- Submissions

Full Text
COJ Nursing & Healthcare
Nursing and the Tele-Medicine Revolution: The Unit Charge Nurse as the “Prime Consultant”
Robert J Adams*
Distinguished Professor of Neurology, Medical University of South Carolina, USA
*Corresponding author: Robert J Adams, Distinguished Professor of Neurology, Medical University of South Carolina, President, Zeriscope Inc, Charleston, South Carolina, USA
Submission: November 11, 2021Published: November 22, 2021

ISSN: 2577-2007Volume7 Issue5
Introduction
I am an engineer, a Vascular Neurologists and inventor. I am not a Nurse, but I have great appreciation for what nurses do and how fundamentally important are their contributions to patient’ well-being at many levels. By way of disclosure I am also President of a for-profit South Carolina company, Zeriscope, Inc (Zeriscope.com) that makes portable and wearable telemedical systems.
Even before the Covid 19 pandemic, telemedicine was driving a revolution in how health care can be delivered. Since 1996, there has been an FDA approved treatment for stroke (tissue plasminogen activator) but its use was restricted to 3 hours after stroke onset. There were (are) few vascular neurologists and not enough time to get them together physically with patients suffering acute stroke. This treatment was underutilized. Telemedicine solves the problem by addressing the twin enemies of time and distance, barriers which are faced every day in every hospital or skilled nursing unit not just for stroke but all medical illness. Its use in stroke became representative of the kind of critical improvements that can be realized. This model is very successful and should be mapped to the experience on medical-surgical units everywhere for all acute illness with one critical and important difference: the potential role of nurses.
Since 2001, I have treated well over 1000 stroke patients using telemedicine. “Tele-stroke” is now fully established as an essential weapon in our arsenal enabling countless patients to receive skilled, urgent consultations to help decide if they should receive thrombolytic therapy, and/or be referred for thrombectomy. In a typical telemedicine consult, there is a patient, an on-site tele-presenter, and a remote consultant. Tele stroke is typical of many scenarios where the tele presenter is a nurse. This model has been very successful but it important to emphasize that the role of nurses in telemedicine should not be restricted to that of tele-presentation.
In my experience the critical factor in an urgent care consult is the “laying on of experienced eyes”. The human brain is quite good at pattern recognition. When confronted with a sick patient, an experienced consultant can see and hear things that facilitate diagnoses, preparation of treatments and rapid triage. The patients’ appearance, voice, speech, movements, breathing and many other features are instantly factored, weighted and assessed.
Doctors currently do most tele-stroke consults, for example, but doctors are not the only medical providers with “experienced eyes”. Nurse Practioners, are increasing their participation as consultants in many medical domains including stroke. But I believe that there are many more ways in which telemedicine can enhance the work that registered nurses do in the typical medical surgical skilled nursing units that need to be visualized. Especially on nights and weekends there are only a few “charge or supervising nurses” and they may be spread quite thin. It is very important that their time, expertise and experienced eyes be effectively leveraged. They are the first line of defense, the “prime consultants” so to speak, to whom the floor CNA’s and LPN’s look for guidance. Telemedicine would not be needed if we had an excess of nurses that could physically pop into any room at a moment’s notice. But this is not realistic. In fact, there is a shortage of nurses.
I am suggesting that the hospital can be seen as comprised of a Core Unit consisting of the patient and bedside nurse surrounded by any number of potential consultants, being defined as anyone with knowledge and skill important to that patient’s wellbeing who is not physically present. The first link in this chain of consultancy is the charge or supervising nurse and indeed most problems are resolved at this level. For this to work the prime consultant needs the best information about the patient’s situation or problem. Apart from being physically present or obtaining information by text or telephone, which is the current practice, assessing the issue through the eyes and ears of the bedside nurse is the next best thing. Before looking beyond the unit for help the first step is to bring in these experienced nursing eyes. Telemedicine can make this step faster and much more easily scaled compared to moving around the unit(s) which amounts to wasted “travel time”.
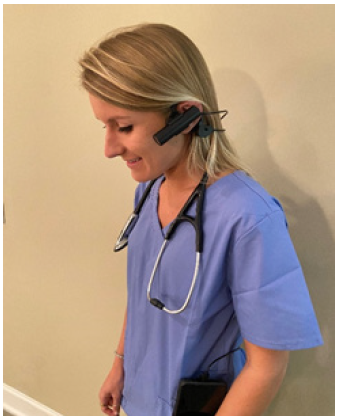
The input of the supervising nurse can answer crucial questions from the bedside staff and family as to the status of sick patients, whether there have been important changes since arriving on the unit or since surgery and so on, and, importantly, whether care escalation is needed. These answers may not be expressed in ICD-10 codes but they can mean the difference between life and death, seamless care and a botched hand-off, between actions that bring specific treatments to bear and lost opportunities for intervention. Over the last decade, my company and others, have developed headset-based cameras that can be worn around the neck (Figure 1), like a stethoscope, donned when needed (Figure 2) and activated with a few commands to a tethered cell phone. A nursing assistant can, using such a system, access their prime consultant and tele-present a distressed patient in minutes without bringing a cart into the room and doing extensive registration. This is much more than “medical face time” as these are HIPPAA compliant systems that allow hands free, stethoscope enabled tele presentation. The systems are web based enabling any number of consultants to participate, serially or in concert. Texts and phone calls from bedside staff are still important but they are in no way comparable to “seeing” the patient. We should take advantage of technology that allows supervising nurses to quickly look over the shoulder of bedside team members.
Figure 1: Zeriscope headset prior to activation.
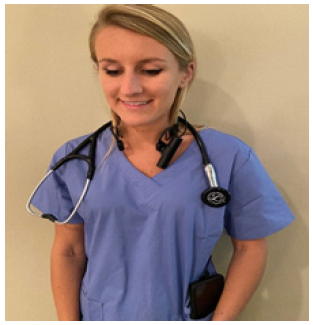
Figure 2:Zeriscope donned and in use.
Apart from evaluating a patient in distress, charge nurses could also take a quick look (tele-rounding) at scores of patients without leaving their computer, and be better prepared to interpret any changes in condition that might arise. Training and education would be enhanced. The web-based systems available today allow rapid escalation from ward- based CNA to charge nurse to resident/hospitalist to specialist or surgeon on a rapid time scale. “Experienced eyes” at all levels anchored by bedside nursing staff wearing the headset could address a number of needs. This expanded view of consultancy would also allow us to bring in social, (absent family members, ministers, therapists) in addition to medical, resources.
We could call this “Tele-Nursing” but its not so much the nursing that is transmitted over the internet but the decision making. Better, faster decisions protect patients and prevent inadequate management that not only threatens patients’ well-being but hospital systems and careers.
I am passionate about this because I have seen what telemedicine has done for stroke care. I have also seen that this revolution has developed in a culture which, without intention, may encourage nurses to be seen as supportive and their role limited to presentation, rather than resolution, of the problem. This is a lost opportunity to take full advantage of the experience of our existing care teams while keeping open the option of bringing in whomever else that may be needed.
I suggest the time has come for nurses to be equipped to function in the hospital with greatest efficiency. Nursing may need to more strongly advocate with their medical and hospital systems to be fitted with modern tools that recognize their role as the prime consultants and that limit the time wasted in physically moving about the hospital. With the bedside members of the nursing team equipped with headset cameras “experienced nursing eyes” can be optimized and made an integral and important part of the revolution in medical care made possible by Telemedicine.
© 2021 Robert J Adams. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






