- Submissions

Full Text
COJ Nursing & Healthcare
Improving the Experience of Patients in Contact Isolation by Human Centered Design: A Proof of Concept Study using Patient Journey Mapping
Mireille Dekker1*, Judith PM Koning2, Marijke Melles2,3, Marieke H Sonneveld2, Rosa van Mansfeld1 and Irene P Jongerden3
1Department of Medical Microbiology and Infection Prevention, Amsterdam UMC, Vrije Universiteit Amsterdam, Amsterdam, the Netherlands
2Faculty of Industrial Design Engineering, Department of Human-Centered Design, Delft University of Technology, Delft, the Netherlands
3Department of Public and Occupational Health, Amsterdam Public Health research institute, Amsterdam UMC, Vrije Universiteit Amsterdam, Amsterdam, the Netherlands
*Corresponding author: Mireille Dekker, Department of Medical Microbiology and Infection Prevention, Amsterdam UMC, Vrije Universiteit Amsterdam, Amsterdam, the Netherlands
Submission: May 3, 2021Published: May 11, 2021

ISSN: 2577-2007Volume7 Issue2
Abstract
Background: Patient information provision about isolation measures is often not standardized. Moreover, it is unclear what information patients and informal caregivers need to optimize their knowledge and actual experience of contact isolation. We explored opportunities for improving the experience of patients in contact isolation from a human-centered design perspective.
Method: We used patient journey mapping and created patient personas based on observations and interviews with patients and health care workers from a hematology, surgery and acute admission ward of a Dutch university hospital.
Result: Patients differed in their experience of contact isolation; three personas were identified. The first liked being in contact isolation, the second had to get used to the measures, the third experienced contact isolation as overwhelming. Patients experienced a lack in structured and tailored information about contact isolation. Nurses confirmed this lack of structure and reported their need for clear instructions on how to inform patients and their informal caregivers and what information to provide at which point in time. By using a human-centered design approach, we created a first draft of an interactive information path for patients, informal care givers and health care workers.
Conclusion: To improve the patient experience in contact isolation, patient information could be structured throughout the patient journey. Information should emphasize the shared responsibility of isolation between patient, health care workers and informal caregivers.
Keywords: Human-centered design; Design thinking; Infection control guidelines; Infection prevention and control
Introduction
Isolation precautions, which are applied in hospitals to limit the spread of microorganisms, restrict patients in their contact with other humans [1]. Studies on contact isolation show considerable variation in the psychological consequences for patients. Some studies report a negative impact on the quality of life of patients and psychological effects such as increased anxiety, stress and depression [1,2]. Other studies reveal no negative impact or even report favorable experiences [3,4]. The mental health of patients in contact isolation is affected by many factors, including duration of isolation, fear of infection of others, frustration and boredom, inadequate supplies and inadequate information [1]. It is suggested that providing adequate information about infectious status and precautions improves accurate application of precautions by both patients and informal caregivers and the patient experience [1,2].
In practice, information provision on contact isolation is often not standardized, and it is unclear when patients are informed, and what information they receive [1]. Moreover, it is unclear what information patients and informal caregivers need to optimize their experience of isolation measures. In this paper we address these issues by adopting a human-centered design research approach; we explored the experiences and needs of patients, informal caregivers and health care workers regarding contact isolation in a non-outbreak situation, created a patient experience journey and defined patient personas. Our aim was to explore opportunities to improve the patient experience during contact isolation from a human-centered design perspective.
Material and Methods
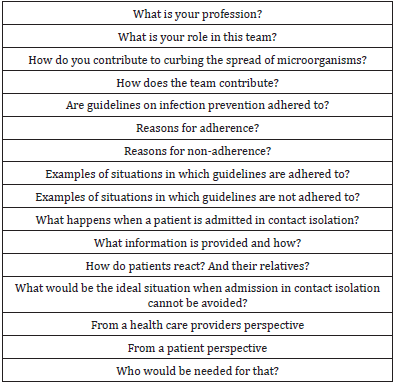
The patient experience can be described as the sum of all interactions that influence patient perceptions [5]. We used patient journey mapping to analyze the context, actors, interactions and emotions from the perspectives of patients in contact isolation and healthcare professionals that provided for their care [6]. The study was conducted between May and October 2019 on a hematology, surgery and acute admission ward of a Dutch university hospital. One researcher (JK) observed the care for patients in contact isolation and conducted semi-structured interviews with the observed patients and health care workers. The interview guides can be found in Tables 1 & 2.
Table 1:Interview guide patient.
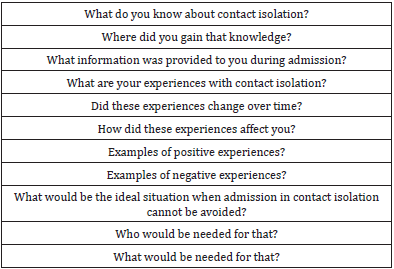
Table 2:Interview guide health care professional.
Participants were asked to participate in person during admission or during their working shifts. Interviews took place between May and July 2019 at a convenient time in a private room at the hospital. All participants provided written consent. Observations and interview fragments were used to create statement cards, define themes and ultimately create a patient journey and patient personas. In this process several ideation techniques, such as brainstorming, brain writing, mind mapping, sketching and storyboarding were applied. Nurses, infection control practitioners, a medical microbiologist, design students, design professionals and the research team were involved in ideation. A patient journey visualizes the different stages of a care pathway from the perspective of patients. It shows processes and interactions within the health care system of which the patient is part of and displays the actors that patients interact with and that affect the patient experience [7]. Personas are archetypes that describe specific user groups and help design teams to better understand the various experiences and needs of these different user groups [8]. Both patient journey and personas provide input for the development of design concepts and decisions, as they suggest what design features are necessary or have priority from a systemic, human-centered point of view.
Result
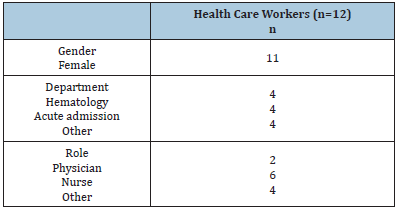
Patient care was observed for three hours in total. Eighteen semi-structured interviews were performed with patients in contact isolation (n=6) and nurses and physicians who cared for these patients (n=12) (Tables 3 & 4).
Table 3:Characteristics of patients.
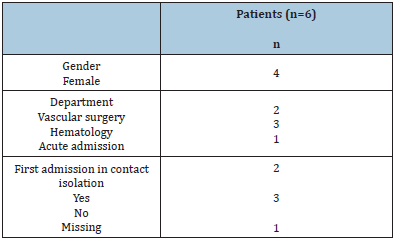
Table 4:Characteristics of health care workers.
Patient experience journey and patient personas
Based upon observations and interviews, five consecutive
phases of the patient experience journey regarding contact isolation
were identified:
A. Admission,
B. The first confrontation with isolation measures,
C. Hospital stay in isolation,
D. Hospital discharge and
E. Readmission
The full patient journey can be found in Additional file. Patients
varied in the way they experienced contact isolation and their
feelings changed during the phases of the journey. We created three
patient personas (Figure 1). The first persona liked being in contact
isolation, appreciated the fact that she did not have to consider the
needs of other patients during their stay and enjoyed being alone in
a room. The second persona had to get used to isolation but followed
what the healthcare providers thought was best for his care. The
third persona enjoyed company and therefore experienced contact
isolation as overwhelming. The need for information and the
adherence to the precautions varied per patient persona and per
phase of admission.
Information during isolation from the health care workers’ perspective
Both physicians and nurses informed patients when contact isolation was imposed, depending on who took the initiative or who came into contact with the patient first. Most information was given during this first contact. Although an information leaflet with general information on contact isolation was available, both nurses and physicians preferred to provide verbal information over a folder. Overall, physicians provided more information about the reason for isolation. Nurses were more inclined to explain the precautions to patient and family. Nurses reported a lack of clear instructions on how to inform patients and their family and what information to provide at which point in time.
Preliminary design
The design process that followed from the patient journey and personas was based on the theory of collective action. This theory concentrates on collective and shared responsibility amongst individuals and their motivations to invest in something for ‘the greater good’ [9]. This motivation can be influenced by face-toface communication, creating links between patients, health care workers and other actors, and communicating on their contribution. Our design process aimed to make the first confrontation with isolation precautions less overwhelming and to create a sense of shared responsibility for this experience among all actors, i.e. health care workers, patients and informal caregivers. A first prototyped information bundle that resulted from this process consists of five information booklets to be handed to the patient by several actors in several phases throughout the care path. An example page is given in Figure 2. It contains information on contact isolation and instructions for health care workers to discuss five subjects relevant to contact isolation: general information, implications for patients, implications for health care workers, implications for visitors and information on when measures do not longer apply. It creates an information path with guidance for health care workers.
Figure 1: Personas of patients in contact isolation.
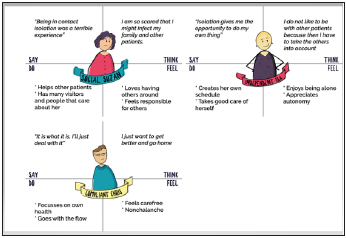
Figure 2: Example page of the information bundle.
Discussion
We found that patients differ in their experience of contact
isolation from being overwhelmed to being compliant or
appreciating the isolation. Information about contact isolation
was neither universally structured nor tailored to patient needs.
Informing patients about what is happening and why, and
explaining how long the precautions will continue, is suggested
to make the isolation more tolerable [10]. This information
should contain practical information about the precautions and
address feelings of stress and fear, which are considered normal in
isolation [1,2]. Our findings support these insights. Furthermore,
our suggested information bundle aims to provide this practical
information as well as to address experienced feelings of stress and
fear. The information bundle can elicit conversations between the
patient and health care worker. This way, it provides opportunities
to personalize the information and support health care workers
in order to meet the needs of the individual patient. This is in line
with previous suggestions that each individual requires support
and care in their own specific way, even when applying uniform
isolation policies [11].
Our information bundle focuses on joint efforts of patients,
family and health care workers, thereby stimulating the involvement
of family and friends to minimize adverse psychological effects
of isolation [12]. To create this joint sense of responsibility and
stimulate individual actors to invest in the common objectives
of limiting the spread of (multi drug resistant) micro-organisms
and limit negative impact of isolation, the theory of collective
action was applied in our design [10]. We hypothesize that with
the help of this information bundle we can connect the goals and
contributions of patients, health care workers and other actors
to electively engage all individuals will engage electively and that
the effort of each individual is noticed [9]. The number of patient
interviews in our study was limited. Our findings may therefore
not provide a complete overview of patient personas. However, the
results were complemented with observations of care situations
and interviews with healthcare workers. With this human-centered
design approach, we created a real-life patient journey of patients
in contact isolation an innovative tool that can be used to guide
provision of information on infection prevention measures.
Conclusion
The patient experience in contact isolation could be improved by providing more structured information, with a sense of shared responsibility for applying the precautions and informing each other about the process and experience of contact isolation. Using personas could help tailor this structured information to the individual patient needs. We incorporated this hypothesis into the suggested information bundle which is a first step in improving the experience of patients in contact isolation. To optimize this proposal, further iterations should be developed with the theory of collective action, patient personas and the various phases during contact isolation in mind.
Acknowledgement
We gratefully acknowledge all participating patients and health care workers of the hematology, surgery and acute admission ward of Amsterdam UMC, location VUmc.
Ethics Approval and Consent to Participate
The medical ethical committee of the Amsterdam UMC, Vrije Universiteit Amsterdam waived ethics approval (protocol number FWA00017598). All interviewees provided a written consent.
References
- Abad C, Feardy A, Safdar N (2010) Adverse effects of isolation in hospitalised patients: a systematic review. J Hosp Infect 76(2): 97-102.
- Guilley LB, Bourigault C, Guilledes BAC, Birgand B, Lepelletier D (2017) Adverse effects of isolation: a prospective matched cohort study including 90 direct interviews of hospitalized patients in a French University Hospital. Eur J Clin Microbiol Infect Dis 36(1): 75-80.
- Chittick P, Koppisetty S, Lombardo L, Vadhavana A, Solanki A, et al. (2016) Assessing patient and caregiver understanding of and satisfaction with the use of contact isolation. Am J Infect Control 44(6): 657-660.
- Wassenberg MWM, Severs D, Bonten MJM (2010) Psychological impact of short-term isolation measures in hospitalised patients. J Hosp Infect 75(2): 124-127.
- Wolf CPXP, Jason A (2014) Defining patient experience. PXJ 1(1): 7-19.
- Melles M, Albayrak A, Goossens R (2021) Innovating health care: Key characteristics of human-centered design. Int J Qual Health Care 33(1): 37-44.
- Carayon P, Albayrak A, Goossens RHM (2021) Macroergonomics of patient work: engaging patients in improving sociotechnical context of their work. In: Holden RJ & Valdez RS (Eds.), The Patient Factor: Theories and Methods for Patient Ergonomics. Boca Raton, CRC Press, USA.
- Carthy S, Raghallaigh P, Woodworth S, Lim YL, Kenny LC, et al. (2016) An integrated patient journey mapping tool for embedding quality in healthcare service reform. J Decis Syst 25(1): 354-368.
- Meinzen DRS, Gregorio M (2004) International food policy research institute, Collective action and property rights for sustainable development. Washington, USA.
- Nair R, Perencevich EN, Goto M, Livorsi DJ, Balkenende E, et al. (2020) Patient care experience with utilization of isolation precautions: systematic literature review and meta-analysis. Clin Microbiol Infect 26(6): 684-695.
- Barratt R, Shaban R, Moyle W (2010) Behind barriers: patients' perceptions of source isolation for methicillin- resistant staphylococcus aureus (MRSA). Aust J Adv Nurs 28(2): 53-59.
- Rump B, Timen A, Verweij AM, Hulscher M (2019) Experiences of carriers of multidrug-resistant organisms: a systematic review. Clin Microbiol Infect 25(3): 274-279.
© 2021 Mireille Dekker. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






