- Submissions

Full Text
COJ Nursing & Healthcare
Tolerance and Coping to High Concentration Capsaicin Patch in the Treatment of Peripheral Neuropathic Pain Using Virtual Reality: A Proof-of-Concept Project
Godoy D, Dürsteler C*, Rioja M and Ferrer A
Anaesthesiology Department, Hospital Clínic de Barcelona, Spain
*Corresponding author: Dürsteler Christian, Pain Medicine Section, Anaesthesiology Department, Hospital Clínic de Barcelona, Spain
Submission: March 24, 2022Published: April 19, 2022

ISSN: 2577-2007Volume7 Issue5
Abstract
Keywords: Postherpetic, Postsurgical, Crystal Serenity, Demographic, Demographic, Scenography
Abbreviations:VR: Virtual Reality; NPRS: Numerical Pain Rating Scale
Introduction
Chronic pain is a highly prevalent major health concern; 17% of the Spanish population is affected [1], as indicated by the annual surveys in health epidemiology. Chronic pain is the third health issue reported by citizens older than 15 [2]. Neuropathic pain prevalence differs among countries (Austria 3.3%, France 6.9%, UK 8.2%, USA 9.8-12% or Ireland 17%) [3]. In Spain is estimated that 5-8% [4-6] of the populations suffers neuropathic pain (20-25%) of chronic pain patients [4]. The global burden of disease caused by chronic pain is significant with a severe impairment of patients’ quality of life, physical and function and mental health (anxiety, depression) [6-8].
Figure 1:
Its repercussion on professional, social and family spheres, as well as sleep disturbance or interference can affect considerably to mood status [5]. Neuropathic pain is caused by injury on somatosensory system by different noxious stimuli (infectious; postherpetic neuralgia, metabolic; diabetic neuropathy, trauma; surgical injury) [7,8] and is classified in central and peripheral neuropathic pain. Clinical presentation of neuropathic pain includes positive (burning pain, paraesthesia, dysesthesia, allodynia, hyperalgesia) and negative (hypoesthesia, paresis) symptoms [5]. Pharmacological management of neuropathic pain proposed involves the combination of antidepressants and anticonvulsants (first line treatment), weak opioids and capsaicin (second line treatment) and strong opioids (third line treatment) [9]. Capsaicin is a chilly pepper derived agonist of the TRVP1 receptor of nociceptive sensory neurons. This receptor senses heat stimuli, low pH and capsaicin, inducing pain by depolarization of nociceptive neurons (burning, itching pain) [6,8,10]. The vigorous ligation of capsaicin to TRPV1 receptor causes a persistent opening of this cationic receptor (Figure 1), causing apoptosis and death of sensory neurons by massive entrance of cations inside the membrane. This overstimulation of receptors causes (paradoxically) a defunctionalisation with a final neurophysiologic correlate consisting in a lower spontaneous nerve activity and a loss of sensory stimulation [3].
Figure 2:

Topical administration of highly concentrated capsaicin (8%) is an accepted and useful treatment of neuropathic pain, but it causes pain, burning sensation, topical reaction and discomfort in near all patients. Burning, itching pain and erythema is common cause of intolerance and interruption of these valuable treatment. Thus, prophylactic analgesic treatment is usually used (topical, oral, intravenous treatment) to ensure feasibility of therapy. Virtual Reality (VR) propose an environment scenography using 360º video imaginary. This environment leads to an immersive experience thanks to a hardware (VR glasses; Pico G2 4K, VR Pharma, Spain) (Figure 2). The first reports (Hoffman et al.) [11] demonstrated that VR confers analgesic properties based in cognitive distraction in patients with severe skin burns [11,12]. It demonstrated to be useful to reduce pain levels in odontology procedures that usually need analgesic treatment [11,13]. Distraction based analgesia is a non-pharmacological technique [12] that alters acute pain perception, reducing activity on specific pain processing related brain areas, especially in young people [11]. A growing body of evidence suggest a potential use in chronic pain conditions [13]. Recent experimentally works demonstrated that VR has been useful neutralizing pain perception after electrical, thermal and pressure stimuli [11]. Specifically, Hughes et al. [13], concluded that VR decreases pain perception induced by continuous capsaicin treatment and secondary hyperalgesia. VR proposes a holistic care approach of pain patients [14], potentially improving comfort and decreasing pain sensation during topical administration of highly concentrated capsaicin patch. This approach could add analgesic sparing effect (Figure 3).
Figure 3:

Objective
i. To evaluate the degree of comfort and tolerability of
capsaicin patch treatment with simultaneous use of VR, in patients
affected of peripheral neuropathic pain.
ii. To quantify the pain level along the treatment duration,
using a Numerical Pain Rating Scale (NPRS) during the procedure.
iii. To estimate the need of rescue analgesia demanded by
patients during patch application.
Material and Methods
Figure 4:

Our study was approved by the Institution Ethical Board (CEIm Hospital cLínic de Barcelona# HCB/2021/008). Prospective experimental descriptive study. Non probabilistic accidental or consecutive sampling for all patients admitted to Hospital Clínic Pain Unit to treat with 8% topical capsaicin patch from November 2021 to June 2022, willing to voluntarily participate in the study and fulfilled inclusion criteria. Outcome were collected through an electronic survey (Lime Survey) protected by double encryption, only accessible to investigators. Statistical analysis was performed using Microsoft Excel 365 and SPPS 19.0. Descriptive statistics was used to analyse quantitative variables. Data are expressed as number of cases, minimum, maximum, mean and standard deviation, regarding pain level (Figure 4).
Study Design
A screening visit to explain procedure, obtention of informed consent and patient codification was performed. Demographic variables as well as principal outcome measurements were recorded. Variables were a comfort Likert Scale, PainDETECT neuropathic pain questionnaire, Visual analogic scale and numerical pain rating scale. A brief instruction about VR interaction was then provided. These variables were obtained before the beginning of treatment, 40min later and 10min after the end of treatment. During the treatment, VR was used with 2 different videos (Ocean Breeze and Crystal Serenity). Ocean Breeze video invites patients to breath in a relaxed manner in a natural seaside environment. Crystal Serenity (13min) immerses patients in s snowy sightseeing inducing cold sensation on patients in order to compensate burning pian induced by capsaicin. Ocean breeze was used first (with a previous basal variables register). Variables were recorded again on minute 40, that is described as the moment of maximal discomfort in previous studies, when Crystal Serenity (16min) video began. 10 minutes after the end of treatment variables were recorded again (Figure 5).
Figure 5:
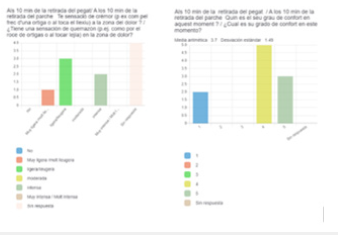
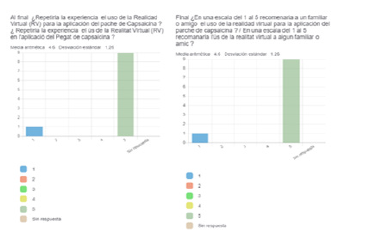
Preliminary Result
We recruited 10 patients, two of them excluded by severe hypoacusis. 50% of patients were female, with a mean age of 55±17. 60% of patients suffered postsurgical neuropathic pain, while a 20% suffered a postherpetic neuralgia and 20% other origins. Body parts involved in treatment were inferior extremities (60%) and thoracic region (40%). 90% of patients were treated with topical analgesia (EMLA cream) previously to patch application. All patients ended VR programs, but one, due to technical problems. Mean basal NPRS was 5±3.06 with a minimum of 1 and a maximum of 9. Comfort Likert Scale mean was 4±0.82. 40 minutes after the beginning we observed a NRPS of 6±3.14 with a minimum of 0 and a maximum of 9. Regarding comfort scores, the mean value observed at 40 min was 3±1.42 and burning sensation was described as intense or highly intense by 100% of patients. 10 minutes after removal of capsaicin patch, mean NRPS was 4±3.25 (Figure 6), Likert Comfort scale 4±1.5. burning sensation was experimented as intense by 40% of patients and low o more intense by the other 60%. Patients were asked at the end of the procedure about the willingness to repeat the treatment accompanied by VR again, 90% of them ranked positively. Most of them would recommend VR technique to other patients or relatives with a value of 5/5 in a Likert scale.
Figure 6:
References
- Cabrera-LA, Cantero-Braojos MÁ, Garcia-FL, Hoyos JAG (2018) Living with disabling chronic pain: Results from a face-to-face cross-sectional population-based study. BMJ Open 8(11).
- Functional dependency (people aged 65 and over).
- O’Brien J, Keaveny J, Pollard V, Nugent LE (2017) Advancing nursing practice: Management of neuropathic pain with capsaicin 8% without physician supervision. Clinical Nurse Specialist 31(3): 157-62.
- Bouhassira D (2019) Neuropathic pain: Definition, assessment and epidemiology. Revue Neurologique 175(1-2): 16–25.
- Definitive Neuropathic Pain Guide.
- Mason L, Moore RA, Derry S, Edwards JE, McQuay HJ (2004) Systematic review of topical capsaicin for the treatment of chronic pain. British Medical Journal 328(7446): 991.
- Blair HA (2018) Capsaicin 8% dermal patch: A review in peripheral neuropathic pain. Drugs 78(14): 1489-1500.
- Hoy SM (2020) Capsaicin 8% dermal patch in peripheral neuropathic pain: A profile of its use. Drugs and Therapy Perspectives Adis 36: 47–56.
- Finnerup NB, Attal N, Haroutounian S, McNicol E, Baron R, et al. (2015) Pharmacotherapy for neuropathic pain in adults: Systematic review and meta-analysis. Lancet Neurol 14(2): 162-173.
- Attal N (2019) Pharmacological treatments of neuropathic pain: The latest recommendations. Revue Neurologique Elsevier Masson SAS 175(1-2): 46-50.
- Huang Q, Lin J, Han R, Peng C, Huang A, et al. (2022) Using virtual reality exposure therapy in pain management: A systematic review and meta-analysis of randomized controlled trials. Value in Health 25(2): 288-301.
- Spiegel B, Fuller G, Lopez M, Dupuy T, Noah B, et al. (2019) Virtual reality for management of pain in hospitalized patients: A randomized comparative effectiveness trial. PLoS ONE 14(8).
- Hughes SW, Zhao H, Auvinet EJ, Strutton PH (2019) Attenuation of capsaicin-induced ongoing pain and secondary hyperalgesia during exposure to an immersive virtual reality environment. Pain Reports 4(6).
- Ahmadpour N, Randall H, Choksi H, Gao A, Vaughan C, et al. (2019) Virtual Reality interventions for acute and chronic pain management. International Journal of Biochemistry and Cell Biology 114.
© 2022 Dürsteler C. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






