- Submissions

Full Text
COJ Reviews & Research
A Near Fatal Miss -Air Bag Related Polytrauma in a Child Presenting as Multiple Air Leaks & Odontoid Fracture
Ravi Sharma1*, Ajay Singh1, Tibin Johny1, Rajiv K Bansal1, Neeraj K Sharma2, Ajay Sharma2, Sanjay Narwani3, DP Sharma4 and Pradeep5
1Department of Pediatrics & Pediatric Intensive care, India
2Department of CTVS, India
3Department of ENT, India
4Department of Neurosurgery, India
5Department of Radiology, India
*Corresponding author: Ravi Sharma, Department of Pediatrics & Pediatric Intensive care, Jaipur, 302015, Rajasthan, India
Submission: August 02, 2021; Published: November 09, 2021
ISSN 2639-0590Volum3 Issue4
Abstract
Airbags have changed the pattern of fractures seen in road traffic accidents, reducing morbidity & mortality. However, in younger patients & patients of short stature who are sitting in front seat, severe spinal injuries can still occur even with deployment of airbags. Airbags related injuries can occasionally present with unusual presentations. The majority of airbags associated injuries are minor. We present a rare fatal manifestation of airbag related polytrauma in a 3-year-old male child presenting as lung contusion, air leaks & odontoid fracture presented as respiratory failure & unstable spine.
Keywords: Seat belt; Air bag; Neck injuries; Air leaks; Fatal; Child
Introduction
Airbags are inflatable sacs made up of nylon & aimed to provide a cushion to prevent the passenger hitting the steering wheel or any hard structure. During collision they expand within 0.5seconds at speeds approaching 200mph [1]. This can cause contusions & lacerations. Though airbags have reduced mortality & morbidity, severe spinal injuries can occur even with deployment of airbags. The majority of airbag associated injuries are minor. Wearing of seat belt have reduced serious injuries by 45% [2]. Together with seatbelt, airbags are now fitted as standard in many modern cars. Recent reports indicate that basic safety features such as airbags were not made mandatory on all cars in India until 2015 [3]. However, despite increase airbag implementation, there are not without complications. Many reports implicate airbags as the cause of injury. There is a zone of deployment for airbags, smaller 30-40liters deploy with much less force than larger (70l) available [4-6]. Timing is also crucial with the aim being for the passenger to strike the airbags once it is fully expandable& not in zone of deployment.
Case Report
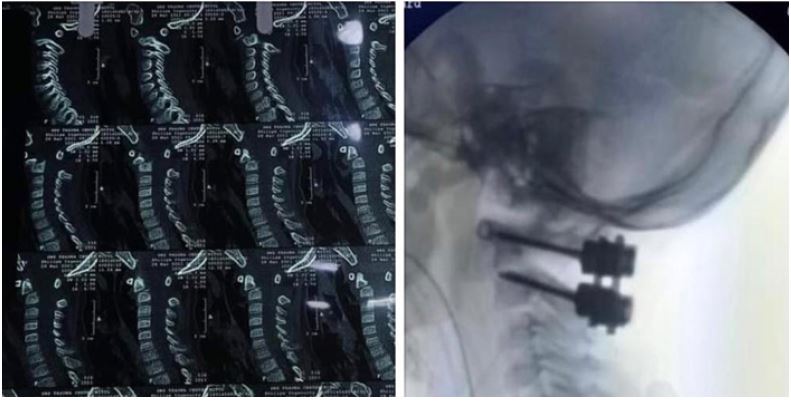
3-year-old male child presented with alleged airbag associated injury while patient being front seat unrestrained occupant & being hit by an electronic autorickshaw on the nondriver front door when car was standing at traffic signal. Patient suffered injuries from airbag & complained of neck pain & breathing difficulty. Patient went to nearby hospital where patient was intubated for respiratory failure(sp02 50% on NRM) .CT thorax done which showed no tracheal injury, bilateral pneumothorax, pneumomediastinum & surgical emphysema (Figure 1). Thereafter Patient was brought to our hospital emergency on Bain circuit with surgical emphysema over face, neck, thorax & upper abdomen, Heart rate of 170/min, Temperature 97.6F, poor perfusion, spo2 70% on Bain circuit, diminished air entry bilaterally, soft abdomen, S1, S2 muffled & agitated. Chest Xray showed pneumomediastinum with surgical emphysema (Figure 1). In view of air leak with desaturation even on Positive pressure ventilation, bilateral intercostals drainage inserted & air drained. Post ICD insertion spo2 increased to 99%. Patient resuscitated with fluid bolus for obstructive shock & hemodynamic monitoring started, x-ray pelvis & USG for trauma was normal, Functional echo showed limited window due to surgical emphysema, CT brain done which was normal, CT thorax showed bilateral lung contusion, pneumopericardium, surgical emphysema in chest wall & moderate pneumothorax, MRI orbits were normal. Patient started on sedation, paralysis, PRVC control mode of ventilation along with broad spectrum antibiotics & other supportive care. For anemia due to pulmonary hemorrhage patient treated with multiple aliquots of PRBC. For pulmonary hemorrhage optimal PEEP, vitamin K & inline closed suction used. After hemodynamic resuscitation vitals improved, patient neck examined for injuries. Hard age-appropriate Cervical collar was placed around neck for suspected cervical injury & MRI neck done which showed fracture in base of odontoid process (Figure 2) & grade 1 anterolisthesis, Atlantoaxial joint normal, Prevertebral hematoma is seen anterior to adontoid process, Edematous changes are seen in Prevertebral space with no spinal canal compression is seen& Spinal cord is normal in signal intensity and morphology. After stabilization of hemodynamic, neurosurgeon did reduction of odontoid process with posterior fixation on day 6th of hospitalization (Figure 3) along with Tracheostomy in view of anticipated prolonged intubation & unstable neck. Cervical collar continued and immobilization of neck was advised. Serial chest x-ray showed resolution of air leaks. Enteral feed was started, tolerated well and increased gradually. Patient weaned from ventilator & decannulated on day 21 of hospitalization. Chest & limb physiotherapy added. Intercostals tubes were gradually removed as child was stable and no drainage or air leak was seen. As child improved, limb physiotherapy was started, and supervised mobilization was done. Parents taught physiotherapy and neck movement precaution to be taken. Oral feed was started which child accepted well. Since child was clinically stable, accepting orally well, child discharged on day 25th day of hospitalization. Patient came after 3 month of injury walking with optimal range of movement over cervical spine.
Figure 1

Figure 2

Figure 3: Traumatic # Odontoid with AAD posterior C1-C2 fixation using lateral mass and transpedicular screw and rod.
Discussion
Life threatening Head & neck injuries resulting solely from airbag deployment are rare. However, in children they are more common. Children under 10 sitting in the front seat have a 10-34% increased risk of fatality when an airbag is deployed [7,8]. Age due to flexibility of atlanto occipital joint in addition to height is the determining factors. They have 87% increase of non-fatal injuries, many of these injuries occurred at low speeds. A fully restrained 7-year-old sitting in the front seat, involved in a low-speed collision. He sustained a 21mm atlantooccipital dislocation 8. Children are more at risk of atlanto-occipital dislocation. During precrash breaking, the child head is flexed forward into the inflating airbag. The combination of hyperextension & lateral flexion & anatomy of pediatric atlanto-occipital joint lead to increased susceptibility. 4-year-old sustained fatal injuries as a result of airbag deployment. The inflating airbags impacted the patient chin & face leading to hyperextension & complete dislocation of vertebral body at C2 [9]. Till now no case of airbag associated air leak with odontoid fracture being reported in literature. Our patient presented with multiple air leak leading to obstructive shock & respiratory failure requiring prolong ventilation, tracheostomy, cervical collar & definitive surgery for odontoid fixation.
Conclusion
Airbags alone have reduced morbidity & mortality by 19-50% [6,10-12]. Children under age of 13 years should be restrained in the back seat as it reduces their mortality rate [7-9,13-15]. Thus, airbag gives maximum safety with restraining. In unrestrained & front seat occupant, children are bound to have spinal injuries sometimes fatal. Severe damage can happen with slow speeds [8,9,16]. The pattern of injuries depends on type of air bag, velocity of impact, zone of deployment, height of patient, position of occupant & use of restraints [16].
References
- Globalpiasa (2009) Airbags are supplemental restraints and work best in combination with seatbelts.
- World Health Organisation (2015) Global status report on road safety.
- Moushumi DG, Sumant B (2014) Coming soon: new norms to make air bags must for all cars.
- Pearlman JA, Au Eong KG, Kuhn F, Pieramici DJ (2001) Airbags and eye injuries: Epidemiology, spectrum of injury, and analysis of risk factors. Surv Ophthalmol 46(3): 234-242.
- Cunningham K, Brown TD, Gradwell E, Nee PA (2000) Airbag associated fatal head injury: Case report and review of the literature on airbag injuries. J Accid Emerg Med 17 (2): 139-142.
- Christopher Noel B (2004) Maxillofacial and ocular injuries in motor vehicle crashes. Ann R Coll Surg Engl 86(3): 149-155.
- Danne P (2001) Serious injuries from airbags. ANZ J Surg 71(9): 507-508.
- Saveika JA, Thorogood C (2006) Airbag-mediated pediatric atlanto-occipital dislocation. Am J Phys Med Rehabil 85(12): 1007-1010.
- Buruk Y, Uzun I, Erkol Z, Agritmis H, Ustundag K (2010) Air bag-mediated fatalcraniocervical trauma: A case report. Ulus Travma Acil Cerrahi Derg 16 (4): 379-381.
- Francis DO, Kaufman R, Yueh B, Mock C, Nathens AB (2006) Air bag-induced orbital blow-out fractures. Laryngoscope 116(11): 1966-1972.
- Zaglia E, De Leo D, Lanzara G, Urbani U, Dolci M (2007) Occipital condyle fracture: an unusual airbag injury. J Forensic Leg Med 14 (4): 231-234.
- Francis D, Warren SA, Warner KJ, Harris W, Copass MK, et al. (2010) Sodium azide-associated laryngospasm after air bag deployment. J Emerg Med 39(3): 113-115.
- Stein JD, Jaeger EA, Jeffers JB (1999) Air bags and ocular injuries. Trans Am Ophthalmol Soc 97 (1): 59-86.
- Braver ER, Ferguson SA, Greene MA, Lund AK (1997) Reductions in deaths in frontal crashes among right front passengers in vehicles equipped with passenger air bags. JAMA 278 (17): 1437-1439.
- Perez J, Palmatier T (1996) Air bag-related fatality in a short, forward- positioned driver. Ann Emerg Med 28(6): 722-724.
- Boyd BC (2002) Automobile supplemental restraint system-induced injuries. Oral Surg Med Oral Pathol Oral Radiol Endod 94(2): 143-148.
© 2021 Ravi Sharma. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






