National Institute of Medical Science and Research, NIMS University Rajasthan, Jaipur, Rajasthan 303121, India; Former Department of Zoology, Government Meera Girls College, Udaipur, Rajasthan 313001, India
*Corresponding author: Shanti Lal Choubisa, Department of Advanced Science and Technology, National Institute of Medical Science and Research, NIMS University Rajasthan, Jaipur, Rajasthan 303121, India; Former Department of Zoology, Government Meera Girls College, Udaipur, Rajasthan 313001, India
Submission: April 10, 2023;Published: May 22, 2023
ISSN: 2770-6729Volume 3 - Issue 1
Abstract
A special area has been created by the government of India by joining eight districts, namely, Banswara, Chittourgarh, Dungarpur, Pali, Pratapgarh, Rajasamand, Sirohi, and Udaipur out of 33 districts of the state of Rajasthan (India), which is called “scheduled area”. Along with the area being very backward and underdeveloped > 70% of the population of this area is tribals. These people are very poor and backward socio-economically and are financially dependent on agriculture and domestic animals including cattle (Bos taurus), water buffaloes (Bubalus bubalis), sheep (Ovis aries), and goats (Capra hircus). In this area, not only the tribals but also their animals are suffering from the dreaded fluorosis disease by drinking fluoride-rich water. In fact, in this tribal area, almost all drinking groundwater and some perennial fresh water sources are contaminated with fluoride (F) in the range of 1.0-21.6ppm and 0.1-3.05ppm, respectively, which is higher than the recommended standard limits, 1.0 or 1.5ppm, in the country. Many industrial processes are also going on in this tribal area which are emitting F into the environment. Chronic F exposure through these sources numbers of domestic animals are suffering with mild to severe F poisoning. However, dental fluorosis is more prevalent and rampant in this area. At 1.5-4.4ppm of F in drinking groundwater, 28.3-70.2% and 25.7-64.1% animals of different species (mainly bovines and flocks) are found to be afflicted with dental and skeletal fluorosis, respectively. Lameness and ankylosis bone deformities are the worst conditions of chronic F intoxication in these animals. >82% bovine calves are also suffering with fluorosis in this area. However, bovine animals are relatively severely afflicted with chronic F poisoning compared to flock animals. In the present communication, various sources of F exposure, different forms of fluorosis, diverse determinants, susceptibility of F toxicity, bio-indicators and biomarkers of chronic F poisoning, impact of endemic fluorosis on tribal economy, and the prevention and control of fluorosis have been considered and briefly and critically reviewed. Along with this, the shortcomings of the research have also been highlighted. The findings of this review may contribute to the formulation and implementation of health plan for mitigation and control of fluorosis in domestic animals of scheduled area of Rajasthan (India).
Keywords:Bio-indicators; Biomarkers; Dental fluorosis; Fluoride; Food-born fluorosis; Groundwater, Hydrofluorosis; Industrial fluorosis; Scheduled area; Skeletal fluorosis; Tribals; Rajasthan; India
Introduction
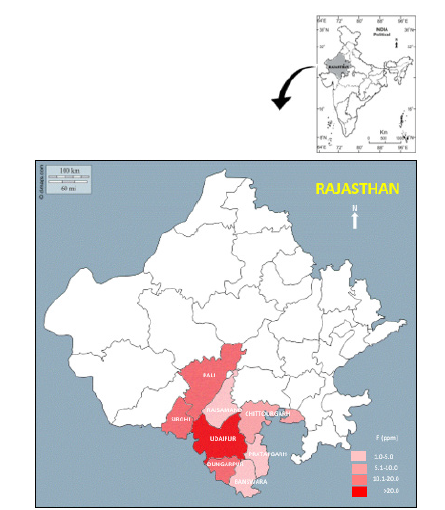
Rajasthan is the largest state in India in which eight districts out of 33 districts, namely Banswara, Chittorgarh, Dungarpur, Pali, Pratapgarh, Rajsamand, Sirohi, and Udaipur have been carved out by the government of India as a special region called “Scheduled Area” (Figure 1). Along with this area being very backward and underdeveloped, >70% of the population in this area is tribals. Apart from traditional agriculture, these people also depend on cattle (Bos taurus), water buffalo (Bubalus bubalis), sheep (Ovis aries) and goats (Capra hircus) animals for regular income of the household. As per the recent Livestock Census 2019, the total livestock population in the country is 535.78 million. Out of this, the population of cow, buffalo, sheep, and goats is 35.95%, 20.45%, 13.87%, and 27.80%, respectively. In the state of Rajasthan, the total population of livestock is 56.8 million. Of which, 13.9 million are cattle, 13.7 million buffaloes, 7.9 million sheep and 20.84 million goats. Generally, the tribal people of this area use these animals for agriculture, milk production, and meat business.
Figure 1:Map showing scheduled area of Rajasthan (as per notification of Government of India, 2018).

80 decades ago, in the scheduled area of Rajasthan, tribal people used to feed water to their domesticated animals including cattle (Bos taurus), water buffaloes (Bubalus bubalis), sheep (Ovis aries), and goats (Capra hircus) from nearby fresh water sources, open-wells, ponds, rivers, etc. But since thousands of hand-pumps and bore-wells have become available in the area, the tribals have started watering their livestock from these sources. In fact, “Dracunculus Eradication Programme” has been the reason behind the high number of these drinking water sources in the scheduled area of Rajasthan [1]. Because the drcunculiasis disease caused by infection of human nematode, dracunculus worm (Dracunculus medinensis), was endemic especially in this area, hand-pumps and bore-wells were dug at various places to break the life cycle of this worm [2-4]. But at that time responsible people did not know that there was F chemical in the groundwater of these drinking water sources.
In rural India, the groundwater of 23, out of 37 states and union territories is found to be contaminated with fluoride (F) with varying amount [5]. In Rajasthan and its scheduled area drinking groundwater is also highly contaminated with F (Figure 2); [1,6- 10]. It is well known that drinking water containing F above the threshold level 1.0 or 1.5ppm [11-13] for prolonged period causes dreaded fluorosis (hydrofluorosis) disease not only in humans [11,14] but also in various species of wild [15-17] and domestic animals [18-28]. Chronic F exposure through industrial fluoride pollution is also causes fluorosis in man and animals [29-35]. In the scheduled area of Rajasthan, chronic F poisoning in the form of hydrofluorosis at different F levels in drinking groundwater has been extensively studied in tribal people [36-46] and their domesticated animals, bovines and flocks [47-57]. In the present communication, various sources of F exposure, different forms of fluorosis, various determinants, relative susceptibility of F toxicity, bio-indicators and biomarkers of chronic F poisoning, impact of endemic fluorosis on tribal economy, and preventive measures and control of fluorosis have been considered and briefly and critically reviewed. Along with this, the shortcomings of the research have also been highlighted. The findings of this review may contribute to the formulation and implementation of health plan for mitigation and control of fluorosis in domestic animals of scheduled area of Rajasthan (India).
Figure 2:Map showing F distribution in eight districts of scheduled area of Rajasthan (India).
Fluoride Sources of Risk in the Scheduled Area
Overall, three major sources of F exposure or risk are prevalent
in the scheduled area of Rajasthan, with potential and active roots
for chronic F intoxication in domesticated animals of tribals. These
are:
i. F-contaminated drinking water,
ii. industrial fluoride emissions, and
iii. fluoridated foods.
However, the first source of F exposure is the primary source that is most common and widely prevalent in this tribal area, while the others are secondary and tertiary sources of F toxicity, respectively, and are confined to the particular location or region.
F-contaminated drinking water
In the villages of scheduled area, among different drinking water sources, deep bore-wells and hand-pumps are the most common drinking water sources for both tribal people and their domesticated bovine and flock animals. Though, for drinking water, some seasonal and perennial water sources (ponds and reservoirs) are also available for these animals. In the scheduled area, water of hand-pumps and deep bore-wells are, generally, contaminated with F in the range of 1.0-21.6ppm [1,6-10] which is higher than the recommended standard or threshold value 1.0 or 1.5ppm in the country [11-13]. In this area, water of some seasonal ponds and perennial reservoirs is also found to be contaminated with F in the range of 0.1-3.05ppm [9]. The distribution of F in drinking groundwater of eight districts of scheduled area has been shown in Figure 2. This has been unanimously accepted that drinking of such F-rich water for a long time becomes toxic and is injurious to animal health. In the scheduled area, not only domesticated animals but also tribal people are also afflicted with chronic F poisoning in form of hydrofluorosis due to consumption of fluoridated groundwater for drinking and cooking purposes [36-46].
Industrial F emission
In recent years, in the scheduled area of Rajasthan, another possible source of F exposure is an industrial F emission. In this region, number of industrial activities such as Hindustan Zinc Smelter, phosphate and chemical fertilizer factories and manufacturing or production of bricks, glass, plastic, cement and hydrofluoric acid are considerably discharging F in both gaseous and particulate /dust forms into their surrounding environments which create an industrial F pollution. Fluoride emitted by the industry not only contaminates the surrounding soil, air, and drinking water reservoirs but also contaminates vegetation, agricultural crops, diverse food-chains and ecological webs, and many other biological communities on which tribal people and domestic animals are generally dependent on them for food. The long-term inhalation and/or ingestion of industrial F also causes diverse mild to severe toxic effects in the form of industrial and neighborhood fluorosis in domestic animals and tribal people, respectively [29-35].
Fluoridated foods
Besides the fluoridated drinking water and industrial F emission, other anthropogenic sources of F exposure are feed supplements such as mineral and phosphate supplements or commercial phosphorous lick to domesticated animals. But these sources are uncommon and restricted to those tribal people who can afford to purchase these feed supplements for their domesticated animals. In fact, these feed supplements contain high amounts of F therefore, these are also potential sources for the development of food-born fluorosis in domesticated animals [18]. However, this food-borne fluorosis in domesticated animals is yet to be reported in the Scheduled Area of Rajasthan. However, few reports are available on this entity in other parts of the country [58,59]. Green grasses and crop feeds (fodder) irrigated with F- rich water are also contain F in varying amount and are also sources of chronic F exposure for domestic animals. In fact, these are contributing sources and cumulative to the principle F exposure or fluoridated drinking water and having significant role in increasing of severity F toxicity in animals. The milk of fluoridated animals also contains high amounts of F which is also a potential source for the development of fluorosis in calves, lambs, and children [60- 64]. But data on food-born fluorosis are not enough in the country. Therefore, more research studies on food- born fluorosis in domesticated animals are highly suggestive. Data from such studies are useful in health risk assessment in domestic animals as they are economically very important for tribal people.
Fluorosis in Domestic Animals in Scheduled Area
Whatever may be the sources of F exposure to domestic animals, once F enters the body, it is absorbed by the digestive and/or respiratory tract. From these F reaches different organs or tissues or every part of the body through the blood circulation system. More than 50% of F is absorbed from the digestive and respiratory tract, leaving the body through excretory products (faeces and urine) and sweat, while the rest remains in the body where it accumulates slowly in various biological or organ systems. However, due to its high affinity with calcium, its maximum amount is deposited in calcified skeletal and dental tissues and minimum in non-calcified tissues or soft organs. The accumulation of F in various organs affects their physiology and architecture and ultimately triggers the generation of various adverse reversible and non-reversible toxic health effects in the body. These toxic changes are collectively known as fluorosis [11]. If fluorosis is the result of drinking F-enriched water, the term is usually referred to as “hydrofluorosis”. Similarly, fluorosis resulting from exposure to F through industrial F pollution and fluoridated foods is also known as “industrial fluorosis” and “food-borne fluorosis”, respectively. Whatever F- induced toxic damage or malformations appear in the teeth (dental fluorosis) and bones (skeletal fluorosis), they are generally permanent and non-reversible. These deformities are lifelong or permanent and most of them are visible from the eyes. However, F- induced changes in various soft tissues or organs (nonskeletal fluorosis) are reversible and disappear after the source of F exposure is removed.
Dental fluorosis
The earliest visible pathognomonic or clinical symptom of chronic F intoxication (fluorosis) in humans and animals is discoloration of the teeth or dental molting, commonly referred to as dental fluorosis [11]. This is the most sensitive, irreversible, easily recognizable, and indexive sign of chronic F poisoning. In the scheduled area, dental fluorosis is the most common and rampant in tribals as well as in their domesticated animals. This entity can be easily identified by the presence of bilateral striated, condensed or diffused and varying degree of horizontal light to deep brownish staining strips on the surface of anterior teeth (Figures 3 & 4) of flourosed animals [23,55,56]. These well stained strips are visualized more sharply and contrast in calves or immature animals (Figure 3A-3C). In some cases, dental fluorosis also appears as brown spots, patches, and fine dots on the enamel of teeth. In its advanced stage, gingivitis and excessive tooth wear with obvious loss of teeth supporting the alveolar bone are also caused by chronic F intoxication which is more prevalent in older animals (Figure 4A-4D). In scheduled area, well layered light to deep black tooth staining was also found in some buffalo calves instead of brownish yellow [48]. Recently, such finding has also been reported in cattle calves of Thar Desert of Rajasthan [22]. The reason behind this difference in staining is still not understood.
Figure 3:Moderate to severe dental fluorosis in bovine calves (A-C) and juvenile (D) and sheep (E) and goat (F) characterised with stiatification with deep brownish staining which is clearer in cattle (A and B) and buffalo calves (C).

Figure 4:An advance stage of dental fluorosis in bovines of higher age group showing irregular striatification with deep brownish staining, pronounced loss of teeth supporting alveolar bone with recession and swelling of gingival, and excessive wearing of teeth giving a wavy appearance.
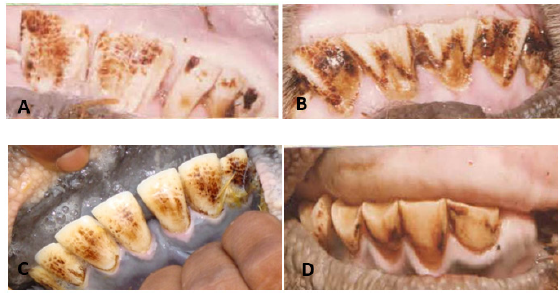
In the tribal villages of scheduled area where F concentration is 1.5-4.4ppm in drinking water, the highest prevalence of dental fluorosis in cattle, buffaloes, sheep, and goats was found to be 50.6%, 70.2%, 28.3%, and 32.9%, respectively [53]. In these villages, >82% bovine calves have also been found to be afflicted with dental fluorosis (Figure 4A-4C) [23]. Whatsoever, F- induced disfigure of teeth reduces the lifespan of these animals. When these dental lesions become severe enough to cause difficulty in grazing and mastication, the animals die at a young age from hunger and cachexia [11,65].
Skeletal fluorosis
Figure 5:Severe skeletal fluorosis in domesticated bovines showing lameness, enlarged joints, debility, invalidism, hoof deformities, wasting of body muscles and bony lesions in the mandibles, ribs, metacarpus and metatarsus regions. Ankylosis deformity is also found in cattle (C and D).
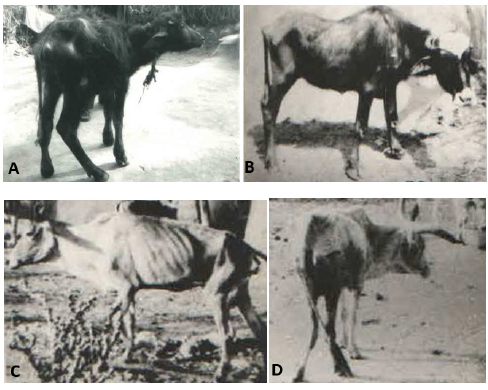
Figure 6:Moderate and severe skeletal fluorosis in domesticated bovines (A and B) and flocks (C and D) characterised with lameness, enlarged joints, debility, invalidism, wasting of body muscles and bony lesions in the mandibles, ribs, metacarpus, and metatarsus regions.
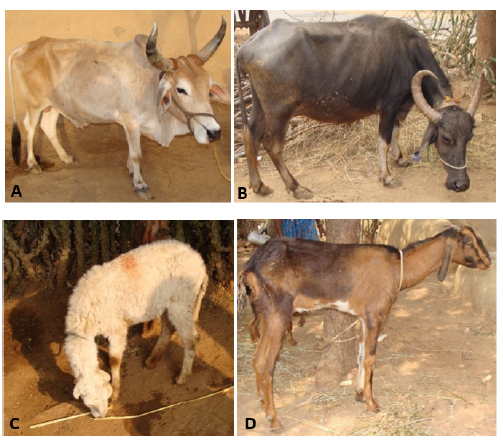
Excess accumulation of F in various skeletal bones and their associated muscles and ligaments causes mild to severe deformities and are more dangerous and highly painful. In fact, these deformities are highly significant because they reduce or limit mobility in humans and animals at a very young age due to different architectural changes in the bones, such as periosteal exostosis, osteosclerosis, osteoporosis, and osteophytosis [66-70]. These changes manifest clinically as vague aches and pains in the body and joints that are associated with stiffness or rigidity and lameness, stunted growth, obvious bone lesions, and a cracking or snapping sound in the legs when walking in animals [48]. In addition, these progressive and irreversible bony changes become more severe as the animal progresses in age or in animals of higher age. Excess accumulation of F in muscle also reduces or restricts normal bone movement, causing lameness in animals. Although intermittent lameness, enlarged joints, debility, invalidism, hoof deformities, wasting of body muscles, and bony exostosis or lesions in the mandibles, ribs, metacarpus, and metatarsus regions are well recognized in the fluorosed animals (Figures 5 & 6) [48,55]. Cases of ankylosis have also been observed in animals due to drinking fluoridated water in scheduled areas, in very advanced stages of skeletal fluorosis (Figure 5). Such findings have been reported previously [71]. But such cases of severe form of skeletal fluorosis are very rare in the country.
In many tribal villages of scheduled area where F concentration is between 1.5-4.4ppm in diverse drinking water sources, the highest prevalence of skeletal fluorosis in cattle, buffaloes, sheep, and goats was found to be 42.7%, 64.1%, 25.7%, and 29.1%, respectively [51]. In these villages, >10% bovine calves are also found to be afflicted with mild to severe skeletal fluorosis (Figure 5A, 5B) [9].
Non-skeletal fluorosis
Whatever F induced manifestations in various organs are referred to as non-skeletal fluorosis. In fluoride and fluorosis endemic tribal villages of scheduled area, the most common F induced health complaints in domesticated animals have been reported as muscles/body weakness, frequently intake of water (polydipsia), frequent tendency to urinate (polyuria), gastrointestinal discomforts (loss of appetite, bloating, colic pain, constipation, intermittent diarrhea, etc.), allergic reactions, irregular reproductive cycles, abortion, still birth, etc. [19,21,55]. Interestingly, these health consequences are temporary and are mostly reversible after withdrawal of F exposure or removing the animals from F endemic area to non-fluoride endemic area. However, these health complaints in animals are only observational and not conclusive from experimental studies. Research work on fluorotoxicosis in excretory and male and female reproductive systems in different species of domestic animals is not scientifically fully justified and yet sufficient. F-induced effects on reproductive organs, endocrines glands, gametogenesis, embryogenesis, and brain are also not well studied and not at level of satisfactory in these domestic animals. Hypothyroidism in domestic animals has not yet been reported. Therefore, well-designed scientific experimental studies are highly needed to unravel the exact mechanisms involved at the molecular level for chronic F intoxication in different organs as well as endocrine glands in different species of domestic animals living in different ecosystems, arid and humid.
Determinants and Susceptibility of F Toxicosis
The prevalence and severity of fluorosis varies greatly among animals of the same or different species living either in the same or different geographic provinces, with drinking water having approximately the same F concentrations. This may be possible and indicates that some factor or determinant is involved in controlling or inducing F toxicity. In addition to the frequency of the main determinant F concentration and its duration and risk factors, other are chemical components in drinking water, age, sex, habits, food components, environmental factors, individual sensitivity and biological response or tolerance, and genetics can also significantly accelerate F toxicosis in both animals and humans [72-78]. These findings on determinants are more useful in the implementation or commencement of fluorosis control campaign. However, more studies are still needed for the understanding of correlation of these determinants with severity of chronic F intoxication in different species of animals rearing in the different geographical provinces having almost identical F concentration in drinking water or source of F exposure.
Indeed, major manifestations of chronic F intoxication have emerged as a global animal health problem. Unfortunately, besides considerable outstanding developments in veterinary sciences, a complete cure or reversal of osteo-dental fluorosis is still not known. However, in an experimental condition some of chemical substances like molybdenum (Mo), phosphate (P), sulphate (SO42-), etc. have been reported to induce chemicals intestinal absorption of F while other chemical like calcium (Ca), vitamin A, C and D reduce its absorption [11]. Experimentally, it has been well studied that Ca, ascorbic acid (vitamin C) and vitamin-D3 chemical factors have potential to reduce the F toxicity [76].
A large observational survey study conducted in bovines and flocks living in tribal villages in the scheduled area with low F content (1.5-1.7ppm) in drinking water showed that grass eaters bovines had the highest prevalence and severity of osteo-dental fluorosis as compared to the plant eaters flocks [77,79]. This indicates that bovines are relatively more susceptible to F poisoning than flock animals. Natural alleviation of F toxicity in plant eater animals living in high F endemic areas has also been reported [55,56,75]. In fact, flock animals typically eat small, delicate fresh leaves, legumes, and small fruits of trees and shrubs that contain substantial amounts of calcium (Ca) and ascorbic acid (vitamin C) nutrients. Both nutrients interfere with F metabolism and ultimately reduce the F toxicity. Similarly, in dromedary camels, F toxicity is also found less due to high content these nutrients in their natural foods [80]. Although the reversibility of dental fluorosis by supplementation of these nutrients in humans is still controversial, its further advancement can be checked by supplementation of Ca and vitamin C nutrients [76]. This indicates that both these nutrients can alleviate the F effects but cannot reverse dental and skeletal deformities.
Furthermore, in survey studies [9], it has been observed that bovine calves have higher susceptibility and sensitivity and lower tolerance to F compared to lambs and kids of flocks. Therefore, bovine calves are found to be suffering from severe fluorosis. Interestingly, in the study, none of lambs and kids were found to be afflicted with either dental or skeletal fluorosis. From this, it can be concluded that flock animals are naturally protected from chronic F poisoning due to the presence of rich amounts of Ca and vitamin C nutrients in their feed [79,80]. However, differences in the prevalence of fluorosis between goats and sheep are due to differences in sensitivity to F and the amount, duration, and frequency of F ingestion. Sheep animals are generally well adapted to arid environments and require relatively less amount of water for their survival. Hence, they have less and irregular F exposure resultant to lower F toxicity as in the case of dromedary camels [20,80].
Bio-Indicators and Biomarkers for Fluorosis
Any bio-indicator should have low resistance or tolerance to fluorosis, but high sensitivity or susceptibility to F exposure and give early signs of F intoxication. Recently, a large study was performed in mature and immature animals belonging to different species of animals residing in the scheduled area of Rajasthan where drinking water sources are naturally contaminated with F [81]. Interesting that among these animals, immature ones were found to be more susceptible to chronic F toxicosis and revealed its early clinical sign in the form of dental fluorosis. However, bovine calves are relatively more ideal bio-indicators for chronic F intoxication as these showed an early clinical sign of dental fluorosis [81].
Biomarker or biological marker generally refers to a measured characteristic that can be used as an indicator of some biological state. The term also sometimes refers to a substance whose presence indicates the existence of living organisms. These biomarkers are often measured and assessed to investigate normal biological processes or pharmacological responses to therapeutic intervention. F content in environmental samples such as feed and fodder indicate persistence of F contamination in the environment [82,83]. However, F contents in biological samples (milk, urine, blood serum, nails, teeth, bones, etc.) are also better biomarkers for chronic F intoxication in man and animals in contrast to morbidity and mortality [84-89]. Nevertheless, the presence of F in blood serum and urine is the most ideal method for the indication of current status of chronic F poisoning [14,90].
Impact of F and Endemic Fluorosis on Tribal Economy
The economic condition of the tribal people of scheduled area of Rajasthan is very poor. Economically, they are mainly dependent on traditional agriculture and animal husbandry. Despite the availability of sufficient essential resources and advanced equipment for modern farming, most of the tribal people are unable to use and purchase them for their farming due to poor economic conditions. Therefore, these people are heavily dependent on domesticated oxen for their traditional agriculture. But most of these bulls suffer from a severe form of incurable skeletal fluorosis disease. In general, these flourosed animals are physically weak and unable to walk properly due to having of F- induced lameness. As these animals are not useful for farming purposes, the tribal people have no option except to buy new bulls and cause them unintended economic loss. On the other hand, people like to buy lame animals in the market less. Due to this reason, tribal people are forced to sell them at low prices. Due to not getting proper price for these animals in the market, the economic condition of these people becomes weaker. On the other hand, irrigation with fluoridated water also reduces agricultural crop production [91] which also causes significant economic losses to tribal farmers. The tribal people of this area also do milk business for daily or household income. That’s why these people breed and raise cow-buffalo for milk production. Due to chronic F toxicosis, the production of milk in these animals is reduced, due to which these people have to suffer economic loss due to less income. Due to poor quality of meat of fluorosed buffalo, sheep, and goats, the tribal people do not get good prices in the market. This is also a cause of huge loss to tribal subjects.
Interestingly, neither tribal people nor veterinarians in scheduled areas know the negative aspect of dental fluorosis in animals. In fact, dental fluorosis mitigates the lifespan of animals. When dental fluorosis is more severe than due to difficulty in grazing and mastication, the animals die at a young age from starving and emaciation [11,65]. Yet, the death of animals at a young age has greater economic consequences for tribal people of scheduled area of Rajasthan [56,75].
In fact, both F and fluorosis weaken the economic condition of the tribal people. But neither the tribals nor the concerned government departments are aware of the type of economic loss. Therefore, it is absolutely necessary to take all possible measures so that the tribal individuals of this area do not suffer financial loss due to causative factors, endemic fluoride and fluorosis. It is difficult to state that due to fluoride and fluorosis how much economic loss is caused to the tribal individuals of this scheduled area. But it can be evaluated after doing scientific research on this aspect. This type of assessment is more important and necessary in making health and economic policy in underdeveloped and backward scheduled area of Rajasthan.
Prevention and Control of Fluorosis in Scheduled Area
Most of the tribals do not know that there is no cure for fluorosis disease yet. Due to superstition, these people treat animals suffering from fluorosis in their traditional way which is very cruel. In this, the neck, shoulder, back and neck of the animal suffering from fluorosis are burnt or stained with a hot iron rod. But these animals die quickly due to secondary infection in deep wounds on the body. But with a little effort this disease can be checked easily. For this, first it is necessary to prevent F from entering the animal’s body. Therefore, F- free healthy foods and drinking water should be provided to animals. It is also important, generating general awareness in the tribals and veterinarians regarding the preventive measures of chronic F poisoning in animals. Defluoridation of fluoridated water can be done by adopting appropriate defluoridation techniques. Although several defluoridation techniques are available. However, one of them, Nalgonda defluoridation technique is most appropriate, suitable, and effective and also less costly [92]. In the scheduled area this technique has been adopted but its success rate is still very poor and at many places it is a total failure due to lack of proper monitoring, maintenance, responsibility, and handling. However, harvesting and conservation of rainwater are the most ideal methods to get regular F- free drinking water for domesticated animals. Another effective option is to provide treated fresh or surface water for ponds, reservoirs, dams, rivers, etc. instead of groundwater to domesticated animals which contain F in the range of 0.01-0.3ppm [11,93]. Shifting of animals from F endemic or industrial F pollution area to non-F endemic or non-industrial F pollution area is also one of the ways for prevention and control of F intoxication in domestic animals.
Conclusion
More than 70% of the tribal people living in the scheduled area of Rajasthan are economically poor and economically dependent on agriculture and animal husbandry. In general, tribal people rear bovine and flock animals for their agriculture and household income. But due to chronic F exposure through F-contaminated drinking water and industrial F pollution, most of these animals are suffering from dangerous fluorosis disease. Lameness and ankylosis deformities in these animals are the worst condition of this disease. F and endemic fluorosis are not only affecting the health of the tribal people and their domesticated animals but also affecting the economy of the tribal people. But this disease could be checked by providing F- free healthy foods and drinking water. General awareness about this disease in tribal people is also important for its prevention and control in tribals and their reared animals. In the scheduled area, an epidemiological survey studies on chronic F intoxication in diverse species of domestic animals is highly suggestive to know the current status of various fluoroses. During the survey studies, biological (urine, blood serum, milk, hair, teeth, bones, etc.) and environmental (soils, grass, water, cereals, vegetables, etc.) samples should also be collected and analyzed for evidence of F content which indicates the current status of fluorosis. Findings of these studies are useful in making health policy to control fluorosis in this backward and underdeveloped tribal area. The significance of the present review is to provide scientific information about the F and its toxicosis in diverse species of domestic animals which is useful in framing of future health plan for the mitigation of chronic F poisoning in this tribal area.
Acknowledgement
The author is thankful to Dr. Darshana Choubisa, Associate Professor, Department Prosthodontics and Crown & Bridge, Geetanjali Dental and Research Institute, Udaipur, Rajasthan 313002, India for cooperation.
References
- Choubisa SL (2018) Fluoride distribution in drinking groundwater in Rajasthan, India. Current Science 114(9): 1851-1857.
- Choubisa SL (2002) Guinea worm (Dracunculus medinensis) in Rajasthan, India: A case report. Journal of Parasitic Diseases 26(2): 105-106.
- Choubisa SL, Verma R, Choubisa L (2010) Dracunculiasis in tribal region of Rajasthan (India): A case report. Journal of Parasitic Diseases 34(2): 94-96.
- Choubisa SL (2022) A historical dreaded human nematode parasite, Dracunculus worm (Dracunculus medinensis) whose awe is still alive in elderly of India! Can't it reappear in India (editorial)? Austin Public Health 6(1): 1019.
- Choubisa SL (2018) A brief and critical review on hydrofluorosis in diverse species of domestic animals in India. Environmental Geochemistry and Health 40(1): 99-114.
- Choubisa SL, Sompura K, Choubisa DK, Pandya H, Bhatt SK, et al. (1995) Fluoride content in domestic water sources of Dungarpur district of Rajasthan. Indian Journal of Environmental Health 37(3): 154-160.
- Choubisa SL, Sompura K, Choubisa DK, Sharma OP (1996) Fluoride in drinking water sources of Udaipur district of Rajasthan. Indian Journal of Environmental Health 38(4): 286-291.
- Choubisa SL (1997) Fluoride distribution and fluorosis in some villages of Banswara district of Rajasthan. Indian Journal of Environmental Health 39(4): 281-288.
- Choubisa SL (1996) An epidemiological study on endemic fluorosis in tribal areas of southern Rajasthan. A technical report. The ministry of Environment and Forests, Government of India, New Delhi, India, pp. 1-84.
- Choubisa SL (2022) Status of chronic fluoride exposure and its adverse health consequences in the tribal people of the scheduled area of Rajasthan, India. Fluoride 55(1): 8-30.
- Adler P, Armstrong WD, Bell ME, Bhussry BR, Büttner W, et al. (1970) Fluorides and human health. World Health Organization Monograph Series No. 59. World Health Organization, Geneva, Switzerland.
- ICMR (Indian Council of Medical Research) (1974) Manual of standards of quality for drinking water supplies. Special report series No. 44, Indian Council of Medical Research, New Delhi, India.
- BIS (Bureau of Indian Standards) (2012) Indian standard drinking water-specification. 2nd revision. New Delhi: Bureau of Indian Standards, New Delhi, India.
- Choubisa SL (2018) A brief and critical review of hydrofluorosis in Rajasthan, India. Fluoride 51(1): 13-33.
- Shupe JL, Olson AE, Peterson HB, Low JB (1984) Fluoride toxicosis in wild ungulates. Journal of the American Veterinary Medical Association 185(11):1295-1300.
- Shupe JL, Olson AE, Sharma RP (1972) Fluoride toxicity in domestic and wild animals. Clinical Toxicology 5(2): 195-213.
- James RN, Ming-ho Y (1976) Fluorosis in black-tailed deer. Journal of Wildlife Diseases 12(1): 39-41.
- Swarup D, Dwivedi SK (2002) Environmental pollution and effect of lead and fluoride on animal health. Indian Council of Agricultural Research, New Delhi, India, pp. 68-106.
- Choubisa SL (2010) Osteo-dental fluorosis in horses and donkeys of Rajasthan, India. Fluoride 43(1): 5-10.
- Choubisa SL (2010) Fluorosis in dromedary camels of Rajasthan, India. Fluoride 43(3): 194-199.
- Choubisa SL (2012) Status of fluorosis in animals. Proceedings of National Academy of Sciences, India Section B: Biological Sciences 82(3): 331-339.
- Choubisa SL, Modasiya V, Bahura CK, Sheikh Z (2012) Toxicity of fluoride in cattle of the Indian Thar Desert, Rajasthan, India. Fluoride 45 (4): 371-376.
- Choubisa SL (2021) Chronic fluoride exposure and its diverse adverse health effects in bovine calves in India: an epitomised review. Global Journal of Biology, Agriculture and Health Sciences 10(3): 1-6.
- Choubisa SL (2022) A brief and critical review of chronic fluoride poisoning (fluorosis) in domesticated water buffaloes (Bubalus bubalis) in India: focus on its impact on rural economy. Journal of Biomedical Research and Environmental Sciences 3(1): 96-104.
- Choubisa SL (2022) A brief review of chronic fluoride toxicosis in the small ruminants, sheep and goats in India: focus on its adverse economic consequences. Fluoride 55(4): 296-310.
- Choubisa SL (2023) Endemic hydrofluorosis in cattle (Bos taurus) in India: an epitomised review. International Journal of Veterinary Science and Technology 8(1): 001-007.
- Choubisa SL (2023) A brief review of fluorosis in dromedary camels (Camelus dromedarius) and focus on their fluoride susceptibility. Austin Journal of Veterinary Science and Animal Husbandry 10(1): 1-6.
- Choubisa SL, Choubisa D, Choubisa A (2023) Fluoride contamination of groundwater and its threat to health of villagers and their domestic animals and agriculture crops in rural Rajasthan, India. Environmental Geochemistry and Health 45(3): 607-628.
- Choubisa SL (2015) Industrial fluorosis in domestic goats (Capra hircus), Rajasthan, India. Fluoride 48(2): 105-115.
- Choubisa SL, Choubisa D (2015) Neighbourhood fluorosis in people residing in the vicinity of superphosphate fertilizer plants near Udaipur city of Rajasthan (India). Environmental Monitoring and Assessment 187(8): 497.
- Choubisa SL, Choubisa D (2016) Status of industrial fluoride pollution and its diverse adverse health effects in man and domestic animals in India. Environmental Science and Pollution Research 23(8): 7244-7254.
- Panchal L, Sheikh Z (2017) Dental fluorosis in domesticated animals in and around Umarda village of Udaipur, Rajasthan, India. Haya: The Saudi Journal of Life Sciences 2 (7): 248-254.
- Sheikh Z, Panchal L (2018) Anthropogenic fluoride contamination and osteo-fluorosis in bovines inhabiting Umarda, Jhamarkotra and Lakkadwas villages of Udaipur, Rajasthan, India. International Journal of Innovative Research and Reviews 6 (1): 12-20.
- Choubisa SL (2023) Industrial fluoride emissions are dangerous to animal health, but most ranchers are unaware of it (editorial). Austin Environmental Sciences 8(1): 1089.
- Choubisa SL (2023) A brief review of industrial fluorosis in domesticated bovines in India: focus on its socio-economic impacts on livestock farmers. Journal of Biomed Research 4(1): 8-15.
- Choubisa SL, Sompura K, Bhatt SK, Choubisa DK, Pandya H, et al. (1996) Prevalence of fluorosis in some villages of Dungarpur district of Rajasthan. Indian Journal of Environmental Health 38(2): 119-126.
- Choubisa SL, Verma R (1996) Skeletal fluorosis in bone injury case. Journal of Environmental Biology 17(1): 17-20.
- Choubisa SL, Sompura K (1996) Dental fluorosis in tribal villages of Dungarpur district (Rajasthan). Pollution Research 15(1): 45-47.
- Choubisa SL, Choubisa DK, Joshi SC, Choubisa L (1997) Fluorosis in some tribal villages of Dungarpur district of Rajasthan, India. Fluoride 30(4): 223-228.
- Choubisa SL (1998) Fluorosis in some tribal villages of Udaipur district (Rajasthan). Journal of Environmental Biology 19(4): 341-352.
- Sompura K, Choubisa SL (1999) Some observations on endemic fluorosis in the villages of Sagawara Panchayat Samiti of Dungarpur district, Rajasthan. In: Proceedings of National Seminar on Fluoride, Fluorosis and Defluoridation Techniques, M.L.S. University, Udaipur, India, pp. 66-69.
- Choubisa SL (1999) Chronic fluoride intoxication (fluorosis) in tribes and their domestic animals. International Journal of Environmental Studies 56(5): 703-716.
- Choubisa SL (2001) Endemic fluorosis in southern Rajasthan (India). Fluoride 34(1): 61-70.
- Choubisa SL, Choubisa L, Choubisa DK (2001) Endemic fluorosis in Rajasthan. Indian Journal of Environmental Health 43(4): 177-189.
- Choubisa SL (2012) Fluoride in drinking water and its toxcosis in tribals, Rajasthan, India. Proceedings of National Academy of Sciences, India Section B: Biological Sciences 82(2): 325-330.
- Choubisa SL, Choubisa D (2019) Genu-valgum (knock-knee) syndrome in fluorosis- endemic Rajasthan and its current status in India. Fluoride 52(2): 161-168.
- Choubisa SL, Pandya H, Choubisa DK, Sharma OP, Bhatt SK, Khan IA (1996) Osteo-dental fluorosis in bovines of tribal region in Dungarpur (Rajasthan). Journal of Environmental Biology 17(2): 85-92.
- Choubisa SL (1999) Some observations on endemic fluorosis in domestic animals of southern Rajasthan (India). Veterinary Research Communications 23(7): 457-465.
- Choubisa SL (2000) Fluoride toxicity in domestic animals in Southern Rajasthan. Pashudhan 15(4): 5.
- Choubisa SL (2007) Fluoridated ground water and its toxic effects on domesticated animals residing in rural tribal areas of Rajasthan (India). International Journal of Environmental Studies 64(2): 151-159.
- Choubisa SL (2008) Dental fluorosis in domestic animals. Current Science 95(12): 1674-1675.
- Choubisa SL, Mali P (2009) Fluoride toxicity in domestic animals. In: Dadhich L, Sultana F (Eds.), Proceedings of the National Conference on Environmental Health Hazards; Kota, Rajasthan, India, p. 103.
- Choubisa SL, Mishra GV, Sheikh Z, Bhardwaj B, Mali P, et al. (2011) Toxic effects of fluoride in domestic animals. Advances in Pharmacology and Toxicology 12(2): 29-37.
- Choubisa SL (2012) Study of natural fluoride toxicity in domestic animals inhabiting arid and sub-humid ecosystems of Rajasthan. A technical report. University Grants Commission, New Delhi, India.
- Choubisa SL (2013) Fluorotoxicosis in diverse species of domestic animals inhabiting areas with high fluoride in drinking waters of Rajasthan, India. Proceedings of National Academy of Sciences, India Section B: Biological Sciences 83(3): 317-321.
- Choubisa SL (2013) Fluoride toxicosis in immature herbivorous domestic animals living in low fluoride water endemic areas of Rajasthan, India: an observational survey. Fluoride 46(1): 19-24.
- Choubisa SL, Mishra GV (2013) Fluoride toxicosis in bovines and flocks of desert environment. International Journal of Pharmacology and Biological Sciences 7(3): 35-40.
- Mehrotra M, Singh R (1989) Chronic fluorosis in a goat farm. Indian Journal of Animal Science 59: 808-810.
- Singh JL, Swarup D (1995) Clinical observations and diagnosis of fluorosis in dairy cows and buffaloes: case report. Agricultural Practices 16: 25-30.
- Gautam R, Bhardwaj N (2009) Fluoride accumulation in milk samples of domestic animals of Newa tehsil in Nagaur district (Rajasthan). The Ecoscane 3(3&4): 325-326.
- Gupta P, Gupta N, Meena K, Moon NJ, Kumar P, et al. (2015) Concentration of fluoride in cow’s and buffalo’s milk in relation to varying levels of fluoride concentration in drinking water of Mathura city in India - A pilot study. Journal of Clinical and Diagnostic Research 9(5): 5-7.
- Pradhan BC, Baral M, Prasad S, Pradhan D (2016) Assessment of fluoride in milk samples of animals of around Nalco Angul Odisha, India. The International Journal of Innovative Pharmaceutical Sciences and Research 4(1): 29-40.
- Raina S, Dua K, Singh S, Chhabra S (2020) Urine and milk of dairy animals as an indicator of hydrofluorosis. Journal of Animal Research 10(1): 91-93.
- Asembo EO, Oliech GO, Wambu EW, Waddams KE, Ayiekod PO (2021) Dental fluorosis in ruminants and fluoride concentrations in animal feeds, faeces, and cattle milk in Nakuru County, Kenya. Fluoride 54(2): 141-155.
- Wang JD, Zhan CW, Chen YF, Li J, Hong JP, et al. (1992) A study of damage to hard tissue of goats due to industrial fluoride pollution. Fluoride 25(3): 123-128.
- Choubisa SL (1996) Radiological skeletal changes due to chronic fluoride intoxication in Udaipur district (Rajasthan). Pollution Research 15(3): 227-229.
- Choubisa SL (2012) Toxic effects of fluoride on bones. Advances in Pharmacology and Toxicology 13(1): 9-13.
- Choubisa SL (2022) The diagnosis and prevention of fluorosis in humans (editorial). Journal of Biomedical Research and Environmental Sciences 3(3): 264-267.
- Choubisa SL (2022) How can fluorosis in animals be diagnosed and prevented (editorial)? Austin Journal of Veterinary Science and Animal Husbandry 9(3): 1096.
- Choubisa SL (2022) Radiological findings more important and reliable in the diagnosis of skeletal fluorosis (editorial). Austin Medical Sciences 7(2): 1069.
- Viswanathan GR (1944) Fluorosis of cattle in the Madras Presidency. Indian Journal of Veterinary and Animal Sciences Research 14(4): 239-242.
- Choubisa SL, Choubisa L, Sompura K, Choubisa D (2007) Fluorosis in subjects belonging to different ethnic groups of Rajasthan. Journal of Communicable Diseases 39(3): 171-177.
- Choubisa SL, Choubisa L, Choubisa D (2009) Osteo-dental fluorosis in relation to nutritional status, living habits and occupation in rural areas of Rajasthan, India. Fluoride 42(3): 210-215.
- Choubisa SL, Choubisa L, Choubisa D (2010) Osteo-dental fluorosis in relation to age and sex in tribal districts of Rajasthan, India. Journal of Environmental Sciences and Engineering 52(3): 199-204.
- Choubisa SL (2010) Natural amelioration of fluoride toxicity (fluorosis) in goats and sheep. Current Science 99(10): 1331-1332.
- Choubisa SL, Choubisa L, Choubisa D (2011) Reversibility of natural dental fluorosis. International Journal of Pharmacology and Biological Sciences 5(20): 89-93.
- Choubisa SL, Mishra GV, Sheikh Z, Bhardwaj B, Mali P, et al. (2011) Food, fluoride, and fluorosis in domestic ruminants in the Dungarpur district of Rajasthan, India. Fluoride 44(2): 70-76.
- Choubisa SL (2012) Osteo-dental fluorosis in relation to chemical constituents of drinking waters. Journal of Environmental Sciences and Engineering 54(1): 153-158.
- Sheikh Z (2011) Prevention of fluorosis in domestic animals. Current Science 10(9): 1124-1125.
- Choubisa SL (2013) Why desert camels are least afflicted with osteo-dental fluorosis? Current Science 105(12): 1671-1672.
- Choubisa SL (2014) Bovine calves as ideal bio-indicators for fluoridated drinking water and endemic osteo-dental fluorosis. Environmental Monitoring and Assessment 186(7): 4493-4498.
- Dwivedi SK, Dey S, Swarup D (1997) Hydrofluorosis in water buffalo (Bubalus bubalis) in India. Science of the Total Environment 207(2-3): 105-109.
- Trangadia BJ, Kaul PL, Patel BJ, Joshi DV, Kaul L (2015) Chronic fluorosis in buffaloes: clinic-pathological studies. The Indian Journal of Veterinary Pathology 39(4): 354-357.
- Samal UN, Naik BN (1992) The fluorosis problem in tropical sheep. Fluoride 25(4): 183-190.
- Swarup D, Dey S, Patra RC, Dwivedi SK, Lali S (2001) Clinico- epidemiological observations of industrial bovine fluorosis in India. Indian Journal of Animal Sciences 1(12): 1111-1115.
- Kalisinska E, Palczewska-Komsa M (2011) Teeth of the red fox Vulpes vulpes (L., 1758) as a bioindicator in studies on fluoride pollution. Acta Theriologica 56(4): 343-351.
- Sankhala SS, Harshwal R, Paliwal P, Agarwal A (2014) Toenails as a biomarker of chronic fluoride exposure secondary to high water fluoride content in areas with endemic fluorosis. Fluoride 47(3): 235-240.
- Death C, Coulson G, Kierdorf U, Kierdorf H, Morris WK, et al. (2015) Dental fluorosis and skeletal fluoride content as biomarkers of excess fluoride exposure in marsupials. Science of the Total Environment 533: 528-541.
- Choubisa SL, Choubisa A (2021) A brief review of ideal bio-indicators, biomarkers and determinants of endemic of fluoride and fluorosis. Journal of Biomedical Research and Environmental Sciences 2(10): 920-925.
- Patra RC, Dwivedi SK, Bhardwaj D, Swarup D (2000) Industrial fluorosis in cattle and buffalo around Udaipur, India. Science of the Total Environment 253(1-3): 145-150.
- Ghaffar S, Khan I, Ahmad MA, Umar T, Munir I, et al. (2020) Effect of fluoride on the physiology and growth indicators of maize (Zea mays ). Fluoride 53(3 Pt 2):491-498.
- Bulusu KR, Nawlakhe WG, Patil AR, Karthikeyan G (1993) Prevention and control of fluorosis: water quality and defluoridation techniques. In: Bulusu KR, Biswas SK (Eds.), Rajiv Gandhi National Drinking Water Mission, Volume II, Ministry of Rural Development, New Delhi, India, pp. 31-58.
- UNICEF (The United Nations International Children's Emergency Fund) (1999) State of the art report on the extent of fluoride in drinking water and the resulting endemicity in India. New Delhi: Fluorosis Research and Rural Development Foundation for UNICEF.
© 2023 Shanti Lal Choubisa. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






