- Submissions

Full Text
Clinical Research in Animal Science
The Prognosis with Mechanical Ventilation in Dogs and Cats
Yuki Uetsu*
North Shore Veterinary Specialist and Emergency Centre, Australia
*Corresponding author:Yuki Uetsu, North Shore Veterinary Specialist and Emergency Centre, 63 Herbert St, Artarmon, NSW 2064, Australia
Submission: April 28, 2023;Published: May 11, 2023
ISSN: 2770-6729Volume 2 - Issue 5
Abstract
Mechanical Ventilation (MV) is becoming increasingly available as a lifesaving tool in veterinary medicine. Informed decision-making is particularly important because of the labor intensity and the associated cost, and the prognosis is one of the major factors for the owner to consider. The overall survival rate with MV in heterogenous populations of dogs and cats was reported to be between 15-33%. However, this is widely varied depending on the underlying diseases process. Moreover, euthanasia accounted for a large proportion of non-survivors and the reasons potentially included financial aspects. This needs to be considered for interpretation of the results. MV from hypoxemic respiratory failure and patients with worse pulmonary function tended to have an unfavorable outcome, with the mortality rate of Acute Respiratory Distress Syndrome (ARDS), for example, up to 90%. However, patients with left-sided congestive heart failure had a better short-term outcome compared to other causes, likely because rapid improvement of pulmonary function is possible with pharmacological treatment. Patients with neuromuscular diseases such as tick paralysis and snake envenomation tended to have more favorable outcome compared to pulmonary disease because hypercapnic respiratory failure is more common. Pneumonia was the leading underlying disease for MV in puppies and brachycephalic dogs and survival rate of brachycephalic dogs might be lower compared to other breeds of dogs. The prognosis associated with the underlying causes should be the focus for the decision-making process rather than the general prognosis with MV. Moreover, further studies of ventilator strategies are required in dogs and cats which may give insights into improving patient outcomes.
Keywords:Mechanical ventilation; Dogs; Cats
Abbreviations:MV: Mechanical Ventilation; LSCHF: Left-Sided Congestive Heart Failure; ARDS: Acute Respiratory Distress Syndrome; VILI: Ventilator-Induced Lung Injury
Introduction
Mechanical Ventilation (MV) can be lifesaving and is becoming increasingly available in veterinary medicine [1]. MV is indicated in cases of; 1) severe hypoxemia despite oxygen therapy (hypoxemic or type 1 respiratory failure), 2) severe hypoventilation despite therapy (hypercapnic or type 2 respiratory failure), or 3) excessive respiratory effort with impending respiratory fatigue and failure [2]. While a growing number of articles have been published in the past decade, the evidence of MV in dogs and cats is still limited. Management of patients on MV can be challenging and requires intensive care and monitoring [2]. This increases the commitment of veterinarians, nurses and the owner as well as considerably increasing the associated cost. The appropriate informed consent, therefore, is particularly important for the management of MV cases. The purpose of this article is to review the available evidence of prognosis with MV in dogs and cats to help informed decision-making.
Discussion
The overall survival rate with MV in dogs and cats is generally poor and is reported to be 15-33% [3-6]. However, a large proportion of non-survivors were euthanized [4-6]. Due to the retrospective nature of the studies, the reasons for euthanasia could not always be determined; and thus, the financial reason could not be ruled out. Those studies found an association between higher PaO2:FiO2 (P: F) ratio and survival, which likely indicated that better lung function was associated with a higher chance for survival. Similarly, the survival rates were higher in cases with non-pulmonary disease compared to those with pulmonary disease, although this was not the case in the most recent study. The durations of MV between the disease groups were not different [3,4,6]. However, one study showed that animals with pulmonary disease had better outcome with the long-term (>24 hours) MV when compared to the short-term (<24 hours) MV [4]. Other reported prognostic factors are summarized in Table 1.
Table 1Reported factors associated with the outcome in each study in MV in dogs and cats. RF: Respiratory Failure, MV: Mechanical Ventilation; PIP: Peak Inspiratory Pressure, RR: Respiratory Rate, LSCHF: Left-Sided Congestive Heart Failure
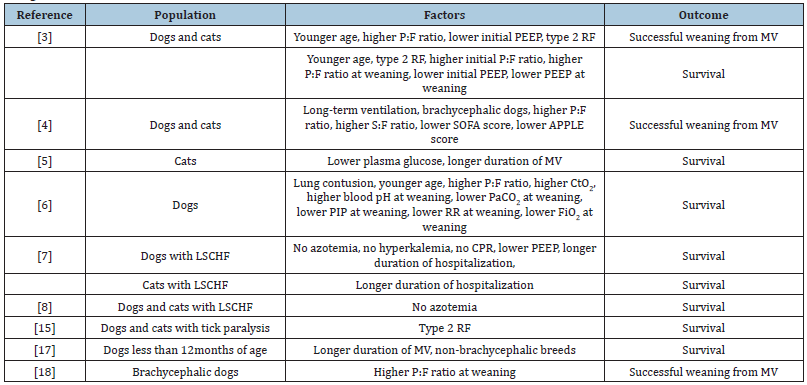
The studies examined thus far included heterogeneous populations with a variety of underlying diseases. Some other studies assessed more specific populations with MV. One study compared cardiac cause for MV with others [7]. The study revealed that the duration of MV was significantly shorter in Left-Sided Congestive Heart Failure (LCHF) patients compared to controls, which included all other diseases for the use of MV, and significantly higher proportion of patients from the LSCHF group survived to hospital discharge compared to the control group (54% VS 26%) [7]. An older case series of LSCHF on MV also showed a similar survival rate (62.5%) [8]. Pharmacological therapy for LSCHF, including diuretics, potentially allows rapid improvement of the pulmonary function; and therefore, could lead to shorter duration of MV, while other pulmonary diseases, such as ARDS and pneumonia, require longer duration for the lung condition to improve. On the other hand, the long-term survival was significantly longer in the control group compared to the LSCHF group [7]. This is likely because many patients in the control group had curable conditions such as pneumonia whereas those in the LSCHF group typically had chronic uncurable diseases.
Acute Respiratory Distress Syndrome (ARDS) has high mortality rates in both human and veterinary medicine and MV is an essential part of its management in humans [9-11]. In a recent retrospective study in dogs and cats, MV was recommended in 86% of cases, although the owner declined it in 43% of those cases and only 1 dog survived to hospital discharge among them [10]. Among those that received MV, only 19% managed to be weaned from MV [10]. The overall mortality rate of the study was 86% [10]. An older, smaller retrospective study reported a comparable mortality rate of 90% [11].
The neurotoxin from the salivary gland of I.holocyclus (‘paralysis tick’) in Australia is known to cause lower motor neuron signs and can lead to respiratory failure [12,13]. In a retrospective study in cats, MV was deemed to be required in 6% of cases, whereas such data is not available for dogs [14]. Eighteen percent of those that went on to MV, died in this study [14]. Another study investigated outcomes of MV in dogs and cats with tick paralysis and reported the overall mortality rate of 36.1%. However, 40.9% of those deaths were euthanasia because of financial reasons. Similar to other studies, hypoxemic respiratory failure had significantly lower survival rates compared to hypercapnic respiratory failure (52.6% vs 90.5% excluding euthanasia because of financial reasons, p=0.01) [15]. Snake envenomation can also cause hypercapnic respiratory failure and require MV. The median incidence requiring MV in snake envenomation was reported to be 13% and the survival rate with MV ranged between 66% - 91.7% depending on the geography and species of snake [16].
A study investigated the outcome with MV in dogs of less than 12 months of age. Pneumonia and non-cardiogenic pulmonary edema were the most common causes and composed more than 50% of cases. The survival rate in this study was 39% and was associated with the longer duration on MV [17]. Lastly, one study investigated outcomes in brachycephalic dogs requiring MV. This study found that brachycephalic dogs were more likely to be on MV when compared to non-brachycephalic breeds of dogs in ICU, with aspiration pneumonia being the most common pathology. The overall survival rate in this study was 27% and higher P:F ratio was associated with successful weaning from MV, which is comparable to pulmonary causes of other studies [18]. However, the aforementioned study in puppies showed lower survival rate in brachycephalic breeds than non-brachycephalic breeds [17].
The major limitation of these studies is the retrospective nature (1-18). Lung protective strategies of MV have developed over decades to prevent ventilator-induced lung injury (VILI) and the associated worse outcome in human [19]. Because of limited species-specific evidence, the strategy of MV in dogs and cats largely relies on human evidence as well as clinicians’ experience, with very few studies to evaluate whether this is appropriate in our patient population. In addition, to the author’s knowledge, there is no clinical study of VILI in dogs and cats. Many of the aforementioned studies reported ventilator setting variables [3-5,10,11,18]. However, due to the retrospective nature, no meaningful conclusion could be made. It is possible that certain MV strategies would improve the patient outcome and further studies are warranted to investigate this in our patient population.
Conclusion
The prognosis with MV in dogs and cats is generally poor. However, the prognosis is more largely related to the underlying disease process and likely associated with pulmonary function. This needs to be emphasized in discussion with the owner for decision-making rather than focusing on the general prognosis with MV. Further studies of ventilation strategies are warranted in dogs and cats.
References
- Vassilev E, McMichael M (2004) An overview of positive pressure ventilation. J Vet Emerg Crit Care 14(1): 15-21.
- Hopper K (2015) Basic Mechanical Ventilation. In: Silverstein DC, Hopper K (Eds.), Small Animal Critical Care Medicine. 2nd (edn), Elsevier Inc., St. Louis, Missouri, USA, pp: 161-165.
- Hopper K, Haskins SC, Kass PH, Rezende M, Aldrich A (2007) Indications, management, and outcome of long-term positive-pressure ventilation in dogs and cats: 148 Cases (1990-2001). J Am Vet Med Assoc 230(1): 64-75.
- Cagle LA, Hopper K, Epstein SE (2022) Indications and outcome associated with positive-pressure ventilation in dogs and cats: 127 cases. J Vet Emerg Crit Care 32(3): 365-375.
- Lee J a, Drobatz KJ, Koch MW, King LG (2002) Indications for and outcome of positive-pressure ventilation in cats: 53 cases (1993 – 2002). J Am Vet Med Assoc 226(6): 924-931.
- Bruchim Y, Aroch I, Sisso A, Kushnir Y, Epstein A, et al. (2014) A retrospective study of positive pressure ventilation in 58 dogs: Indications, prognostic factors and outcome. J Small Anim Pract 55(6): 314-319.
- Oppenheimer N, Kelmer E, Shwartzshtei N, Segev G, Ohad D, et al. (2022) Retrospective evaluation of the outcome and prognosis of undergoing positive pressure ventilation due to cardiac and noncardiac causes in dogs and cats (2019–2020): 101 cases. J Vet Emerg Crit Care 32(6): 769-776.
- Edwards TH, Coleman AE, Brainard BM, Defrancesco TC, Hansen BD, et al. (2014) Outcome of positive-pressure ventilation in dogs and cats with congestive heart failure: 16 cases (1992-2012). J Vet Emerg Crit Care 24(5): 586-593.
- Cairo JM (2020) Pilbeam’s Mechanical Ventilation Physiological and Clinical Applications. 7th (edn), Elsevier Inc., St. Louis, Missouri, USA.
- Boiron L, Hopper K, Borchers A (2019) Risk factors, characteristics, and outcomes of acute respiratory distress syndrome in dogs and cats: 54 cases. J Vet Emerg Crit Care 29(2): 173-179.
- Balakrishnan A, Drobatz KJ, Silverstein DC (2017) Retrospective evaluation of the prevalence, risk factors, management, outcome, and necropsy findings of acute lung injury and acute respiratory distress syndrome in dogs and cats: 29 cases (2011-2013). J Vet Emerg Crit Care 27(6): 662-673.
- Herndon AM, Thompson AT, Mack C (2018) Diagnosis and treatment of lower motor neuron disease in Australian dogs and cats. J Vet Med.
- Padula AM, Leister EM, Webster RA (2020) Tick paralysis in dogs and cats in Australia: treatment and prevention deliverables from 100 years of research. Aust Vet J 98(1-2): 53-59.
- Leister E, Morton J, Atwell R, Webster R (2018) Clinical presentations, treatments and risk factors for mortality in cats with tick paralysis caused by Ixodes holocyclus: 2077 cases (2008–2016). J Feline Med Surg 20(6): 465-478.
- Webster R, Mills P, Morton J (2013) Indications, durations and outcomes of mechanical ventilation in dogs and cats with tick paralysis caused by Ixodes holocyclus: 61 cases (2008-2011). Aust Vet J 91(6): 233-239.
- Morris CAD, Donaldson RE (2023) Mechanical ventilation in snake envenomation of dogs and cats. Front Vet Sci 10: 1071257.
- Lemieux E, Rozanski E, Buckley G, Chalifouxet N, Kennedy C, et al. (2021) Indications and outcomes for puppies undergoing mechanical ventilation: 59 cases (2006 to 2020). Can Vet J 62(8): 839-842.
- Hoareau GL, Mellema MS, Silverstein DC (2011) Indication, management, and outcome of brachycephalic dogs requiring mechanical ventilation. J Vet Emerg Crit Care 21(3): 226-235.
- Juffermans NP, Rocco PRM, Laffey JG (2022) Protective ventilation. Intensive Care Med 48: 1629-1631.
© 2023 Yuki Uetsu. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






