- Submissions

Full Text
COJ Nursing & Healthcare
Village participants’ perceptions on the use of the Health Guardian for Longevity Program to sustain health in West Africa?
Freida Pemberton*
Molloy College, USA
*Corresponding author: Freida Pemberton, Molloy College, USA
Submission: June 17, 2021Published: July 27, 2021
ISSN: 2577-2007Volume7 Issue3
Abstract
This case study explored the impact of bringing tailored health care to a village in West Africa using the Health Guardian for Longevity Program (HGFLP). Pemberton [1] points out, “the HGFLP takes in hand assessed data, mobilizing the powerful tools of mobile, interactive, remote, video, virtual technologies, selected learning models, behavioral theories, and humor to treat patients as individuals.” The village team leaders led groups of 25-38 individuals (100 participants) through the case study process. A random selection of 100 out of 200 participants in the on-site visit and health promotion program of 2014 was conducted. The population spanned the life cycle from School-Age to Older Adult-Age. The study began in 2014 to explore the impact of the participants’ online usage of the HGFLP related to health care status and sustainability following a healthcare crisis.
The participants used the program for 1.5 years, completed in 2016. The questionnaire was administered to the villagers by the team leaders. The study participants responded to the HGFLP Perception Questionnaire, a 10-item Likert-scale Questionnaire Data using excel to tabulate, analyze and prepare graphs of the perceptions of the villagers by the primary investigator in 2016. The results of the study revealed effective outcomes for 7 out of 10 items. In response to three items, it was identified that modifications were needed;
A. Provide more intensive training for team leaders,
B. Narratives must be written in the language of the villagers, and
C. Health partners need to learn the native language. Strategies for sustainability of quality healthcare using telehealth practice, virtual, and mobile devices were supported.
This case study focused on the utilization of the health guardian for longevity program as a tool designed to sustain the health of the Villagers outside of Benin, West Africa.
Introduction
This paper presents a case study that explored the impact of a custom-tailored mobile telehealth program (Health Guardian for Longevity Program) on the delivery and sustainability of quality care to an indigenous population. The case study was developed by applying algorithmic thinking that facilitated the continuance of addressing, at a distance, the health care needs of the villagers living outside of Cotonou Benin, West Africa. The village has a population of approximately 30,000 residents, with no access or very limited access to health care. There were several small clinics, village infirmary, and a hospital 11 miles from the village. The health care services were fee based. The government provided free malaria treatment for pregnant women, women with children, and children younger than age five. In addition, women scheduled for cesarean sections were also provided free health care. Beyond the free government services, access to health care was not available to the residents of the village without payment. The outreach group worked collectively during the health care program with the village health care team leaders to provide health care services that incorporated the Health Guardian for Longevity Program (HGFLP). This paper presents the purpose, background, problem statement, research question, description of case study participants, literature that supports the original development of the HGFLP created in 2012 as a conceptual framework, step-by-step process/method, analysis, conclusions, and recommendations for future studies
Purpose
The study was conducted to explore the impact of the villagers’
use of the HGFLP that was created to address the health care needs
of those living in indigenous communities with limited or no access
to health care. The tailored program centered on the following
objectives for successful health stability outcomes for the residents
of the villagers outside of Cotonou Benin;
A. Facilitate restoration and sustain healthy behavioral
practices using a tailored health care approach that incorporates
modified mobile technology
B. Enhance the villagers’ and team leaders understanding of
the disease, treatment, recovery and maintenance process
C. Empower villagers to be key players in self-care through
the input and feedback loop of the team leaders following the
onsite visit
D. Empower villagers and team leaders to become effective
managers of their care in an environment of convenience and
comfort, the village outside of Cotonou Benin
E. Enhance coping skills-stress reduction for the villagers
and fishermen
F. Facilitate holistic health behaviors with a touch of humor
applicable to the villagers’ community health concerns
G. Facilitate a sense of never being alone-with access to the
health care team leader
The study explored the villagers’ perceptions of the impact of
the online use of the program to address health care needs and the
effect of the HGFLP on the participants’ outcomes. An identification
of the attainability of the program’s purposes from the perspective
of participants were captured and analyzed to determine potential
benefits of the HGFLP toward sustainability achievement following
a villager’s healthcare crisis. The better the understanding of the
“diagnosis, treatment, and recovery” along with a good support
system; the better one can cope with an illness and adopt behaviors
designed to influence positive outcomes [2].
Background
The report of Global Observatory Statistics [3], 2015 for Benin
noted the average life-span for the population was ages 50-53.
The average life-span for the villagers in West Africa was 50-60.
The average family income was approximately $70-$100 USD per
month for a 10 hour workday. The villagers with jobs worked as
artisans, farmers, fishermen, motorbike taxi drivers, and traders
of all kinds of goods. About 10% (3,000) of the population were
major fishermen and earned $800-$1500 USD during the greatest
fish harvest time of Mid-August. Their diet consisted of powder
milk, cornmeal porridge, spinach and fish during the fish harvest
of every three-four months. The fish cost $10-$15 USD per package.
Foods high in protein were limited as a result of the population’s
low socioeconomic status. In the village, Wi-Fi was not an option.
The delivery and operation of the virtual component of the health
care program was designated to three appointed team leaders who
had transportation, lived within city limits of Cotonou Benin, and
had access to Wi-Fi (Internet Service Provider).
The village is an hour drive from the city of Cotonou Benin and
a three-hour drive from Lagos, Nigeria. During the on-site health
program in 2014 a client traveled overnight on a motor bike to reach
our onsite health care service program prior to closure. When the
client arrived late that evening, he was diaphoretic, short of breath,
and experiencing tachycardia. This is an example of the measures
one goes through to get health care. The residents of the village
expressed the barriers to receiving health care and the need for
more free health care programs that incorporate mobile technology,
virtual access to an Internet Service Provider, remote monitoring,
and continued follow-up and intervention at a distance/Telehealth.
The well-paved road project completion of 2016 will serve as an
asset to easing the commute from country-to-country and make our
scheduled onsite return visit in 2020 program accessible to a larger
population (Figure 1).
Figure 1: Example of the virtual communication with the villagers.

The Problem
We conducted five (2001, 2003, 2005, 2010, and 2014) on-site
health care outreach programs, working in collaboration with the
village’s health care team leaders. During the onsite health care
visits, we provided the following services and programs; holistic
health assessments, health screening, wound care, referrals,
therapeutic treatments for chronic diseases and behavioral health,
health promotion and disease prevention education, life-style
change planning, nutrition planning within the social determinants
of health obstacles. The major enhancement in the health care
service was the incorporation of the Health Guardian for Longevity
Program. It provides the mechanism to the continued follow-up of
our clients at a distance and continued application of progressive
health care interventions. The major contributors to the villagers
shorten life-span included; lack of access to health promotion
and disease prevention programs, lack of access to health care
services, late diagnosis and intervention, poor nutrition, and lack
of continued health monitoring. In terms of support systems, they
were extremely limited. Referrals and follow-up delays posed
serious problems in terms of client outcomes and health stability,
generating the necessity to incorporate telecommunications (The
Health Guardian for Longevity Program) being used effectively in
the USA.
The implementation of the Health Guardian for longevity
Program within the USA resulted in positive outcomes and several
requests to develop and implement a tailored program that
addressed individual and community-based health care needs.
Through the application of algorithmic thinking, the development of
the Health Guardian for Longevity Program was operationalized for
the residents of the village outside of Cotonou Benin, with a minor
modification in the construct and a work-around in the delivery
process. It was important to capture the views of the participants
in terms of the impact of the HGFLP in meeting their needs as using
the prior visits without the technology/virtual program as a base
of comparison.
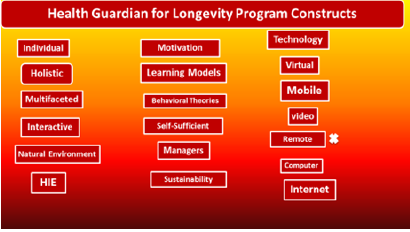
Figure A shows the components of the construct in the
development of the program and the “X” next to the remote
construct component was the bases for the work-around. Remote
monitoring was modified to be done using digital equipment by the
team leader and transmitted to the primary health care provider
for follow-up and intervention to be captured in the villagers’
progressive updated tailored program (Figure 2).
The required technological equipment was provided to the
health team partners assigned as group leaders of the participants
in the study. The program design centered on changing unhealthy to
healthy life-style behaviors while working through obstacles with
the support of the virtual program. Supplies of medications, medical
resources, Glucometers, digital vital sign monitoring devices, and
other technological equipment were provided for the health care
team leaders taking part in the study. The problem over time was the
reoccurring instability of the health status of the residents. During
the outreach onsite health care program visit in 2014 we identified
that 60% of the population continued to have re-occurring health
problems in terms of hypoglycemia, hyperglycemia, Hypotension,
Hypertension, Bradycardia, Tachycardia, complaints of chest pain,
joint pain, post Cerebral Vascular Accident (CVA) and impaired
oxygenation. The problems warranted an urgent need to change
our practice methodologies.
The problem statement: There is a deficiency in sustainability
of the health restoration for residents of the village outside of
Cotonou Benin. To address health care challenges and achieve
sustainable health outcomes for the Villagers, a different approach
to health care practice was required. The Health Guardian for
Longevity Program, used successfully in the USA, was activated
with technological modifications. The program had the potential
to effectively address the ongoing challenges seen in the Village, as
successfully done for clients in the USA.
Gustafson et al. [2] in a random trial study, concluded
supportive individualized computer–based systems can lead to
a better life experience and effective use of health care services
for a population of 184 HIV-positive patients. Jenny & Fai [4] in a
descriptive study of a population of 48 cardiac patients using CAI
vs. 48 using traditional education, found the CAI group gained
significantly more knowledge. They further noted that the CAI
was recommended for preventive health education programs
and patient’s self-management of chronic diseases. The research
question: What is the impact of the participants’ perceived usage
of the Health Guardian for Longevity Program on health care
sustainability?
Figure 2: Interwoven concepts and Technology Constructs for the Villagers’ Program.
Method/Process
Using a step-by-step process, Figure 2 illustrates that 100 out of
200 participants from the 2014 onsite health promotion program
was randomly selected. 68 were females and 32 were males, with
the ages ranging from 6 to 93. In step one the participants were
grouped by age; school age, adolescent, young adult, middle adult,
and older adult. In step two group-sets were established, resulting
in Group Set A: comprised of nine school ages children (6-10), six
adolescent ages (13-18) and ten older adult ages (66-93) , for a
total of 25 participants. Group set B: encompassed young adult ages
(19-40) for a total of 38 participants and Group Set C composed of
the middle adult ages (42-65) for a total of 37 participants. Step
three encompassed the assignment of the three team leaders taken
from the administrators of the village, and each was assigned to
one of the group sets. In step four, a comprehensive training session
was enacted for all participants, four days per week with return
demonstrations. In Step five, the assessment of the participants was
completed and data captured once every two weeks for a normal
assessment result and twice a week for abnormal results (Figure
3). In the final step six, the team leaders of group-sets A, B, and C,
were given, on a flash drive the series of programs tailored to their
group’s needs, to be presented to the appropriate assigned groups
and to obtain feedback (Table 1).
Brug et al. [5] reported on eight studies that identified the
benefit of tired nutrition education as having a greater chance of
being reviewed, retained, and accepted as relevant when compared
to views related to the use of standard materials and standard
methods of health nutrition education. Lewis [6] conducted a
review of literature related to computer-based patient education
studies and found that for short-term knowledge acquisition the
technology consistently revealed positive outcomes. However, for
long-term achievement, further study was required (Figure 4).
Table 1:Perception of Participants: Survey Questions.
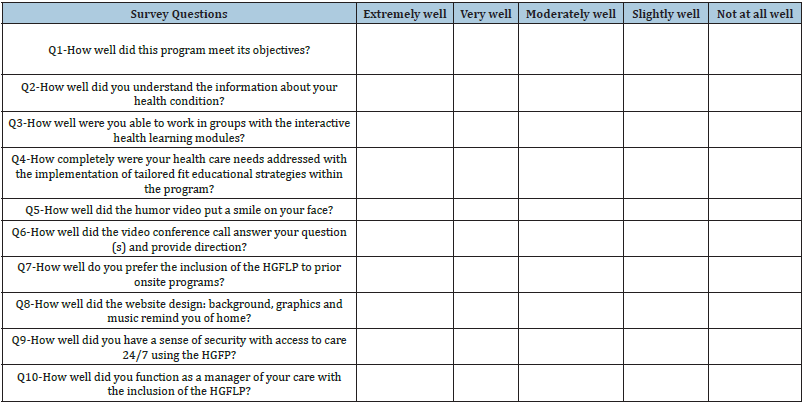
Figure 3: Method/Process.
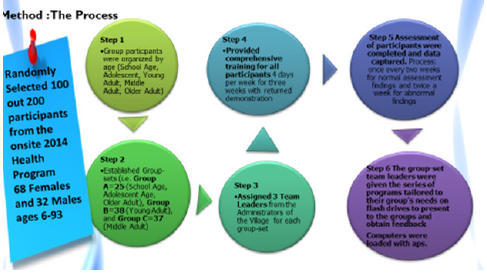
Figure 4

Result and Conclusion
The questions with a combined total rating of less than 80%
for extremely well and very well will be studied after further
modifications are made to the program. The results of the study
revealed effective outcomes for 7 out of 10 items. In response to
three items, it was identified that modifications were needed:
a. Provide more intensive training for team leaders,
b. Narratives must be written in the language of the villagers,
and
c. Health partners need to learn the native language.
Strategies for sustainability of quality healthcare using
telehealth practice, virtual, and mobile devices were supported.
The follow-up visit scheduled 2020 to continue the quantitative
component of the intended mixed study was interrupted as a result
of the pandemic. The researcher recommends the continuation for
future studies to examine whether a correlation exist between the
HGFLP and the clinical assessed data captured over time once the
pandemic is resolved.
References
- Pemberton F (2017) A tailored approach is key: The Health Guardian for Longevity Program uses mobile technology to sustain healthy life behaviors. COJ Nursing and Health Care, Crimson Publisher, NY, USA, pp. 1-5.
- Gustafson, Hawkins, Boberg, Pingree, Serlin, et al. (1999) Impact of a patient-centered, computer-based health information/support system. Am Jof Prev Med 16(1): 1-9.
- Jenny NYY, Fai TS (2001) Evaluating the Effectiveness of an interactive multimedia computer-based patient education program in cardiac rehabilitation. Occupational Therapy Journal of Research 21(4): 260-275.
- The Global Health Observatory Statistics for Benin (2015)
- Brug J, Campbell M, van Assema P (1999) The application and impact of computer-generated personalized nutrition education: A Review of the Literature. Patient Education and Counseling 36(2): 145-156.
- Lewis D (1999) Computer-based approaches to patient education: A Review of the Literature. J Am Med Inform Assoc 6(4): 272-282.
© 2021 Freida Pemberton. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






