- Submissions

Full Text
COJ Nursing & Healthcare
Same Country, Different Realities: The Detection of Congenital Defects at Birth in Brazil Between 2008 and 2018
Victória Machado Scheibe1*, Amanda Maria Schmidt1*, Lara Helena Zortéa1, Gabriella Zanin Fighera1, Gustavo Matas Kern1, Augusto Mädke Brenner2 and Bibiana Mello de Oliveira3,4
1School of Medicine, Universidade Luterana do Brasil, Brazil
2School of Medicine, Universidade Federal de Ciências da Saúde de Porto Alegre, Brazil
3Post-Graduation Program in Genetics and Molecular Biology, Brazil
4Hospital Santa Casa de Misericórdia, Brazil
*Corresponding author: Victória Machado Scheibe and Amanda Maria Schmidt, School of Medicine, Universidade Luterana do Brasil, Brazil
Submission: January 28, 2022Published: September 15, 2022

ISSN: 2577-2007Volume8 Issue2
Abstract
Congenital defects are defined as structural or functional abnormalities that occur during embryonic development. In Brazil, it is estimated that 2 to 5% newborns have congenital defects. This study aims to characterize newborns with congenital defects at birth, evaluating the association with pre- and perinatal factors in comparison with newborns without these defects. A retrospective descriptive epidemiological study based on data from the Information System on Live Births between 2008 and 2018. In the period, 32,124,447 live births were reported in Brazil; of this total, 225,561 had congenital defects identified at birth. The detection of these anomalies was significantly more frequent among the maternal age group from 45-49 years old; mothers with ≥12 years of schooling; legally separated mothers; mothers who had -3 prenatal visits; premature pregnancies of 28-31 weeks; triplet pregnancies or more; women who underwent cesarean delivery; yellow color; male sex; newborns with a 5’ Apgar score 0-2 and with very low birth weight (P<0.0001). The results of this study suggest a progressive increase of congenital defects cases in the country over the years, although it still points out possible underdiagnosis and underreporting, highlighting the need for interventions for adequate and early recognition of congenital defects.
Keywords: Congenital defects; Infant; Public health; Brazil; Perinatal care
Keywords:CD: Congenital defects; SINASC: Sistema de Informações sobre Nascidos Vivos; DATASUS: Departamento de Informática do Sistema Único de Saúde, CEP-CONEP: Research Ethics Committees-National Research Ethics Commission; DNV: Declaration of Live Births; ICD-10: International Classification of Diseases; ECLAMC: The Latin American Collaborative Study of Congenital Malformations; OCD: Osteo Condro Displasias; SIAT: National System of Information on Teratogenic Agents; ICBDSR: International Clearinghouse for Birth Defects Surveillance and Research; EUROCAT: European Registration of Congenital Anomalies and Twins; BINOCAR: British and Irish Network of Congenital Anomaly Researchers; RD: Rare Diseases
Introduction
Congenital Defects (CD) are defined as structural, functional or metabolic abnormalities that occur during embryonic development. They can be related to genetic, environmental-such as infections and exposure to toxic agents during pregnancy-or multifactorial causes [1]. Structural defects can be divided into four main groups: malformations, disruption, deformity and dysplasia [2]. Malformations are a type of CD in which the developing tissue was not formed correctly from the early stages, in other words, it is a consequence of a defect inherent to the affected tissue or organ with permanent changes [3-4]. Malformations can also occur due to agenesis or hypogenesis (non-development or underdevelopment of the structure, respectively) [3]. In addition, the malformations can be classified into major or minor, according to the clinical impact [4- 5]. Disruption, on the other hand, is defined as the destruction or alteration of already formed structures-previously normal during fetal development [4]. Deformity can be understood as a change in the shape, contour or position of an organ. Dysplasia is identified as the abnormal organization of cells in specific tissues, which can lead to changes in shape [5]. Moreover, the sequences are a pattern of related CD already known to be derived from a single primary anomaly, that is, a single event causes a cascade of effects that generate other CD [6].
Environmental factors, such as gestational exposure to some infectious agents, drugs and alcohol, correspond to 5 to 10% of CD [5,7]. Additionally, some maternal diseases can also be related to congenital malformations, such as gestational or previous Diabetes Mellitus, which is responsible for around 6% of these occurrences, and folic acid deficiency, both well-known preventable risk factors for the development of CD [5,7]. Genetic factors correspond to approximately 30 to 40% of cases of malformations [2,5,8,10]. Annually, approximately 8 million children are born worldwide with some CD, representing about 6% of these births [11]. The general incidence of CD in Brazil is not very different from that presented in the world [12]. In Brazil, it is estimated that around 2 to 5% of live births have CD [12-13]. Infant mortality is an important health indicator, as it is associated with factors such as maternal well-being, quality and access to health services, socioeconomic conditions and public health practices [13]. Studies in developed countries have shown that around 70% of congenital malformations can be prevented or have their disabilities minimized [14]. Therefore, population surveillance of these births is necessary to monitor changes in the pattern of anomalies [7]. This study aims to characterize the population of neonates with CD identified at birth in Brazil from 2008 to 2018, assessing the association with pre-and perinatal factors and comparing to those newborns who had no identified CD.
Materials and Methods
A retrospective descriptive epidemiological study was conducted to analyze the profile of newborns with CD identified at birth in Brazil between 2008 and 2018. The pre-and perinatal variables were compared with the population of live births without reported CD in the same period. The data, available at the Sistema de Informações sobre Nascidos Vivos (SINASC) on the platform of the Departamento de Informática do Sistema Único de Saúde (DATASUS), were collected with the aid of TABWIN (guide for Windows) and TABNET (guide for internet) Softwares. Information considered ignored were quantified, but were not considered in the comparative analyses. Research involving public domain data without identification, such as SINASC, does not need approval by the system CEP-CONEP (Research Ethics Committees-National Research Ethics Commission) according to National Healthcare System (Conselho Nacional de Saúde - CNS) 510/2016 resolution [15].
DATASUS, SINASC e DNV
DATASUS was founded in 1991 and is responsible for supplying the entities of Brazil’s Unified Health System (Sistema Único de Saúde - SUS) about information systems, data collection, and computerized support. This department manages the knowledge of health indicators [16-17]. In 1990, SINASC was implemented to aggregate epidemiological information regarding births notified throughout the national territory. SINASC collects and provides information on births, maternal data, pregnancy, delivery and newborn, making it possible to know the profile of live births in Brazil. The system depends on the information obtained from the DNV (Declaration of Live Births). Since 1990, there is a field in the DNV to describe all the CD observed in the newborn. All CD must be registered following the International Classification of Diseases (ICD-10). It should be noted that any CD detected after filling the DNV are not computed by SINASC [17-20].
Statistical analyses: Microsoft Excel and SPSS version 26.0 were used for the data collection and analysis. Categorical variables are presented as frequencies and percentages, and continuous variables as rates, means and standard deviations (±SD). To assess the existence of an association between the studied variables, correlations were made through the analysis of odds ratios, with a 95% confidence level (p≤0.05). Linear regression analysis was performed, with statistical significance calculated by Anova.
Result and Discussion
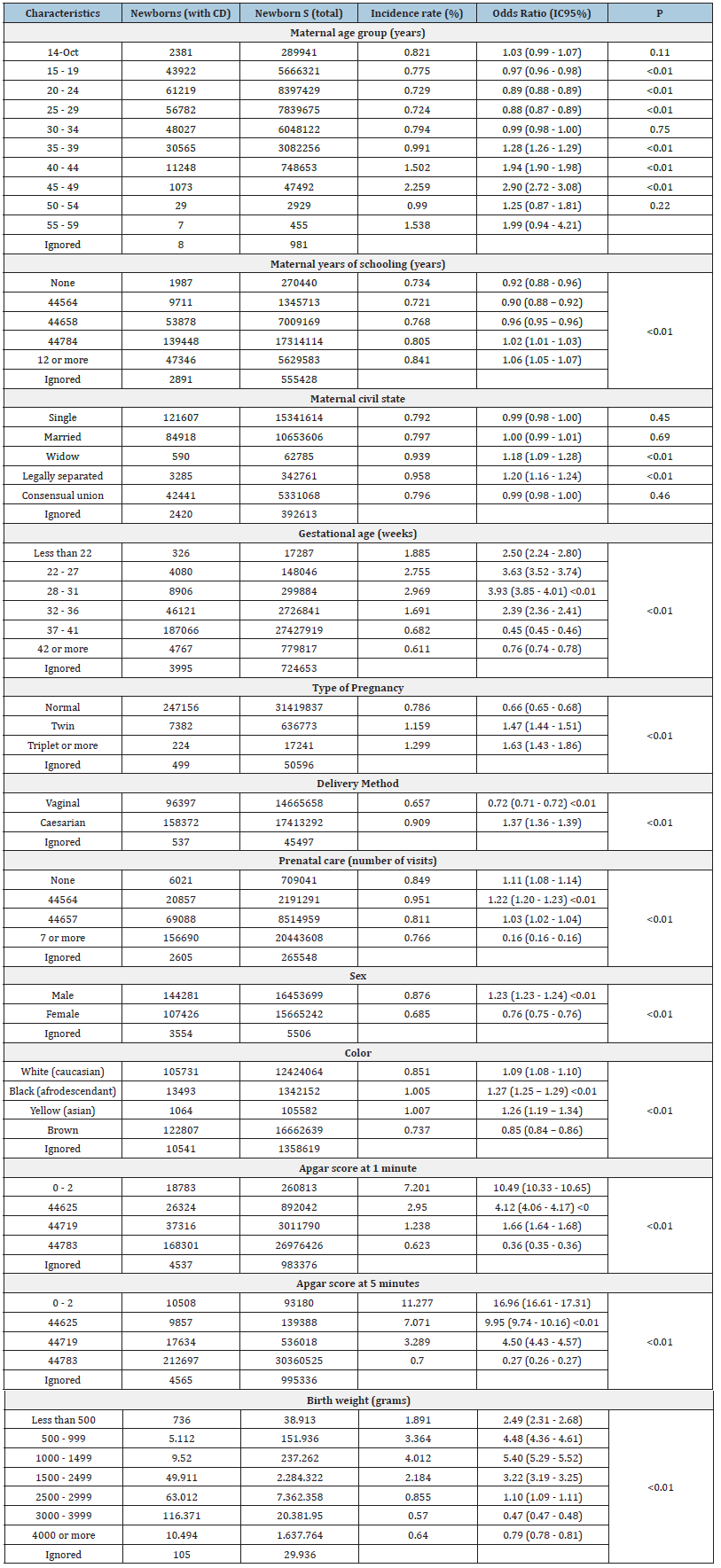
In the study, within the period of 2008-2018, were identified 32,124,447 live births in Brazil; of this total, 225,561 (0.70%) newborns had CD (Table 1). The detection of these anomalies was significantly more frequent among mothers from 45 to 49 years old; among mothers with 12 years of schooling or more; between legally separated mothers; mothers who had 1 to 3 prenatal visits; premature pregnancies of 28 to 31 weeks; in triplet pregnancies or more; in those who underwent cesarean delivery; yellow color; male sex; newborns with 5’ Apgar score 0 to 2 and with birth weight from 1000 to 1499 grams (P <0.01) (Table 1). For 924,235 (2.88%) newborns, the field related to CD was not filled, and these cases were included in the ignored category. The Southeast Region had the highest incidence rate of CD (0.93%), and the North Region the lowest (0.55%) (P <0.01) (Figure 1). Among the Brazilian states, São Paulo had the highest CD incidence (1.12%), and Maranhão the lowest (0.40%) (P <0.01). The average incidence between regions was 0.74% (± 0.13) and between states it was 0.70% (±0.17). Regarding the annual incidence of CD in Brazil during the studied period, an average of 23,387 (±608.93) cases per year was identified, with a progressive increase in the number of affected newborns (R²= 0.94, p<0.01). A peak in the detection of central nervous system anomalies was identified between 2015 (8,1/1,000 live births) and 2016 (9,1/1,000 live births). The most common CD were those of the musculoskeletal system, congenital deformities of the feet, CD of the nervous system and circulatory system. An increased incidence of chromosomal abnormalities was observed in neonates born from mothers aged over 35 years.
Figure 1:Incidence rate of CD in Brazil between 2008 and 2018.
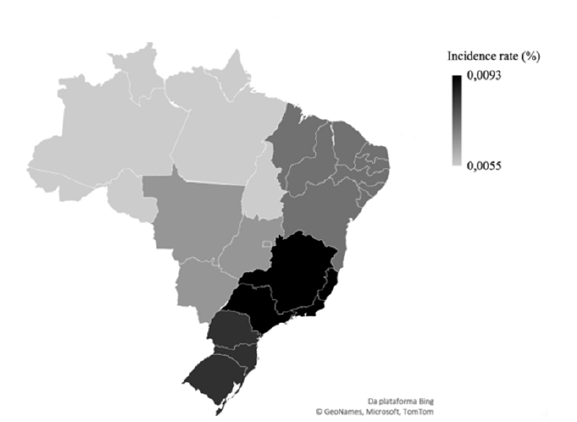
Table 1:Sample characterization.
The present study demonstrated a progressive increase in the number of newborns with CD in the studied period, from 19,878 in 2008 to 25,932 in 2018. It also shows significant regional differences, with the North region presenting the lowest rate of incidence. The discrepancy in the notification can be explained by the possible inequality of access and distribution of specialized assistance services for CD around the country [21]. The urban centers of the South and Southeast regions concentrated the highest incidence of CD, in accordance with the distribution of general and specialized healthcare services [21]. The Latin American Collaborative Study of Congenital Malformations (ECLAMC) has observed differences in the records of CD between countries in Latin America, with the prevalence in 2011 varying from 1.4% in Ecuador to 4.2% in Brazil [22]. These assessments were carried out by trained people who were actively searching for CD, since this is the main objective of ECLAMC-which could explain the discrepancies in the results of their study and the present one. The global prevalence, in the same study, was 2.7% in line with the average for countries in Latin America [22]. Studies based on SINASC in different regions of Brazil have also shown varying frequencies, with 0.20% in Acre [23]; 0.58% in Rio Grande do Norte [24]; 0.92% in Rio Grande do Sul [25]; and 1.6% in São Paulo [26] corroborating the data obtained by the present study.
Even with some regions showing higher incidences and with the progressive increase in the number of neonates with CD nationally, low rates identified strongly suggest the possibility of under-registration and point to the need for interventions to qualify the diagnosis of CD [13]. Although restricted to large centers, education and training in medical genetics have been implemented in health services in Brazil [27]. Primary healthcare professionals must receive adequate training to administer care to patients with CD, knowing how to orientate the prevention, recognition and coordination of care at birth or in another period of life [28]. There was a peak detection of anomalies of the nervous system between 2015 and 2016, probably associated with the Zika virus infection epidemic [29,30] and the consequent increase in the surveillance of such anomalies, especially microcephaly. The syndrome triggered by prenatal infection by the Zika virus started to have immediate compulsory federal notification as of February 201630 and gained national visibility, expanding the surveillance of professionals and the healthcare system in relation to such cases [31] The present study identified a higher relative frequency of CD in newborns with birth weight from 1,000 to 1,499 grams and premature pregnancies of 28 to 31 weeks in this period in Brazil. According to Costa [32], a newborn with congenital malformation is twice as likely to have low birth weight, possibly being a consequence of CD or the syndromic condition in these individuals [4]. It is not possible, however, to know whether CD were the causative factor of the shortest duration of pregnancy, as they are not necessarily a factor in early gestational termination [33,34]. The present study demonstrated a higher incidence of CD in newborns with 5’ Apgar scores 0 to 2, which suggests poor intrauterine conditions, impacting on vitality at birth [35]. A similar result was observed in a study in the city of Rio de Janeiro, which identified a higher prevalence of CD among newborns with a 5’ Apgar score <7 and low birth weight [36]. A higher incidence of CD at birth was identified in males, as observed in other studies [35,37]. Regarding the newborn’s color, there was a higher incidence of CD in yellow color, unlike other studies, in which the highest frequencies were found among brown individuals [35,37]. It is noteworthy that different CD vary significantly between ethnicities, and some dysmorphisms can be considered variations from normality [35]. A study published in 2015 demonstrated similar results, observing a higher frequency of CD in children of mothers with advanced age (>35 years old) [38]. Regarding maternal education, another study demonstrated that the group with less years of study had a higher risk of CD [39], which was dissonant from our research. Maternal education can be related to socioeconomic factors, access to health information, access to health services and the mother’s age. The present study may support new prospective studies on each factor to understand how each one interferes with the risk of CD.
Pregnancies with less than recommended prenatal visits had a higher risk of having CD at birth, while those who had 7 or more visits had an incidence around 10% lower, representing a protective factor (<0.0001). The Brazilian Ministry of Health recommends at least 6 prenatal follow-up visits: one in the first trimester, two in the second and three in the third trimester of pregnancy [12,40,41]. Ideally, reproductive counselling should start even before pregnancy. It is up to health professionals to orientate how couples’s lifestyle in gestational planning and pregnant women should be, to influence good embryo-fetal development [12,41]. There is also a need to perform a thorough prenatal care, in an attempt to modify possible problems in maternal and fetal health in a timely manner, avoiding unfavorable outcomes [42]. The insertion of clinical genetics in primary care would be a potentially effective action for the implementation of an effective service network and, for this, the multidisciplinary team must receive adequate, longitudinal and updated training. Support services for primary care professionals with extensive access, such as Alô genetica, TelegeneticaMG, OCD [OsteoCondroDisplasias] and SIAT [National System of Information on Teratogenic Agents] are also important sources of information and diagnostic support available at national level [42]. However, these services are still accessed by a small number of professionals. To expand support for primary care professionals in relation to CD, the growing insertion of medical genetics services within the scope of SUS and teleconsulting initiatives in genetics could possibly be a good support.
SINASC is a population surveillance tool for CD since this field was incorporated into DNV in 1990 [17-20]. Surveillance services (such as these six international collaboration networks: ECLAMC, ICBDSR, EUROCAT, BINOCAR, SEAR-NBBD and ReLAMC) [43] are essential in monitoring and improving care and can provide professionals and the health system with tools to prevent CD on the global epidemiological scenario [42,44]. Despite the fact that SINASC information is in the unrestricted public domain, available to the entire population in free access, there was a scarcity of studies evaluating CD in Brazil, limited to local and regional initiatives [2,13,25,37,45]. Therefore, this study is the first to address the epidemiological profile and to outline factors involved in CD cases nationally. The importance of further studies with the available data is highlighted, as these data are fundamental for the collective construction of knowledge and the management of the health system [39]. The reference services in Rare Diseases (RD), disorders which prevalence is less than 65per 100,000 individuals according to the World Health Organization [12], were established by the National Policy for Comprehensive Care for People with RD, which offers preventive, diagnostic and therapeutic actions [44], aiming to reduce morbidity and mortality and improve the quality of life of individuals with RD. There are more than 6 thousand RD that affect more than 8% of the population, which constitutes a relevant public health problem [30,46], with approximately 77.5% of CD being RD [47].
The methodological limitations of this study include the fact that it was conducted retrospectively [48]. The assessment of the presence of CD was performed exclusively at birth, with no longitudinal follow-up of cases or subsequent re-screening of individuals without anomalies identified at birth [48]. Furthermore, even though public and private hospitals register a progressive increase in the number of individuals with CD, the data still suggest underreporting [13]. The unequal training of healthcare teams prevents qualified screening and makes it difficult to monitor the population with CD, which represents a limiting factor for the analysis [49]. It is crucial to recognize the need for prospective longitudinal studies in this field in order to qualify the strategies for surveillance, diagnosis and treatment of these newborns, aiming at the most appropriate way to quantify and describe the CD, as well as pursuing the prevention and identification of the risk factors involved.
Conclusion
This is the first study to assess the epidemiological profile of neonates with CD detected at birth throughout Brazil. The reduced incidence of registered CD suggests possible underdiagnosis and underreporting, highlighting the need for interventions for the adequate and early recognition of anomalies. Factors such as age group, education level and prenatal care were associated with more elevated incidence of CD. These results are relevant for public health in the country, as they may be susceptible to change in the upcoming years, through awareness campaigns on family planning and contraception, investments and improvements in education and training of healthcare professionals. It is also urgent that prospective studies on each factor be carried out, to better comprehend how they individually interfere in the risk of CD.
References
- International Clearinghouse for Birth Defects Monitoring Systems. International Centre for Birth Defects, WHO Human Genetics Programme & European Registration of Congenital Anomalies (2003). World atlas for birth defects/International Centre for Birth Defects of the International Clearinghouse for Birth Defects Monitoring Systems, 2nd ed. World Health Organization.
- Costa CMS (2005) Profile of Congenital Malformations in a sample of births in the city of Rio de Janeiro 1999-2001. National School of Public Health, Oswaldo Cruz Foundation, Rio de Janeiro, Brazil.
- Schafer GB, Thompson Jr NR (2015) Genética Médica - An integrated approach. 1st (edn), Editora AMGH LTDA. Porto Alegre, Brazil.
- Ramos AP, Oliveira MND, Cardoso JP (2008) Prevalence of congenital malformations in newborns in a public hospital. Saúdcom 4(1): 27-42.
- Mendes IC, Jesuino RSA, Pinheiro DS, Rebelo ACS (2018) Congenital anomalies and their main preventable causes: A Review. Rev Med Minas Gerais 28: e-1977.
- Guerra FAR, Llerena Júnior JC, Gama SGN, Cunha CB, Theme Filha MM (2008) Birth defects in the municipality of rio de janeiro, Brazil: An assessment through SINASC (2000-2004). Cad Public Health 24(1): 140-149.
- Oliveira CIF, Fett-Conte AC (2013) Birth defects: Risk factors and consequences. J Pediatr Genetic 2(2): 85-90.
- Rizk F, Salameh P, Hamadé A (2014) Congenital Anomalies: prevalence and Risk Factors. Univers J Public Health 2(2): 58-63.
- Mills JL (2010) Malformations in infants of diabetic mothers. Birth Defects A Clin Mol Teratol 88(10): 769-778.
- Lobo I, Zhaurova K (2008) Birth defects: Causes and statistics. Nature Education 1(1): 18.
- Nhoncanse GC, Germano CMR, Avó LRS, Melo DG (2014) Maternal and perinatal aspects of birth defects: A case-control study. Rev paul pediatr 32(1): 24-31.
- Horovitz DDG, Llerena Júnior CL, Mattos RA (2005) Attention to birth defects in Brazil: Current scenario. Cad Public Health 21(4): 1055-1064.
- Christianson A, Howson CP, Modell B (2006) March of Dimes: Global Report on Birth Defects - The hidden tool of dying and disabled children, New York, USA.
- Ministry of Health (2016) National Health Council. Deals with guidelines and regulatory standards for research in human and social sciences. Official Gazette, Brasília, Brazil.
- Silva NP (2009) The use of the TABWIN and TABNET programs as tools to support the dissemination of health information Rio de Janeiro: Sergio Arouca National School of Public Health, Oswaldo Cruz Foundation, Brazil.
- Lima AC, Januário MC, Lima PT, Moura W (2015) DATASUS: The use of Information Systems in Public Health. Refas-Magazine Fatec Zona Sul 1(3): 1-16.
- Ministry of Health/DATASUS - SUS Information Technology Department (2020) Information System on Live Births SINASC, Brasil.
- The Brazilian experience in health information systems (2009) Ministry of Health, Pan American Health Organization, Oswaldo Cruz Foundation. Publisher of the Ministry of Health, Ministry of Health, Brasília, Brazil.
- Jorge MHPM, Laurenti R, Gotlieb SLD (2007) Analysis of the quality of Brazilian vital statistics: The experience of implementing SIM and SINASC. Science Collective Health 12(3): 1-12.
- Scheffer M (2018) Demografia Médica no Brasil. São Paulo, FMUSP, CFM, Cremesp, Brazil, p. 286.
- Nazer JH, Cifuentes LO (2011) Congenital malformations in Chile and Latin America: An epidemiological view of the ECLAMC for the period 1995-2008. Rev med Chile 139(1): 72-78.
- Rocha CF (2015) Birth defects: prevalence in the state of Acre - 2001 to 2010. Paulista School of Nursing, Federal University of São Paulo (UNIFESP), São Paulo, Brazil.
- Lucena EES, Lima NA, Silva CF, Santos MM, Fernandes TAAM (2018) Epidemiological Profile of Congenital Malformations in Newborns in the State of Rio Grande do Norte from 2004 to 2011. R Bras Ci Saúde 22(1): 45-50.
- Luz GS, Karam SM, Dumith SC (2019) Congenital anomalies in the state of Rio Grande do Sul: Time series analysis. Rev Bras Epidemiol 22: e190040.
- Luquetti DV, Koifman RJ (2011) Surveillance of birth defects: Brazil and the US. Ciênc Saúde Coletiva 16(1): 777-785.
- Porciuncula CGG (2004) Evaluation of the teaching of medical genetics in medical courses in Brazil. State University of Campinas, Faculty of Medical Sciences, Campinas, São Paulo, Brazil.
- Meira JGC, Acosta AX (2009) Public health policies applied to medical genetics in Brazil. Rev Ciên Méd Biol 8(2): 189-197.
- Nunes ML, Carlini CR, Marinowic D, Neto FK, Fiori HH, et al. (2016) Microcephaly and Zika virus: A clinical and epidemiological analysis of the current outbreak in Brazil. J Pediatr 92(3): 230-240.
- Ministry of Health (2014) Deals with the National Policy for Comprehensive Care for People with Rare Diseases. Official Gazette, Brasília, Brasil.
- Victora CG, Schuler-Faccini L, Matijasevich A, Ribeiro E, Pessoa A, et al. (2016) Microcephaly in Brazil: How to interpret reported numbers? Lancet 387(10019): 621-624.
- Pinto CO, Nascimento LFC (2007) Prevalence study of birth defects in Vale do Paraíba Paulista. Rev paul Pediatr 25(3): 233-239.
- Costa CE, Gotlieb SLD (1998) Epidemiological study of birth weight based on the Live birth declaration. Rev Saúde Pública 32(4): 328-334.
- Costa CMS, Gama SGN, Leal MC (2006) Congenital malformations in Rio de Janeiro, Brazil: prevalence and associated factors. Cad Saúde Pública 22(11): 2423-2431.
- Rodrigues LS, Lima RHS, Costa LC, Batista RFL (2014) Characteristics of children born with congenital malformations in the city of São Luís Maranhão 2002-2011. Epidemiol Serv Saúde 23(2): 295-304.
- Ferreira CR (2019) The burden of rare diseases. Am J Med Genet A 179(6): 885-892.
- Mendes CQS, Avena MJ, Mandetta MA, Balieiro MMFG (2015) Prevalence of live births with congenital anomalies in the city of São Paulo. Rev Soc Bras Enferm Ped 15(1): 7-12.
- Horovitz DDG, Cardoso MHCA, Llerena Junior JC, Mattos RA (2006) Attention to birth defects in Brazil: Characteristics of care and proposals for the formulation of public policies in clinical genetics. Cad Saúde Pública 22(12): 2599-2609.
- Cosme HW, Lima LS, Barbosa LG (2017) Prevalence of congenital anomalies and associated factors in newborns in the municipality of São Paulo in the Period from 2010 to 2014. Rev Paul Pediat 35(1): 33-38.
- Health Surveillance Department. Department of Communicable Disease Surveillance. Protocol for Surveillance and Response to the Occurrence of Microcephaly and/or Changes in the Central Nervous System (CNS)/Ministry of Health, Health Surveillance Department, Department of Communicable Disease Surveillance. Ministry of Health,2015. Ministry of Health, Brasilia, Brasil.
- Vieira TA, Trapp FB, Souza CFM(2019) Information and diagnosis networks-tools to improve diagnosis and treatment for patients with rare genetic diseases. Genet Mol Biol 42(1): 155-164.
- Costa FAS, Quadrado AVM, Brandão AP (2013) Congenital rubella syndrome: Literature review. Rev Med Saude 1(2): 46-57.
- Giugliani L, Vanzella C, Zambrano MB (2019) Clinical research challenges in rare genetic diseases in Brazil. Genet Mol Biol 42(1): 305-311.
- Gomes MRR, Costa JSD (2012) Infant mortality and congenital malformations in the Municipality of Pelotas, State of Rio Grande do Sul, An ecological study in the period 1996-2008. Epidemiol Serv Saúde, Brazil 21(1): 119-128.
- Health Care Department (2014) Department of Specialized and Thematic Care. General Coordination of Medium and High Complexity. Guidelines for Comprehensive Care for People with Rare Diseases in the Unified Health System - SUS / Ministry of Health. Department of Specialized and Thematic Care. General Coordination of Medium and High Complexity. Ministry of Health, Ministry of Health, Brasilia, Brasil.
- National Health Council (2000) It deals with the regulation of prenatal care, institution of the Humanization Program in prenatal care and birth. Official Gazette, DF, Ministry of Health, Brasília, Brasil.
- Hochman B (2005) Desenhos De Pesquisa. Acta Cir Bras 20(2): 2-9.
- Health Surveillance Department (2017) Health Care Department. Integrated guidelines for surveillance and health care within the scope of the Public Health Emergency of National Importance. Ministry of Health. Ministry of Health, Brasilia, Brasil.
© 2022 Victória Machado Scheibe & Amanda Maria Schmidt. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






