- Submissions

Full Text
COJ Nursing & Healthcare
The Use of Reflection in Medication Administration in Nursing High School Students at a Higher Education Institution in Southern Puerto Rico
Rafael José Arroyo Torres*
Pontifical Catholic University of Puerto Rico, Puerto Rico
*Corresponding author: Rafael José Arroyo Torres, Pontifical Catholic University of Puerto Rico, Puerto Rico
Submission: May 06, 2022Published: October 31, 2022

ISSN: 2577-2007Volume8 Issue2
Abstract
Summary
In this article, we present the findings of a research that aimed to determine how the use of reflection contributes to the analysis of a real clinical situation of drug administration in high school students in nursing in an institution of higher education of southern Puerto Rico. Through an exploratory-descriptive design, through which qualitative data were collected to understand the problem posed, students enrolled in the last clinical course of a Bachelor of Science program in nursing participated. The results showed that reflection is a teaching strategy that allows observing clinical situations that occur in hospital environments, which facilitates the student to fragment the situation to analyze the actions, procedures, knowledge, attitudes and skills that are developed in it. The purpose is to train professionals capable of reflecting and proposing interventions or alternatives that result in safe practices of administration of medications and in a better quality of service provision to the patient. It was concluded that the analysis of a real clinical situation contributed to the reflection of the participants regarding the administration of medicines medication errors. Likewise, it was concluded that the use of the CARAC Reflective Model, designed by the researcher, contributed to help in the development of new skills and reflective behaviors in the participants. The recommendations raise the need to conduct more research and to encourage the use of reflective models in nursing academic training programs.
Keywords:Reflection; Medication administration; Nursing students; Reflective model; Medication errors
Introduction
A substantial amount of evidence from the international literature indicates the existence of a serious problem in the administration of medicines [1]. The National Coordinating Council for Medication Error Reporting and Prevention [2] defined a medication error as any preventable event that may cause or lead to improper use of medication or harm to the patient while the medication is under the control of the healthcare professional, patient, or the consumer. In the United States, it is estimated that medication errors will cost the Health System up to about 177,000 million dollars annually [3]. In Puerto Rico, there is Law No. 254 of December 31, 2015, known as the Law, to Regulate the Practice of Nursing in Puerto Rico [4]. This Law defines nursing as “the science and art of caring for the health of the individual, family, groups and community” (p.2). According to this Law, the practice of nursing is not only based on promoting and maintaining health, and preventing conditions, but also includes the realization of therapeutic measures. One of the therapeutic measures is the administration of drugs. Therefore, it is the generalist nurse who is responsible for carrying out these therapeutic measures as stipulated in the legal system.
For their part, Castro-González LV et al. [5], mentioned that the frequency of medication errors is high, so it has been necessary to strengthen and implement safety barriers in this process to reduce the risk of harm to the patient. Olsen J et al. [6] mentioned the 6 correct ones that guide the generalist nurse to reduce the mistakes that are made in the medication administration. These are: correct patient, correct medication, correcta route, correct time, correct dosage and correct documentation. The correct patient means that before the administration of medications, the nursing professional must check the identification of the patient using several identifiers. These identifiers are asking the patient to identify themselves by pronouncing their name aloud and checking that the identification bracelet matches the identification number. The right drug refers to a chemical that will act on physiological processes in the human body [7]. According to Hanson A et al. [8] the nursing professional must make sure that the drug to be administered is identical to the name of the drug that was prescribed.
Each drug has a generic name, a trade name, its uses and its side effects, which implies that the nurse has the responsibility to know them to administer the drugs correctly, (Craig, 2012). The correct route refers to the safe and correct administration of the drug according to the route established in the medical order, (Craig, 2012). Some routes of administration used are the oral, intramuscular, intravenous, otic, subcutaneous and rectal route, among others. On the other hand, the correct time means that the nurse must administer the drug as close as possible to the time because it can alter the bioavailability and / or other chemical mechanisms, according to Hanson H et al. [8]. The correct dose implies that the nursing professional must administer to the patient the exact dose of the drug according to the medical order, (Craig, 2012).
The nursing professional spends much of his or her workday managing medicines [9]. According to Wright K [10], these professionals must be able to perform accurate drug calculations to safely deliver medications to patients. Studies have shown that nurses do not always have the skills needed to calculate precise doses of drugs and are potentially administering incorrect doses of medication to their patients.
For McCabe D [11], the development of drug dosage calculation skills is part of the academic training of the nursing student. She added that it is important to examine this competence, since nursing professionals are usually the ones who administer the medications and serve them together with the patient and the family, being that moment the last opportunity for the prevention of errors. Despite the safety implications surrounding drug dosing and administration, there is little scientific evidence to guide best practices for teaching this competence, according to McCabe D [11].
Estrada-Zapata et al. [12] argued that, in order to develop critical thinking in the future training of nursing professionals, teaching-learning strategies must be used to encourage this thinking in students and, therefore, train autonomous professionals, empowered and capable of carrying out a reflective practice, which translates into a quality service towards the patient. In recent years reflection and reflective practice have acquired a great relevance in the academic training of nursing students [13]. The use of reflection as a technique reveals the areas of learning that need to be based on practice, as well as on the areas and situations in which it is necessary to reflect, (Rodríguez, Cárdenas and Blando, 2012). These authors added that reflection allows individualizing tutoring, both in academic and personal and professional needs. The Reflective Cycle designed by Graham Gibbs (1988) has a remediation component that aims to develop a corrective action plan. The combination of reflection and remediation is gaining momentum in nursing education to improve learning about medication dosage calculation, according to McCabe D [11].
Theoretical Framework
The research was guided by the principles of Taylor’s BJ [14] reflect reflective model (2006). The author defined the concept of reflection as the return of thoughts and memories in cognitive acts such as thought, contemplation, meditation and any other form of attentive consideration, in order to make sense of them and make contextually appropriate changes if necessary. For the author, this definition is an integral one and allows a wide variety of thoughts as a basis for reflection. He added that the health professionals “need help identifying and describing their workplace practices, in order to maximize what they do well and remedy those behaviors that need amendments and changes” (p.6). Taylor BJ [14] presented a model in the form of a globe surrounded by reflect bands and electrons orbiting around it. Figure 1 presents taylor’s reflect reflective model.
Figure 1:Reflective model reflect by Taylor BJ [14].
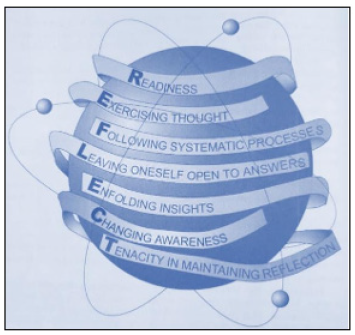
According to the author, the globe represents the world of practice where all the contextual characteristics are immersed within and acting on the environment in which she works. second, the author mentioned that reflect bands represent “the systematic flow of reflective processes in and through the practice world, preparing and reacting to the dynamic tension of your workplace” (p.63). For the author, the reflect process is represented as a to show the continuous links between the reflective processes that permeate human ideas in the sphere of practice. he added that the flow of reflective processes can vary in time, duration or timing in response to workplace circumstances or be directed intencionalmente by the person within the practice world, depending on the clinical problems of the work context and the internal or external limitations operating at a time. Dice. Taylor BJ [14] stated that “reflective processes occur within, through, around, and across the sphere of practice, taking reflective turns as they immerse themselves in clinical problems and out of them phenomena.
labor” (p.63). For the autora, the world of practice is not static or orderly, but constantly moves by turning to different points, changing shape within it due to its internal context and limitations, and evolving, distorting and flowing, due to external pressures and influences, limitations that constantly orbit, touch and sometimes collide with the sphere of practice. According to the author, the diagram represents the external limitations in structures that look like orbiting electrons.
The author mentioned that limitations are represented by neutrons in orbit [14]. For the author, the limitations include pressures and influences from multiple factors, among these: political, environmental, professional communities, social, economic, social, health patterns and initiatives, from general and global levels to specific levels. Taylor BJ [14], expressed that external limitations will always be present and will appear unpredictably in an unstable and sometimes chaotic external environment. According to the author, all external constraints are complex and interrelated, always present, sometimes unpredictably, in an unstable and often chaotic external environment.
He added that these processes are the means in the workplace that are identified and resolved to restore, maintain and possibly improve the overall integrity of the world of practice. Finally, the author ends by mentioning that the procesos of Reflection is not intended to be the remedy for all the challenges of practice. If not, let the reflect mnemonic device one of many ways to restore, maintain and enhance the so-called sphere of practice.
Methodology
The design used in this research is qualitative exploratorydescriptive. The population in this research was constituted by 33 students of 21 years or more, enrolled in the last clinical course of a Bachelor of Science in Nursing program of a higher education institution in southern Puerto Rico during the academic semester from August to December 2021. In this research, the sample consisted of 21 students of both sexes. For the purposes of this research, intentional sampling was used. According to Grove SK et al. [15], intentional sampling is one in which the researcher consciously selects certain participants, elements, events, or incidents to include in the study.
To collect the data of the variables of this research, we used the instrument entitled: Reflexive Model CARAC, developed by the researcher. To validate the research instrument, content validity was used by a panel of experts. According to Ponce O [16] a content validity refers to the fact that the instrument appears to measure what the researcher is trying to measure. The expert panel was composed of five professionals with a doctor’s degree: three experts in nursing and curriculum and teaching; one expert in nursing and educational management; and a nursing expert.
The instrument is composed of three parts. The first part corresponds to the sociodemographic data of the participants: age, sex, town of origin, residential area and whether you are currently employed. The second part of the instrument consists of a reflective sheet on a real clinical situation related to the administration of drugs at the Vibra Hospital of Sacramento, located in California, United States. The reflective sheet was used by the participants to answer the questions of the third part of the instrument. The CARAC Reflective Model consists of four parts: Prior Knowledge, Analysis, Reflexion of Experience and Corrective Actions, with a series of questions that guide students to reflect on the real situation.
Findings and Discussion
For this exploratory-descriptive qualitative research, the following research question was established: How does the use of reflection contribute to the analysis of a real clinical situation of drug administration in nursing high school students at a higher education institution in southern Puerto Rico? To answer this question, a research instrument entitled CARAC Reflective Model, developed by the researcher, was used.
The emphasis of the discussion of the findings was based on three of the phases of the CARAC Reflective Model: Analysis, Reflection of experience and Corrective Action, since the researcher considers that these phases contribute to answering the research question.
Analysis Phase
The questions of the research instruments 3, 4 and 5 belong to the Analysis phase of the CARAC Reflective Model. The findings of the questions from this phase are discussed below.
Question 3 of the instrument
What medication errors are present in the actual clinical situation?
When analyzing the codifications of the answers of each participant, the findings revealed that the codes that prevailed the most were: administration of the undiluted drug, did not read the medical order, did not perform double comparison with another nurse, ignorance, did not follow the policy or protocol of the hospital and did not consult in case of doubts or errors. In this regard, participant #5 stated “The nurse administered 4 milligrams of the undiluted medication. The enfermera did not read the medical order.” Similarly, participant #8 expressed “The nurse did not dilute the medication and administered it IV push.” Similarly, participant #15 mentioned “The nurse did not know about the medication or the use, nor the management, nor the route, she did not use the protocol of the institution, she did not ask another colleague. Medications like that should be administered between 2 nurses. The results of this research are consistent with a research conducted by Gracia JE et al. [17], in which it was found that the main areas of risk of errors in the administration of drugs were in dilution, concentration and infusion rate of the medication. In the same study it was found that nurses have a low level of knowledge of the drugs they use the most and with which a greater number of medication errors are made.
Question 4 of the instrument
What actions did the nursing professional carry out in the face of the errors identified in the administration of the drug?
When analyzing the codings of the answers of each participant, it is clear that the most frequent codes were: the double comparison with another nurse was not carried out, activation of the green code, did not apply the correct ones in the administration of medicines, did not follow the policy or protocol of the hospital, did not read the medical order and did not consult in caso of doubts or Errors. In answering the question, participant #1 stated that “He did not read the medical order, and claimed not to have administered Levoped before, did not investigate the medication, and did not ask another nurse to check and sign him to give the medication.” Similarly, participant #9 indicated that “He administered the drug without knowing its action, use, intervention and interaction. He did not follow the 7 correct or protocols of the hospital institution before the administration of medicines. He did not interpret the medical order. He did not use the correct route or dose (by not diluting it in dextrose according to medical order) He did not use the time or the correct frequency.”
According to the findings of this research, they concur with those of Santi et al. [18] in Brazil, in which they found that workers associate medication error with multifactorial causes and, as factors that influence the error, they cite the illegible handwriting, talks in the medication room, work overload, lack of attention, lack of identification of the patient, stretcher, medication, time and route.
Question 5 of the instrument
What was the outcome of the situation?
When performing an analysis on the participants’ answers to question 5, the data reveal that the codes that prevailed the most were: death of the patient, cardiorespiratory arrest with ventricular fibrillation and activation of the green code. In this regard, participant #15 responded “Once the nurse administered the medication, the patient presented cardiorespiratory arrest, with ventricular fibrillation, from which he did not survive, despite the fact that the green code process was carried out.” Similarly, participant #9 expressed “Improper administration led to cardiorespiratory arrest with ventricular fibrillation.
A green code of 24 minutes without response and in which the patient did not survive.”
According to the findings of the present research, it is clear that the results concur with what was expressed by Tiziani A [19] who mentioned that among the side effects are arrhythmias, palpitations and severe retrosternal pain. Similarly, the findings concur with those of Martín C et al. [20] in France, who concluded that the mortality rate reached 90% in those patients receiving more than 1μg/kg per minute of norepinephrine.
Reflection Phase of the Experience
The questions of research instruments 6 and 7 belong to the Reflection phase of the EXPERIENCE of the CARAC Reflective Model. The findings of the questions from this phase are discussed below.
Question 6 of the instrument
Why did the errors in the administration of the drug occur?
The codes that most prevailed when analyzing the answers of the participants were: did not read the medical order, ignorance, did not consult in case of doubts or errors, did not follow the policy or protocolo of the hospital, did not apply the correct ones in the administration of medications, did not perform double comparison with another nurse and lack of attention and/or concentration. In this regard, participant #9 indicated “Not being sure of a medication, it is essential that the nurse corroborates the information and clarifies her doubts to avoid a bad practice. The nurse did not follow the correct 7, did not verify the information or use a double check with another nurse. “On the other hand, participant #15 responded “The errors in the administration of the drug occurred because the nurse in charge did not follow the correct process. He confessed to not knowing anything about the drug and did not read the medical order correctly.”
According to the findings of the research, the results concur with those of Santi et al. [18] in Brazil, who concluded that workers associate medication error with multifactorial causes. Similarly, the findings agree with those of Gracia JE et al. [17], who concluded in their research that nurses have a low level of knowledge about the drugs that they use the most and with which a greater number of medication errors are made .
Question 7 of the instrument
What interventions should the nursing professional have performed while administering medications
When analyzing the data of the participants, the findings revealed the codes that most prevailed, these were: use of the correct ones in the administration of medications, consult in case of doubts or errors, read and interpret correctly the medical order, perform double comparison with another nurse, evaluation of the client’s answers and verify or take the vital signs.
In this regard, participant #1 indicated “Check for sudden changes in the patient.” Similarly, participant #4 said “The nurse should have consulted her questions about the medication with another nurse and if she thought that the order might be wrong, consult with the doctor the dose when administering. Also having seen that the machine warned him that the drug was diluted and follow the protocol of the hospital. “Participant #15 replied “The interventions that the nurse had to perform while administering the medications was to compare the instructions of how the drug was administered and talk to another nurse for the correct administration since she had no knowledge about how it was administered.” In turn, participant #12 indicated “Read the medical order and interpret it correctly, follow the correct 7 and reflect and recognize that I had doubts in the administration and not administer until I was safe and assisted by another partner.”
According to the findings of the present research, the results concur with those of Nathaly RR et al. [21] where it was found, among other things, lack of pharmacological safety round with patients of high pharmacological risk in a third-level hospital. Similarly, the findings concur with those of Armitage G [22] who concluded that double verification can be useful if it is implemented according to a multidisciplinary, systematic and efficient process. In addition, the findings agree with what was expressed by Olsen J et al. [6], who mentioned that to reduce the errors that are commented on in the administration of medications, nursing professionals are guided by the correct six of the medication administration. However, they contrast with the findings of Alsulami Z et al. [23] in England, who reported that clinical trials are required to establish whether double checking of drugs is effective in reducing medication errors.
Corrective Action Phase
The questions of research instruments 8 and 9 belong to the Corrective Action phase of the CARAC Reflective Model. The findings of the questions from this phase are discussed below.
Instrument question 8: From you encountering a similar clinical situation
How would you develop the skills required by the health institution as a future nursing professional?
In this research it was found that the codes with the highest prevalence according to the students’ answers to question 8 were: knowledge about the policy or hospital protocol, consult in case of doubts or errors, read and correctly interpret the medical order, understanding of basic and advanced skills before executing the practice of medication administration and use of correct medication administration. Participant #8 replied that “I would focus on the right 7, and if I didn’t know something about the medication, I would corroborate it with another professional.” In the same way, participant #1 expressed that “If I find myself in a situation like this, I would take care of strictly reading the medical order, I would not proceed to administer a medication that I do not know, I would call the doctor to corroborate that I am reading the medical order well, I would ask for help from the companions. I would check if the medicine is already diluted or needs to be diluted. I would take all necessary measures before harming the patient’s life.” For his part, participant #13 indicated that “As a future nursing professional, the training of part of the institution is important to be able to know the policies of case management in different scenarios, additional reading and ensuring the understanding of basic and advanced skills before execution.”
According to the findings of the present research, it is clear that the results concur with those of Pereira, Pereira C et al. [24] in Brazil, who concluded that 75% of nursing graduate students would seek guidance regarding the behavior of the future professional regarding medication error. Similarly, they concur with the findings in Brazil presented by Franco da Silva et al. [25], who concluded that there is a need to invest in the continuous training associated with the computerization of care processes, as a strategy for the substantial reduction of medication errors.
Instrument question 9: If in a real scenario you encounter this situation
how would you make it different?
According to the analysis of the participants’ answers to question 9, the findings indicated that the codes that prevailed the most were: consult in case of doubts or errors, read and correctly interpret the medical order, use of the correct ones of the administration of medicines, training, double comparison of another nurse, knowledge of the policy or hospital protocol and avoid causing harm to the patient. Regarding this, participant #5 stated that “I would read and interpret the medical order in conjunction with a partner, consult the order with the doctor and reflect on my strengths and weaknesses and seek help if I have doubts. I would follow the correct 7, check the protocol of the institution and compare the order to see if I am correct. I would assess vital signs earlier, as all protocols state.” Similarly, participant #19 replied “If I had encountered this situation, I would do everything as it has to be, I would use the right 10, even if I am late, but I make sure that I am taking the correct technique and thus make sure I do not make medication errors.” On the other hand, participant #15 indicated “I would first read the medical order and if I did not understand it I would consult with a partner. In case I do not know how to administer the medication, I talk to my companion to show me how to perform the administration.”
According to the findings of this research, the results concur with those of Santi et al. [18] in Brazil, who concluded that nursing professionals should use the correct medication to guide their actions. Similarly, the findings concur with the Walsh LJ et al. [26] in Canada, who concluded that professional socialization, in combination with supportive learning environments, can increase students’ comfort in reporting medication errors.
Research question
How does the use of reflection contribute to the analysis of a real clinical situation of medication administration in nursing high school students at a higher education institution in southern Puerto Rico?
Reflection is a teaching strategy that allows observing clinical situations that occur in hospital environments, which makes it easier for the student to fragment the situation to analyze the actions, procedures, knowledge, attitudes and skills that are developed in it. The purpose is to train professionals capable of reflecting and proposing interventions or alternatives that result in safe practices of administration of medicines and in a better quality of provision of services to the patient. This argument reaffirms the approaches of Mann, Gordon and MacLeod (2009), since they argue that reflection is a significant and valuable technique in the training of nursing professionals.
Similarly, he agrees with Barksby J et al. [27], in that the use of a Reflecting model can help students focus on learning and selfawareness after an incident and avoid simply recommitting the events. In addition, it is consistent with the approaches of Lestander O et al. [28], in which the use of a reflection model fosters a clear and effective appreciation of communication. And finally, this argument reaffirms the approach of Taylor BJ [14] who argues that when concepts and ideas are complex, it is necessary to fragment them into parts so that they are manageable.
Conclusion and Recommendation
After the analysis of the data, the researcher established in his conclusions, that the analysis of a real clinical situation contributed to the reflection of the participants regarding the administration of medications, especially medication errors. Finally, the researcher concluded that the use of the CARAC Reflective Model, designed by the researcher, contributed to help in the development of new skills and reflective behaviors in the participants.
The researcher presented recommendations for educational institutions that offer degrees leading to the baccalaureate in nursing. Among the recommendations were: Replicate research in other higher-level institutions in other geographic areas of Puerto Rico; Conduct new research using the technique of reflection in the teaching and learning process of high school students in nursing to enrich the curriculum; Using the CARAC Reflective Model to encourage reflection in nursing baccalaureate students regarding medication administration, especially medication errors; Train the faculty of nursing in the use of reflection through workshops and trainings; and, Develop instructional units based on the analysis of clinical situations through the use of reflection.
Research Contribution
The researcher contributes to the field of nursing education the first research carried out in Puerto Rico with the variables reflection and administration of medications with students of bachelor’s degree in nursing. Finally, the researcher supported the research instrument, the CARAC Reflective Model, which can be used to encourage the reflection of high school students in nursing regarding the administration of medications, with the use of a real clinical situation.
References
- Aspden P (2006) Institute of medicine committee (USA) on the identification and prevention of medication errors. Error Prevention Medicatión, National Academies Press, Washington DC, USA.
- National coordinating council for medication error reporting and prevention (2022) About medication errors: What is a medication error?
- Lynch S (2009) Medication errors. MSD Manual.
- (2015) Law 254 of December 31, 2015, Law to regulate the practice of nursing in Puerto Rico, USA.
- Castro-González LV, Martínez-Contreras AM, Caro VJ, Barreras-Serrano A, Dautt-Silva J (2020) Medication errors in patients hospitalized in the Internal Medicine service. Med Int Mex 36(6): 751-758.
- Olsen J, Giangrasso A, Shrimpton D (2015) Medical dosage calculations, Pearson Prentice Hall, New Jersey, USA.
- Olsen J, Giangrasso A, Shrimpton D, Dillon P (2008) Medical dosage calculations, Pearson Prentice Hall, New Jersey, USA.
- Hanson A, Haddad LM (2020) Nursing rights of medication administration. StatPearls Publishing, Florida, USA.
- Martinez V (2021) Prevention of medication errors in nursing. Editorial Océano SL, Barcelona, Spain.
- Wright K (2008) Can effective teaching and learning strategies help student nurses to retain drug calculation skills? Nurse Education Today 28(7): 856-864.
- McCabe D (2016) Enhancing medication safety teaching through remediation and reflection. Quality and Safety Education for Nurses, Case Western Reserve University, Ohio, USA.
- Estrada-Zapata, Katherinne (2019) Critical thinking: Concept and its importance in nursing education. Nursing Index 28(4): 204-208.
- Cárdenas BL, Monroy RA, Arana GB, García ML (2014) Importance of reflective and critical thinking in nursing. Mexican Journal of Cardiological Nursing 23(1): 35-41.
- Taylor BJ (2006) Reflective practice: A guide for nurses and midwives. (2nd edn), McGraw-Hill, New York, USA.
- Grove SK, Gray JR (2019) Nursing research: Development of evidence-based nursing practice. (7th edn), Elsevier, Barcelona, Spain.
- Ponce O (2006) Writing of research reports. Puerto Rican Publications, Hato Rey, Puerto Rico, USA.
- Gracia JE, Serrano RB, Garrido JF (2019) Medication errors and drug knowledge gaps among critical-care nurses: A mixed multi-method study. BMC Health Serv Res 19(1): 640.
- Santi, Beck, da Silva, Tonel, do Reis, et al. (2014) Medication error in a university hospital: Perception and related factors. Global Nursing 13(35): 160-171.
- Tiziani A (2018) Harvard drugs in nursing. Modern Manual (5th edn), pp. 614-615.
- Martín C, Medam S, Antonini F, Alingrin J, Haddam M, et al. (2015) Norepinephrine: Not too much, too long. Shock: Injury, Inflammation, and Sepsis: Laboratory and Clinical Approaches 44(4): 305-309.
- Nathaly RR, Santacruz RM, Escobar Espinosa SB (2013) Prevalence of errors in the use of medicines in patients of high pharmaceutical risk and analysis of their potential causes in a hospital entity. Global Nursing 12(32): 171-184.
- Armitage G (2008) Double checking medicines: Defence against error or contributory factor? Journal of Evaluation in Clinical Practice 14(4): 513-519.
- Alsulami Z, Conroy S, Choonara I (2012) Double checking the administration of medicines: What is the evidence? A systematic review. Archives of disease in childhood 97(9): 833-837.
- Pereira C, Pereira O, Carboni R (2010) Conduct of the future nurses in the perspective of medication error. Revista de Enfermagem UFPE: Online 4(1): 118-123.
- Franco da Silva E, De Faveri F, Lorenzini L (2014) Medication errors in nursing practice: An integrative review. Global Nursing 13(34): 330-337.
- Walsh LJ, Anstey AJ, Tracey AM (2018) Student perceptions of faculty feedback following medication errors-A descriptive study. Nurse Education in Practice 33: 10-16.
- Barksby J, Butcher N, Whysall A (2015) A new model of reflection for clinical practice. Nursing Times 111: 21-23.
- Lestander Ö, Lehto N, Engström Å (2016) Nursing students perceptions of learning after high fidelity simulation: Effects of a three-step post-simulation reflection model. Nurse Education Today 40: 219-224.
© 2022 Rafael José Arroyo Torres. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






