- Submissions

Full Text
COJ Nursing & Healthcare
Bridging the Gap: Using Healthcare Survey Data to Highlight Communication Gaps Between Primary Care and Ambulatory Care Settings
Angelina Vascimini1*, Andrew Tenpas2 and Stacey Curtis1
1Department of Pharmacotherapy and Translational Research, University of Florida College of Pharmacy, USA
2Department of Pharmacy Practice, Texas A&M University School of Pharmacy, USAA
*Corresponding author: Angelina Vascimini, Department of Pharmacotherapy and Translational Research, University of Florida College of Pharmacy, USA
Submission: April 27, 2024;Published: May 21, 2024

ISSN: 2577-2007Volume9 Issue1
Abstract
In order to ensure safe and optimized patient medication management, transitions of care must be a vital component of the healthcare process. However, medication safety extends beyond just times of transition, but similarly relies on effective and accurate communication regarding accurate medication lists. Many health systems do not communicate effectively, missing changes to medication lists that do not require a new prescription sent to the community pharmacist. Universally, successful care plan development and communication for a patient is creation of an effective interdisciplinary healthcare team. However, there is one interdisciplinary relationship that many times is not fostered, communication to the community pharmacists. The focus of this commentary is to address a gap in the literature and develop a more functional relationship between ambulatory care and community pharmacists.
Keywords:Communication; Community pharmacy; Ambulatory care; Patient safety
Abbreviations: MD: Doctor of Medicine; DO: Doctor of Osteopathic Medicine; NSAID: Nonsteroidal Anti-Inflammatory Drug; ACEi: Angiotenisin Converting Enzyme Inhibitor
Introduction
The roles and responsibilities of pharmacists have evolved significantly over the last decade or so [1]. The ambulatory care and community spheres, in particular, have witnessed several innovations, including chronic disease state management, broader immunization protocols, medication advisory services, comprehensive collaborative practice agreements, point-of-care testing, and increased recommendations by community pharmacists for minor ailments and conditions [2]. While these services add value to patient care, one critical component is missing: collaborative communication between ambulatory care and community pharmacists [3]. Recent studies have shown that lapses in communication negatively impact patient safety, quality of care, and overall health outcomes [4-6]. Conversely, clear and consistent communication between different pharmacy settings can improve detection of medication errors and even reduce hospital readmission rates [3-7].
Though nearly all healthcare professionals recognize the importance of effective communication across practice settings, significant barriers remain [8-10]. One common barrier relates to coordination outside of one’s own institution or practice setting; after all, it may require substantial time and effort to communicate across unconnected healthcare institutions or healthcare systems [11-14]. Moreover, communication regarding chronic disease state management and corresponding medication changes may be difficult within the ambulatory care space, especially when vital information is communicated solely to patients and caregivers and not to community pharmacists dispensing medications to those same patients [15-23]. Recent work suggests that other members of the healthcare team; including prescribers, nurses, and office managers, are in favor of greater collaboration and communication with pharmacists [20]. In one survey, over 90% of physicians wanted help ensuring that patients with multiple chronic conditions adhered to their care plans, though in yet another survey 27% of physicians attributed poor communication as one of the primary reasons why their patients mistrusted the healthcare system as a whole [24,25]. Clearly, considerable improvements in communication can and should be attempted by all parties.
This commentary article attempts to “bridge” these so-called gaps in communication by highlighting recent survey data obtained from physicians and medical assistants/nurses. We contend that, at present, communication within primary care is highly variable which, in turn, prevents consistent and clear communication between clinical or ambulatory care pharmacists and their retail or community counterparts. It is hoped that this survey data may call attention to and help to facilitate improvements in those relationships.
Discussion
As noted above, clear and consistent communication across healthcare systems is vital for safe and effective patient care [26]. To better understand how different members of the healthcare team convey prescription information to community pharmacists, surveys were distributed to physicians (MD/DO) and medical assistants/nurses in a small, rural family medicine clinic in Florida. These surveys were part of the primary author’s PGY2 residency research project, which was approved by the University of Florida Institutional Review Board. The project sought to determine how changes in prescription information were communicated from physicians and medical assistants/nurses to local community pharmacists. Surveys were administered electronically via RED Cap, a secure, IRB-approved web-based platform designed for data collection, storage, and analysis [12,13]. Only those who successfully completed the survey were included in the study. If desired, respondents were allowed to skip questions, though a two-week deadline was enforced for survey completion. Digital reminders were sent to participants approximately seven days after the introductory email.
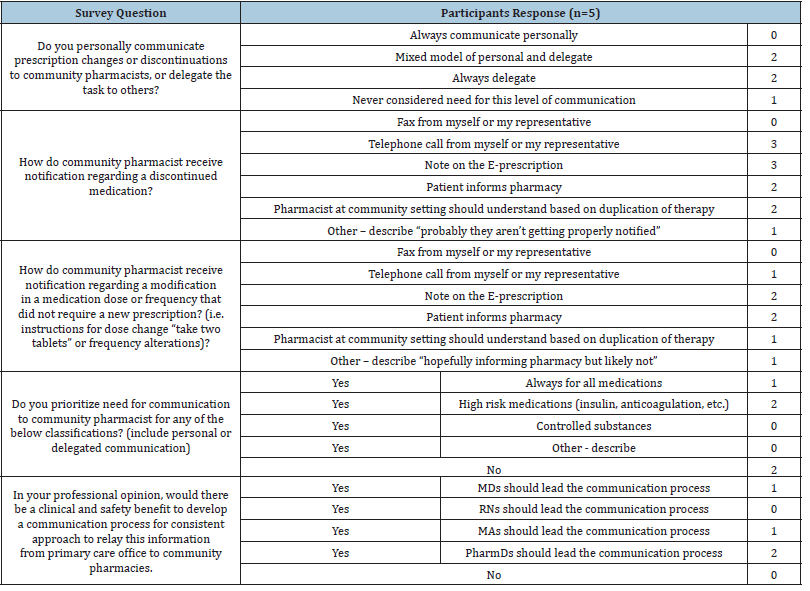
Survey data was divided into two cohorts. The response rate for the physician cohort was 83% (5/6 completed), while the medical assistant/nurse cohort exhibited a 67% rate (4/6 completed). An example of the Prescriber Survey can be found in Table 1. When asked about their customary communication method regarding prescription changes or discontinuations with community pharmacists, two physicians indicated that either they or a delegate personally called the pharmacy. Moreover, another two physicians always asked a delegate to spearhead communication, while a single prescriber admitted to never considering the importance of conveying such information to local community pharmacists.
Table 1:Prescriber survey example with results.
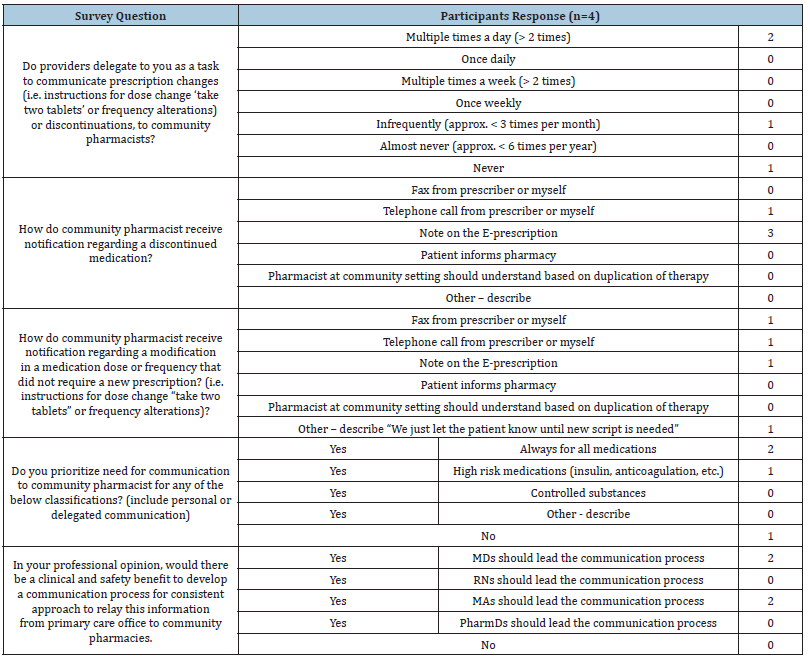
When asked how often prescription changes are communicated to community pharmacists, two medical assistants/nurses reported the frequency at more than twice daily, while two others admitted to once every three months or even never. When the same cohort was asked how vital information was conveyed to community pharmacists, 75% of medical assistants reported that details were embeded within “notes” attached to electronic prescriptions, which could be overlooked by pharmacy staff. More comprehensive results from the Medical Assistant Survey can be found in Table 2.
Table 2:Medical Assistant/Nurse Survey Results.
Conclusion
Recent literature has demonstrated improvements in patient care with increased communication between inpatient and outpatient spheres [3,14]. Despite its obvious benefits, there is little scholarship concerning processes to improve communication between ambulatory care and community pharmacists [16]. The aforementioned physician and medical assistant/nurse surveys support the need for more systematic communication methods between the two settings. As an example, each of the five physician respondents provided mixed or variable responses across all four sections of the survey. Additionally, preferred modes of communication varied significantly across the physician cohort, which further underscores the general lack of standardized communication between prescribers and community pharmacists. One prescriber even candidly admitted that “the pharmacies probably aren’t getting properly notified.” Likewise, two prescribers assumed that community pharmacists would intuitively understand when or why medication discontinuations were needed. Such assumptions are pernicious since approximately 25% of medication errors leading to patient harm occur in community pharmacies, where high prescription volume and inadequate pharmacist coverage are the strongest contributors [27,28]. Though studies suggest that nurses and pharmacists catch anywhere from 30-70% of medication-ordering errors, that still leaves a huge percentage of total errors unaddressed [29]. Surprisingly, only two physician respondents recognized the inherent risk of medications like insulin or anticoagulants and placed greater emphasis on clear communication with local pharmacies [30]. Since approximately 71% of drug-related hospitalizations in the United States are linked to drug classes like antiplatelets or anticoagulants, NSAIDs, diuretics, cardiovascular agents (e.g. B-blockers or ACE inhibitors), opioids, and antidiabetics, this implies that many prescribersincluding the ones surveyed here-may underestimate the dangers of seemingly “ordinary” prescription medications [31].
Results from the medical assistant/nurse cohort mirrored the variability seen in the physician cohort. Interestingly, none of the medical assistant/nurse respondents assumed that community pharmacists would intuitively understand when or why medication discontinuations were needed, while only one respondent placed greater emphasis on clear communication of high-risk medications with local pharmacies. Though these survey results are undeniably limited-reflective of a single rural family medicine clinic-they are nonetheless telling and potentially reflective of larger systemic issues. Further work is certainly needed; in the future, the authors hope to administer similar surveys at their respective practice settings and compare results with those listed above.
Ultimately, this commentary article was intended to call attention to a general lack of communication in primary care settings and the belief that interventions are sorely needed. Studies have repeatedly shown that communication gaps in healthcare can compound themselves into medication errors, therapeutic discrepancies, or adverse drug reactions farther downstream at local pharmacies [32]. We contend that development of and adherence to a consistent communication process between ambulatory care and community settings would pay immediate dividends, including increased accuracy of active medication lists, reduced medication errors, fewer drug interactions and adverse events, and improved patient care outcomes [33].
References
- (2023) The history of pharmacy, The Express Scripts Pharmacy Blog, Missouri, USA.
- Bertsch T (2023) The vital role of community pharmacists in today’s health care environment. Pharmacy Times, New Jersey, USA.
- Ozavci G, Bucknall T, Woodward-Kron R, Carmel Hughes, Christine Jorm, et al. (2021) A systematic review of older patients' experiences and perceptions of communication about managing medication across transitions of care. Res Social Adm Pharm 17(2): 273-291.
- Stauffer RL, Yancey A (2020) Impact of a pharmacy-driven transitions of care medication reconciliation following hospitalization. J Pharm Technol 36(2): 68-71.
- Shaver A, Morano M, Pogodzinki J, Stacy Fredrick, David Essi, et al. (2003) Impact of a community pharmacy transitions of care program on 30-day readmission rates. J Am Pharm Assoc 59(2): 202-209.
- (2013) ASHP-APhA medication management in care transitions best practices.
- Biscaldi L (2022) Clinical pharmacists value during transition of care evaluated. Drug Topics, New Jersey, USA.
- Report: A survey of healthcare leaders and patients, TigerConnect, California, USA.
- Pelletier D, Green-Demers I, Collerette P, Heberer M (2019) Modeling the communication-satisfaction relationship in hospital patients. SAGE Open Med 7: 2050312119847924.
- (2023) Social determinants of health data: Survey results on the collection, integration, and use, NORC at the University of Chicago, Chicao, USA.
- Vermeir P, Vandijck D, Degroote S, R Peleman, R Verhaeghe, et al. (2015) Communication in healthcare: A narrative review of the literature and practical recommendations. Int J Clin Pract 69(11): 1257–1267.
- Communication strategies in healthcare, The HIPAA Journal.
- (2020) Interpersonal communication in healthcare, Kognito, Massachusetts, USA.
- Impact of communication in healthcare, Institute for Healthcare Communication.
- Chui MA, Stone JA (2013) Exploring information chaos in community pharmacy handoffs. Res Social Adm Pharm 10(1): 195-203.
- Ilardo MA, Speciale A (2020) The community pharmacist: Perceived barriers and patient-centered care communication. Int J Environ Res Public Health 17(2): 536.
- Renfro CP, Robinson JM, Turner K, Gaskins T, Ferreri SP (2003) Care coordination and follow-up practices in the community pharmacy setting: A mixed methods study. J Am Pharm Assoc 60(4): 631-638.
- Smith MG, Ferreri SP, Brown P, Kristen Wines, Christopher M Shea, et al. (2017) Implementing an integrated care management program in community pharmacies: A focus on medication management services. J Am Pharm Assoc 57(2): 229-235.
- Spiro S, Quach D (2015) Interoperability: Plugging community pharmacy into the clinical data superhighway, Oncology Edition, Pharmacy Times, New Jersey, USA.
- Fay AE, Ferreri SP, Shepherd G, Kristin Lundeen, Gretchen L Tong et al. (2003) Care team perspectives on community pharmacy enhanced services. J Am Pharm Assoc 58(4S): S83-S88.
- Contreras B (2021) Healthcare leaders say lack of communication between prescribers, pharmacists is biggest issue in medication management, Managed Healthcare Executive, New Jersey, USA.
- Guthrie KD, Stoner SC, Hartwig DM, Justin R May, Sara E Nicolaus, et al. (2017) Physicians’ preferences for communication of pharmacist-provided medication therapy management in community pharmacy. J Pharm Pract 30(1): 17-24.
- Curran GM, Freeman PR, Martin BC, Benjamin S Teeter, Karen L Drummond, et al. (2019) Communication between pharmacists and primary care physicians in the midst of a US opioid crisis. Res Social Adm Pharm 15(8): 974-985.
- Powell S (2023) How to evaluate a chronic care management program for your practice.
- (2021) Surveys of trust in the US health care system. ABIM Foundation, NORC at the University of Chicago, Chicago, USA.
- (2020) The importance of clear, effective communication in healthcare, Hospital Housekeeping Systems (HHS), Texas, USA.
- Ledlie S, Gomes T, Dolovich L (2023) Medication errors in community pharmacies: Evaluation of a standardized safety program. Explor Res Clin Soc Pharm 9: 100218.
- Pervanas H, Revell N, Alotaibi AF (2016) Evaluation of medication errors in community pharmacy settings. J Pharm Technol. 32(2): 71–74.
- Tariq R, Vashisht R, Sinha A, Scherbak Y (2024) Medication dispensing errors and prevention, StatPearls Publishing, Florida, USA.
- High-risk medications, Humana, Kentucky, USA.
- Dreischulte T, Guthrie B (2012) High-risk prescribing and monitoring in patient care: How common is it, and how can it be improved? Ther Adv Drug Saf 3(4): 175–184.
- Branch J, Hiner D, Jackson V (2021) The impact of communication on medication errors. Patient Safety Network, Maryland, USA.
- Pharmacists’ impact on patient safety, American Pharmacists’ Association (APhA), Washington DC, USA.
© 2024 Angelina Vascimini. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






