- Submissions

Full Text
COJ Nursing & Healthcare
A Juvenile Bilateral Persistent Pupillary Membrane with Deprivation Amblyopia and Based Treatment
Xinlei Hao, Man Yuan, Wei Jin and Anhuai Yang*
Renmin Hospital of Wuhan University, China
*Corresponding author: Anhuai Yang, Renmin Hospital of Wuhan University, China
Submission: February 22, 2021Published: May 27, 2021

ISSN: 2577-2007Volume7 Issue3
Abstract
Persistent Pupillary Membrane (PPM) is a congenital ocular anomaly which originated from neonate. The incomplete involution of it leads to persistent pupillary membrane, which can be unilateral or bilateral and can be variable in size, shape and density. This case is a report of bilateral persistent pupillary membrane with deprivation amblyopia and good visual recovery with no iatrogenic cataract.
Keywords: Bilateral persistent pupillary membrane; Deprivation amblyopia; Medium-size pupils; Surgical treatment
Case Report
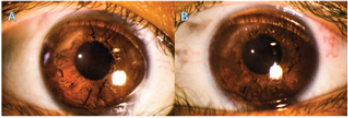
A 11-year-old girl was found pupillary membrane during physical examination. She was born 2 months early and was diagnosed as neonatal jaundice. And her whole sister, who was term delivery, was not found any abnormities in eyes. Other past medical history was normal. Her uncorrected visual acuity, as determined with the use of the Log MAR chart, was 0.20 OD and 0.40 OS. Her Best Corrected Visual Acuity (BCVA) was 0.10 OD and 0.40 OS. The routine slit-lamp examination confirmed the existence of pupillary membrane, which performed radial membrane extending along pupils (Figure 1), having no effect on light reflex. Transparent cornea, clear aqueous fluid, deep anterior chamber and open angle of anterior chamber were also exhibited. The anterior segment optical coherence tomography showed the membrane was not adhered to the corneal endothelium or to the anterior lens surface. Axial length of her eyeballs was 20mm, much below normal. Other examination and parameters were within normal limits. A diagnosis of bilateral persistent pupillary membrane with deprivation amblyopia in the left eye was made definitively.
Considering that the patient was only 11 years old, her retina and macular still had the potential to develop into the normal with the stimulation of light. Excising PPM was a better choice. Besides, her membrane was presented as thick lacy strands extending along iris. Laser therapy probably have no effect on thick membrane or even cause damage to lens accidentally. After informing her parents of advancing of disease and benefit and risk of surgery, a surgery was operated. Ophthalmic knives were used to make a superior clear primary corneal incision and an auxiliary corneal incision at 11 o’clock and 1 o’clock. After which viscoelastic material was injected into anterior chamber using choppers putting apart membrane, exactly speaking, between PPM and lens. Then PPM was excised with capsulotomy vannas scissors, and the tissue was removed by capsulorhexis forceps from anterior chamber, which was sent for histopathological examination. And remained viscoelastic material was excised with flushing needle by irrigation. Finally, the superior clear corneal incisions were proved in closure state carefully with sterile balanced salt solution after surgery. Histopathological examination of the tissue revealed typical features of normal iris tissue which contained massive pigmentation. Postoperatively, the pupils were round and light reflex was normal (Figure 2), and fundus was visible and seen normally using digital wide field. There was no evidence of intraoperative or postoperative surgical complications, such as iatrogenic cataract. At 1 year postoperatively, her uncorrected visual acuity was 0.10 OU, while BCVA improved to 0.00 OU.
Figure 1: Slit-lamp photomicrographs of pupillary membrane before dilation. The membrane in the left eye(B) blocks visual axis more than right eye(A).

Figure 2: Slit-lamp photomicrographs of ocular anterior segment before dilation postoperatively. (A) right eye; (B) left eye.
Discussion
Persistent Pupillary Membrane (PPM) is a congenital ocular
anomaly which originated from neonate. It provides nutrition to
lens in fetal life, the involution of which begins from six month.
The incomplete involution of it leads to PPM, whose prevalence
is about 4-5% [1]. Besides, PPM also can be in combination with
other ocular pathologies, such as congenital cataract, amblyopia,
strabismus, macular hypoplasia, etc. The treatments of PPM include
conservative management [2,3], laser therapy [4] and surgical
therapy [5].
In the case, the size of pupils was the key point, which was
emphasized in the operation. If pupils were too large, PPM would
be stretched and attached to anterior lens capsule, making it more
difficult to inject viscoelastic material behind the iris to separate
PPM from lens and increase the risk of injuring lens. If pupils were
too small, PPM and iris would be accumulated. In the condition, it’s
not easy to differentiate PPM from iris, and ophthalmologists may
hurt iris when using capsulotomy vannas scissors, even causing
bleeding. Above where the reasons why surgery was operated
under medium-sized pupils. Intraoperatively, ophthalmologists
used chopper as an intermediary tool to separate PPM from lens,
to inject as much viscoelastic material as possible behind PPM and
reduce the amount of viscoelastic material leaking into anterior
surface iris or hole of PPM. Above is another surgical skill in this
case. Bilateral PPM and short axial length in this case probably
be related to premature delivery. Although PPM rarely causes
blindness among ocular anomaly, it does harm to vision. For young
patients, their retina is still in developing stage, best option is
excising PPM to let light irradiate macular.
Acknowledgement
We thank the patient’s parents for providing permission to share the patient’s information.
References
- Nie WY, Wu HR, Qi YS (2008) A pilot study of ocular diseases screening for neonates in China. Zhong Hua Yan Ke Za Zhi 44(6): 497-502.
- Miller SD, Judisch GF (1979) Persistent pupillary membrane: successful medical management. Arch Ophthalmol 97(10): 1911-1913.
- Meyer RB, Thill M, Vujancevic S (2010) Conservative management of bilateral persistent pupillary membranes with 18 years of follow-up. Graefes Arch Clin Exp Ophthalmol 248(7): 1053-1054.
- Ramakrishnan R, Natchiar G, Michon J, Robin AL (1993) Bilateral extensive persistent pupillary membranes treated with the neodymium-YAG laser. Arch Ophthalmol 111(1): 28-32.
- Tsai YY, Chiang CC, Tsai CH (2004) Surgical technique for removing an extensive persistent pupillary membrane. J Cataract Refract Surg 30(8): 1622-1625.
© 2021 Anhuai Yang. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






