- Submissions

Full Text
COJ Nursing & Healthcare
Needs of Critically Ill Cancer Patients and their Relatives: Nursing Perspectives
Hayam Ibrahim Asfour*
Professor of Critical Care and Emergency Nursing, Saudi Arabia
*Corresponding author: Hayam Ibrahim Asfour, Professor of Critical Care and Emergency Nursing, Saudi Arabia
Submission: January 27, 2020Published: February 10, 2021

ISSN: 2577-2007Volume7 Issue1
Abstract
Background: Patients with cancer face many challenges in their treatment journey. When patients with cancer are admitted to intensive care units (ICUs), they and their families have many needs need to be met by nurses. The aim of this study was to identify needs of critically ill cancer patients’ and their relatives from the nurses’ perception.
Method: A descriptive study design was used to conduct the study. Sixty critical care nurses working in intensive care units of 10 Hospitals participated in the study. Care needs of Critically ill cancer patients and their relatives semi-structured interview schedule” was the tool used to collect data in the study. This tool covered 26 items geared towards caring of critically ill cancer patients and 30 items related to relatives’ needs in ICUs. The tool also included open questions to make nurses express their perceptions freely and strengthen the data collected.
Result: Nurses stated that ICUs accept admission of critically ill cancer patients, the more common reason is performing surgery (80%) followed by respiratory emergencies (70%), shock (50%), bleeding 40% and electrolyte disturbance (30%).Nurses agreed that care of cancer patients is the same care for any critically ill patient in general as they provide care of mechanically ventilated patients (100%), oxygen administration (60%), blood transfusion (40%), in addition to cancer-related care such as monitoring during chemotherapy & radiotherapy (50%), and they need psychological support (60%). Nurses reported that relatives of critically ill cancer patients have many needs; all nurses (100%). reported that relatives’ needs to have questions answered honestly, know how the patient was being treated, frequently see their patient, and feel that the ICU health care team cared about their patient, are essential for relatives from their point of view.
Conclusion: Critically ill cancer patients Cancer patients and their relatives have many needs, should be identified and the plan of care should meet the needs of critically ill cancer patients and their relatives.
Keywords: Needs; Critically ill cancer patient; Relatives; Intensive care units
Introduction
Care of patients in intensive care units (ICUs) need highly qualified health care team including nurses. Critical care nurses provide high skilled evidence-based care for all admitted patients to critical care units. Patients are admitted to critical care units for many reasons as they have or at risk for life-threatening problems mainly; respiratory, circulatory, neurological and renal. Patients with cancer are exposed to different treatment modalities such as surgery, chemotherapy, radiation and others. Taccone et al. [1] studied the characteristics and outcomes of patients with cancer in CCUs and reported that a large proportion of patients in ICUs had cancer. It was reported that every sixth to eighth critical care unit patient admitted because of the underlying malignant disease [1,2]. Patients with cancer may be admitted to ICUs for treatment of the associated side effects of cancer management or for follow-up treatment [2]. Many cancer- related complications such as malignancy-related airway obstruction, hyperleukocytosis, tumor lysis syndrome, drug reactions to immune and/or chemotherapy, stem cell transplant-associated conditions, hemorrhage, electrolyte disturbances, and thrombotic microangiopathies are considered causes for admission of patients with cancer to ICUs. Cancer was not considered from the admission criteria to ICUs, in the past. However, patients with advanced complications related cancer may develop multiple distressing symptoms which result in admission to ICUs [3-5].
Despite the advances in technology and science which aid in prevention, early detection, management of cancer, the incidence, consequences of cancer on the patients, their families/relatives and the society still high. Studies reported that the mortality rate because of cancer is higher than all types of stroke and cardiovascular diseases. In
addition, the mortality rate is high in hospitals especially in ICU
[3-6]. Azoulay et al. [4], studied the prevalence and factors of ICU
and found that conflicts care of critically ill patients with cancer
may have a negative impact on the patient, their family, and the ICU
team members. The nature of cancer & its consequences, and the
uncertainty about the future, make the patients and their relatives
suffer from a lot of physiological, and psychological problems.
Therefore, they need extra-care to meet their physiological,
psychological, and spiritual needs4. Nurses’ role for care of
critically ill cancer patients focuses on assessing, educating the
patients, coordination of care, provision of direct care, symptom
management, and supportive care [7-9]. Critically ill cancer patients
-despite the innovative therapies- may be near the end of life and can
have several episodes of clinical deterioration because of increasing
tumor burden or as a side-effect of therapies. Hillman [10] & Jones
et al. [11] stated that aggressive interventions may not always be in
the preferred measure. Similarly, Khan et al. [12] revealed that goals
of care in the stage of life, should be focused on decreasing suffering
and distress by alleviating the symptoms. These interventions are
recognized as critical components of excellent end of life care for
patients, family and nurses, and can be implemented in intensive
care units. Care of patients with cancer require nurses to be expert
in providing high quality care. It is essential to understand the
needs of patients with cancer in order to provide effective ways of
caring. Care of patients with cancer is based on many aspects of
care such as emotional and the moral, cognitive aspect, perception,
and knowledge. Cancer affects family members and relatives. The
diagnosis of cancer precipitates complex feelings and changes in
the lifestyle which become as overwhelming for patients ‘family
and relatives. Relatives of critically ill cancer patients may have
many physiological, psychological changes as they support, help,
and provide care for their patients. The relatives were suffering
from many unexpected bad experiences with these patients during
their journey of treatment from cancer. When patients with cancer
are admitted to ICUs, sufferings of their families increased as they
may have little experience with life-threatening illness, they even
feel don does not know how and what to do for their patients.
Recognizing the relatives’ needs and meeting them will have an
important role in improving the quality of patient care and the
quality of their life [8-10].
Patients with cancer and their families often need to understand
what is happening in the critical care unit, they discuss the reasons,
advantages of being on mechanical ventilation, renal replacement
therapy, vasoactive agents, or other life-sustaining treatments
modalities in ICUs. They also have unsolved queries about whether
part or all these supportive therapies can be administered with
cancer-specific treatments, including chemotherapy at the same
time. More recently, the lack of survival benefit in patient with
cancer who is admitted to ICUs with multiple organ failure has
raised concerns about the timing of ICUs’ admission [4,5]. Han et
al. [13] investigating the coping styles and social support among
relatives of patients with cancer and reported that both patients
and their relatives need support in order care for patients during
this challenging time and to cope with presence of this disease.
Many studies reported that effective care of critically ill cancer
patients rely on identifying and meeting their needs [14-16]. There
are few studies examined the needs critically ill cancer patients and
their relatives from the nursing perspectives. Therefore, this study
was conducted to identify critically ill cancer patients and relatives’
needs from the nursing perspectives. In order to achieve this aim,
the following research question was addressed; what are the needs
of critically ill cancer patients and their relatives in intensive care
units?
Methods
A. Study design: A descriptive study design was used in this study.
B. Setting: The study was conducted in 10 intensive care units in Alexandria (2 ICUs in a university teaching hospital, 2 ICUs of a health insurance hospital, 6 ICUs in private hospitals).
C. Participants: the participants were chosen through the purposive sampling technique who were providing care for critically ill cancer patients and communicating with their relatives. Sixty critical care nurses working in the previously mentioned ICUs agreed to participate in the study. Nurses were distributed as their working ICU; 9 from ICUs of the university teaching hospital, 6 from ICUs of the Health Insurance Hospital, and 45 nurses from ICUs of the private hospitals.
D. Tool: Care needs of Critically ill cancer patients and their relatives semi-structured interview schedule”, this tool was developed by the researchers based on reviewing the related literature [14-20]. It was used to describe the needs of critically ill patients and their families in intensive care units. This tool covered 26 items geared towards caring of critically ill cancer patients and 30 items related to relatives’ needs in ICUs. These items were distributed into six main broad categories of (CANCER) including the following: (C) Criteria and causes for admitting cancer patients to ICUs, (A) Action; the medical/surgical actions performed to the critically ill cancer patients in ICUs, (N) Nursing; nursing interventions performed to the critically ill cancer patients in ICUs, (C) Communication needs for the critically ill cancer patients in ICUs, the (E) End of life care performed to the critically ill cancer patients in ICUs, and (R) Relative’ needs; this part measured nurses’ perceptions of the needs of relatives of critically ill cancer patients. All parts were scored using 5 points Likert scale ranging from 0 to 4 (0=not important at all to 4=Absolutely Essential). The tool also includes open questions to make nurses express their perceptions freely and strengthen the data collected. Tool preparation, validity, and reliability: The tool of the study was developed by the researcher based on reviewing the related literature [14-20] and tested by five academic experts (three from the Faculty of Nursing and two from the Faculty of Medicine of University of Alexandria), and 10 nurses from hospitals for content related validity and the necessary modifications were done accordingly. The tool was tested for its reliability using interrater reliability. The reliability coefficient was (r) =0.83). A pilot study was conducted on 5 nurses to test the clarity, applicability and feasibility of the tool (those nurses were not included in the study). Appropriate modifications were performed prior to data collection for the actual study.
Procedure
To collect data, semi-structured interviews were held from the beginning of June to the end of August 2018. Each nurse was interviewed individually once by the researchers using the tool. Nurses were interviewed in the morning, afternoon, and at the beginning of the night shift during their break time. Each interview lasted from 20 to 30 minutes. Data were coded and entered in statistical program to be analyzed. Administrative design and Ethical considerations: A letter was submitted to the ethical committee and hospitals directors contains the purpose, the required participants, the tool, and methods of data collection of the study to obtain their approval. Before starting the interviews, an explanation of the study aim was done and the confidentiality, anonymity, right, refuse to participate, or withdraw from the study were emphasized to them. Consent was taken from nurses who agreed to participate in the study.
Statistical Analysis
The data were entered into SPSS system files (SPSS package version 20) using personal computer. Output drafts were checked against the revised coded data for typing and spelling mistakes. Finally, analysis and interpretation of data were conducted. Descriptive statistics including frequency and distribution were used to describe different characteristics.
Result
The results of the study are illustrated in two parts: nurses’ perception of care of critically ill patients with cancer and regarding their role toward relatives of critically ill patients with cancer. Part I: Nurses’ perception of care of critically ill patients with cancer Nurses stated that ICUs accept admission of critically ill cancer patients. Regarding criteria/reasons of admission to ICUs; the more common reason is performing surgery (80%) followed by respiratory emergencies (70%), shock (50%), bleeding 40% and electrolyte disturbance (30%). As for the medical/surgical actions performed to the critically ill cancer patients in ICUs; the most performed actions were administration of analgesics (70%), initiation of mechanical ventilation (60%), and monitoring effects of chemotherapy & radiotherapy (50%) as shown in (Table 1).
Table 1:Criteria for ICU admission and Medical/surgical actions performed to critically ill cancer patients in ICUs as reported by nurses.
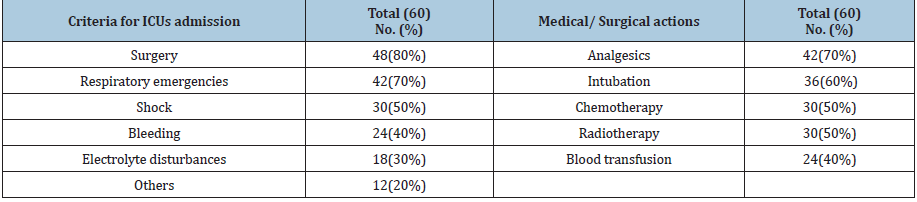
Table 2: Nursing interventions performed to the critically ill cancer patients in ICUs.
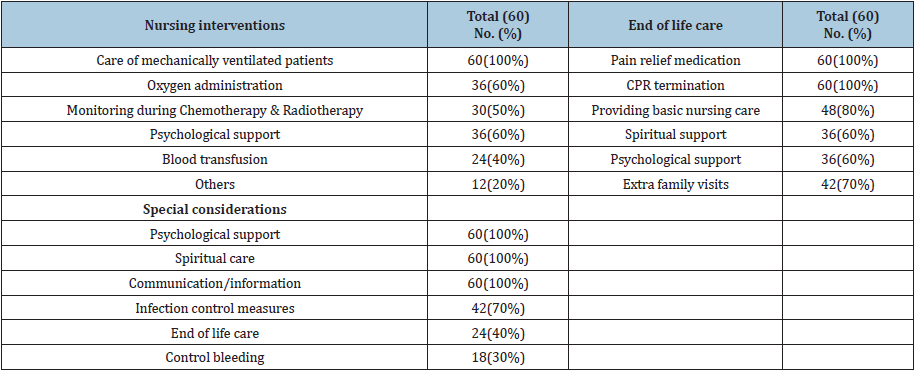
Regarding the nursing interventions performed to the critically
ill cancer patients in ICUs (Table 2); nurses agreed that care of cancer
patients is the same care for any critically ill patient in general
as they provide care of mechanically ventilated patients (100%),
oxygen administration (60%), blood transfusion (40%), in addition
to cancer-related care such as monitoring during chemotherapy &
radiotherapy (50%), and they need psychological support (60%).
There are special considerations for care of critically ill cancer
patients as reported by nurses such as psychological/spiritual
care and communication and information (100%), strict infection
control measures (70%), and control of bleeding (30%). As for
the end-of-life care, many aspects are performed for critically ill
cancer patients such as administration of pain relief medications
and termination of CPR (100%), basic nursing care (80%),
psychological/spiritual care (60%), and allowing extra visits for
relatives (70%) were provided to the critically ill cancer patients
in ICUs as end-of-life care measures. Part II: Nurses’ perception
regarding their role toward relatives of critically ill patients with
cancer: nurses stated that admitting cancer patients to the ICUs
means a lot of cost, stress, and depression to their relatives. As
stated by nurses, relatives had feelings of sadness, depression and
were crying and over-caring of their patients.
Nurses reported that relatives of critically ill cancer patients
have many needs; all nurses (100%) reported that relatives’
needs to have questions answered honestly, know how the patient
was being treated, frequently see their patient, and feel that the
ICU health care team cared about their patient, are essential for
relatives from their point of view. Most nurses reported that the
essential relatives’ needs are to know the prognosis, talk with the
nurse each day (98.33%) followed by; understand the reasons
behind the especial management performed for their patient, be
informed about any changes in the patient’s condition even they
are at home, and their patient is receiving the best possible care
(96.67%) and receive information daily regarding the condition of
their patient, have adequate explanations of understandable terms
related to their patient that are and talk to the doctor every day
(90%). However, some relatives’ needs are of little importance or
not important at all from the nurses’ perspectives such as have a
telephone in the waiting room (13.33% and 48.33%), regarding
social support; relatives need to be told about other hospital staff
who could help with their problems (20 &30%), know types of
ICU staff who is taking care of their patient (20 &30%), and have
explanations/orientation of the ICU environment before admission
(18.33 &20%) as shown in (Table 3).
Table 3: Needs of critical cancer patients as perceived by nurses.

Discussion
Intensive care unit admission of critically ill cancer patients
had many challenges in the past two decades. Many ICUs were
refusing the admission of cancer patients because many their
chronic disease, options of treatment are limited, patients spend a
little time in ICU& die before ICU discharge. In-hospital mortality
rates for cancer patients are less than mortality rates of critically
ill patients [3]. However, the survival rates of critically ill cancer
patients are less than other critically ill patients. In this study,
nurses accepted the rights of critically ill cancer patients to be
admitted to ICUs and have the required care. This is in line with
Azoulay et al. [9] who reported acceptance of critically ill cancer
patients’ admission to the ICUs which lead to improvement in the
survival rates of these critical ill patients. This improvement in
survival rate was reported in many studies for patients who needed
management with vasopressors, mechanical ventilation, and renal
replacement therapy. Studies found that appropriate admission
of critically ill cancer patients help improving their disorders and
their survival rate [2,4,5].
The findings of this study revealed that the criteria for
admitting cancer patients to ICUs from nurses’ point of view are
surgery, respiratory emergencies, shock, bleeding, and electrolyte
disturbance. Several studies agreed with our results and revealed
that managing cancer patients in ICUs through using of more targeted
therapeutic regime, providing intensive chemotherapy treatments
and innovative therapeutic approaches especially for cancerrelated
complications resulted in improving the cancer cure rate.
Cancer-related complications can lead to organ dysfunction mainly
respiratory failure which necessitates ICU admission. Management
of cancer patients with organ dysfunction requires specialized
skills and holistic care which is received in ICUs [3]. Critically
ill cancer patients receive many ICU actions as they conditions
require. In this study, nurses stated that critically ill cancer patients
admitted to ICUs to receive analgesics, intubation, chemotherapy
& radiotherapy, and blood transfusion. This was also reported by
many studies, who is stated that cancer patients admitted to ICUs
for mechanical ventilation support, renal replacement therapy, and
vasopressors and monitoring for chemotherapy & radiotherapy
[5-13]. In this regard, a general improvement in CCUs mortality
of cancer patients was reported over time, the reason for this
improvement may because of improvement of ICU management,
development of more targeted therapies, using more intensive
chemotherapeutic treatments, and advances in supportive care
[3,12,20]. Soares et al. [4], stated that advances in oncology and
intensive care are probably being translated into a better outcome
[21].
Care of critically ill cancer patients as care for any critically ill
patients as nurses stated in this study and added that those patients
need more psychological support and communication. Critically
ill cancer patients most important needs include management
of manifestations, psychological, emotional, and social spiritual
needs. Meticulous care of these patients during the ICU period is
essential to ensure successful outcomes. Critical care nurses must
identify and interpret patients’ manifestations for formulating the
required plan of care [22-24]. Critically ill cancer patients may be
admitted post-operative, and intubated, have multiple connections
need continuous monitoring and high-quality nursing care. Nurses
reported that, cancer patients have many aspects of care in ICU
such as management for the artificial airway, care for patients
with mechanical ventilation, management of pain, electrolyte
disturbances and others. Critically ill patients have many
psychological and emotional problems such as anxiety, fear, and
depression. Therefore, they need support and reassurance [24,25].
Relief of pain, providing emotional and psychological support are
main aspects of care of critically ill cancer patients as perceived by nurses. Collins et al. [17] stated that the five important roles of care
of critically ill cancer patients are being with the patient, vigilant
respiratory system assessment, patient education and support of
family or caregivers, care coordination, and pain management.
There are significant communication exchanges between patients
and non-physician health professionals [26]. Critically ill patients
in general have a low immunity because of many factors; such as
their disorders, age, invasive lines and machines, and malnutrition.
Critically ill cancer patients may be under chemotherapy which
make them at-risk for many complications. Critical care nurses
present all the time with patients and see their sufferings and the
effects of therapy on them which result in alterations in their selfesteem
and body images [3,25,26]. Therefore, nurses reported that
there are special considerations for their care, which are infection
control measures, communication/information spiritual care,
psychological support, and end of life care.
These considerations were assured by many studies.
Communication needs are essential for critically ill cancer
patients because they suffered a lot from cancer and cancerrelated
management & complications. These patients be afraid,
anxiety, depression and may lose their hope to retain to their
lives. ICUs are full of machines, noise, life-threatening conditions,
and resuscitation efforts, which precipitate stress for patients. In
addition, ICU admission make them think that the life will end in
the ICU. All patients need to have explanation for everything done
for them, they need to practice their right to decide what will be
done for them if they can, they can participate in their care and
need everyone to dealt with them with trust of their power and
respect [3,25-28]. Nurses allow the critically ill cancer patients to
express their thoughts, and talk freely about their fear, sadness, and
anxiety. Critically ill cancer patients need to have the care provider
to be with them in all their suffers and help them to combat their
disease and cancer related- complications [25].
Termination of CPR is performed for terminally ill cancer
patients as our results revealed. This agrees with Gendt et al. [27]
who reported that nurses may decide not to start cardiopulmonary
resuscitation (CPR) for a patient without DNR status as it is
considered a futile procedure for them. Providing a good death was
the major theme of the result of Beckstrand [28] study and specific
suggestions were offered to ensure death with dignity and peace.
His study listed critical care nurses’ suggestions to improve endof-
life care in ICUs which are; management of pain & discomfort,
recognizing and following the patient’s wishes regarding end-oflife
care, promoting of earlier termination of aggressive treatment,
not allowing the patient to die alone, communicating effectively
as a healthcare team, and educating others about quality end-oflife
care [28]. a major ethical issue facing nurses in ICUs is donot-
resuscitate (DNR). Many critically ill cancer patients have
DNR order which means providing care including all medical
interventions except vasopressors, and CPR but providing spiritual
care, pain relief management, comfort measures, and other basic
patients’ needs [29-31].
The most technologically sophisticated care is provided for
patients in ICU, to manage their life-threatening problems, while
restoring the quality to their lives. Many studies have reported that
nurses participate in end-of-life decision making with the other
health care team and provide care for patients and their relatives
in this stage. In this study, nurses reported that patients’ needs for
spiritual and psychological care. They need to feel that all people
care of them, they need to see their relatives and closed ones.
Nurses stated that they try to allow more flexible visiting hours. In
the same line, Carlson et al. [32] reported that nurses allow more
free visiting hours as they can and, in some cases, nurses tend to
decrease the visiting time as the patients ‘condition allow. Some
studies revealed that nurses may restrict relatives visit if the ICU is
busy [33-35]. However, in other studies, nurses insist on restrictions
in the visiting hours because they see that ICU is a busy work area,
too small to care for patient and allow for extra-visitation at the
same time. Pediatric nurses were very resistant to allow parents
to visit their children despite they perceived themselves as family
friends [36]. Relatives of critically ill cancer patients have many
emotional and psychological problems. They are with their patients
in all the disease process. Relatives of critically ill cancer patients
are always presenting and share in making crucial decisions about
the patients’ care & management. Studies found that the most
important relatives needs are; to be present with their patients as
they can, information needs, and can ventilate their feelings.
The top important relatives’ needs as reported by Ghabeesh et
al. [31], are being certain that the care given for their patients is
the best, health team members are caring about their patients, and
the health team members answer their questions honestly. In our
study nurses’ perceived relatives’ needs are more than important
for them, they express their understanding of their sufferings
with their patients. Nurses demonstrated that the most important
relatives’ needs are; information needs {answering the questions
honestly, know the progress of their patients frequently, can be
informed about any changes in their patients’ conditions even if
they are at home, security& assurance needs such as know how
their patients was being treated and managed in the ICU, assure
that the health care team care about their patients, can talk with
the health care team as they need, and have adequate explanation
for what is being done for their patients, and support & comfort
needs such as {can see the patient frequently, and have support
from others, and can express their feeling.
Results of the study are consistent with many studies. Maxwell et
al., revealed that the most important relatives’ needs are, assurance,
and information regarding management of patients in ICU. Safety
and information needs are the most important relatives’ needs
as reported by Padilla-Fortunatti et al. [29]. Ashrafian et al. [30]
described the relatives’ needs as social, cognitive, and psychological
needs and stated that relatives’ needs are important. However,
some of these needs are not perceived valuable by the health care
team and not met effectively, such as giving the relatives the needed
explanation and information, understanding of the heath care team of their feelings and sufferings, and communication needs. Many
important decisions are taken by the critically ill cancer patients
‘relatives in ICUs, therefore, relatives of these patients need enough
information, explanation of difficult complex medical issues,
empathy, psychological support to relieve their anxiety and help
them to have at least a comfortable life while their patients in the ICU
[37-42]. This study raises the issues of needs of critically ill cancer
patients and their relatives in ICU regarding support either through
giving adequate clear information, effective communication and
psychological support. This study described the needs of critically
ill cancer patients and their relatives from the nursing perspectives.
Data collection in this study was conducted in different hospitals
including private, health insurance and university hospitals which
is considered a strength for this study. However, there are some
limitations of this study, identifying critically ill cancer patients
and relatives’ needs from only the nurses’ perspectives, it
may be more relevant to take the perceptions of critically ill cancer
patients and their relatives to determine their needs. In addition,
limited studies performed regarding needs of critically ill cancer
patients and their relatives made the discussion difficult.
Conclusion
Management of critically ill cancer patients is a challenging task. Nurses stated that the criteria for admitting cancer patients to ICUs are surgery, respiratory emergencies, shock, & bleeding and electrolyte disturbance. Critically ill cancer patients admitted to ICUs to receive analgesics, intubation, chemotherapy & radiotherapy, and blood transfusion. Care of critically ill cancer patients is the same care of any critically ill patient. Critically ill cancer patients need special approaches for communication. Relatives of critically ill cancer patients have many needs include information, communication, and psychological needs.
Acknowledgment
The researchers are grateful to nurses of the selected critical care units for their cooperation and participation in this study. Special thanks to all hospital’s administrators for their cooperation.
References
- Taccone FS, Artigas AA, Sprung CL, Moreno R, Sakr Y, et al. (2009) Characteristics and outcomes of cancer patients in European ICUs. Crit Care 13(1): R15.
- Schellongowski P, Kiehl M, Kochanek M, Staudinger T, Beutel G (2016) Intensive care for cancer patients: An interdisciplinary challenge for cancer specialists and intensive care physicians. memo 9: 39-44.
- Burlá C, Py L (2014) Palliative care: science and protection at the end of life. Cad Saúde Pública 30(6): 1139-1141.
- Azoulay E, Soares M, Darmon M, Benoit D, Pastores S, et al. (2011) Intensive care of the cancer patient: recent achievements and remaining challenges. Ann Intensive Care 1(1): 5.
- Agostino R, Halpern N (2010) Acute care nurse practitioners in oncologic critical care: the memorial sloan-kettering cancer center experience. Crit Care Clin; 26(1): 207-217.
- Pessini L (2016) Life and death in the ICU: ethics on the razor’s edge. Rev Bioét 24(1):54-63.
- Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, et al. (2015) Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 136(5): E359-E386.
- Lawson A, Farquhar P (2010) The patient with cancer in intensive care. JICS 11(4): 228-240.
- Azoulay E, Piers RD, Ricou B, Ganz FD, Max A, et al. (2014) Inappropriate care in European ICUs: confronting views from nurses and junior and senior physicians. Chest 146(2): 267-275.
- Hillman K (2010) Dying safely. Int J Qual Health Care 22(5): 339-340.
- Jones D, Mitchell I, Hillman K, Story D (2013) Defining clinical deterioration. Resuscitation 84(8): 1029-1034.
- Khan S, Gomes B, Higginson I (2013) End-of-life care: what do cancer patients want? Nat Rev Clin Oncol 11: 100-108.
- Stenberg U, Ruland CM, Miaskowski C (2010) Review of the literature on the effects of caring for a patient with cancer. Psychooncology 19(10): 1013-1025.
- Jongerden IP, Slooter AJ, Peelen LM, Wessels H, Ram CM, et al. (2013) Effect of intensive care environment on family and patient satisfaction: a before-after study. Intensive Care Med 39(9): 1626-1634.
- Han Y, Hu D, Liu Y, Lu C, Luo Z, et al. (2014) Coping styles and social support among depressed Chinese family caregivers of patients with esophageal cancer. Eur J Oncol Nurs 18(6): 571-577.
- Hashim F, Hussin R (2012) Family needs of patient admitted to intensive care unit in a public hospital. Proc Soc Behav Sci 36: 103-111.
- Collins A, Garner M (2007) Caring for lung cancer patients receiving photodynamic therapy. Crit Care Nurse 27(2): 53-60.
- Mistraletti G, Umbrello M, Mantovani ES, Moroni B, Formenti P, et al. (2017) A family information brochure and dedicated website to improve the ICU experience for patients’ relatives: an Italian multicenter before-and-after study. Intensive CareMed 43(1): 69-79.
- Adams A, Mannix T, Harrington A (2015) Nurses’ communication with families in the intensive care unit-a literature review. Nurs Crit Care 22(2): 70-80.
- Khalaila R (2013) Patients’ family satisfaction with needs met at the medical intensive care unit. J Adv Nurs 69(5): 1172-1182.
- Maxwell KE, Stuenkel D, Saylor C (2007) Needs of family members of critically ill patients: a comparison of nurse and family perceptions. Heart Lung 36(5): 367-376.
- Obringer K, Hilgenberg C, Booker K (2012) Needs of adult family members of intensive care unit patients. J Clin Nurs 21(11-12): 1651-1658.
- Cameron JI, Chu LM, Matte A, Tomlinson G, Chan L, et al. (2016) One-year outcomes in caregivers of critically ill patients. N Engl J Med 374(19): 1831-1841.
- Davidson JE, Jones C, Bienvenu OJ (2012) Family response to critical illness: postintensive care syndrome-family. Crit Care Med 40(2): 618-624.
- Broek JM, Reinders AHB, Zedlitz AMEE, Girbes ARJ, Jonge E, et al. (2015) Questionnaires on family satisfaction in the adult ICU: a systematic review including psychometric properties. Crit Care Med 43(8): 1731-1744.
- Shorofi S, Jannati Y, Moghaddam H, Charati J (2016) Psychosocial needs of families of intensive care patients: perceptions of nurses and families. Niger Med J 57(1): 10-18.
- Gendt C, Bilsen J, Stichele R, Noortgate N, Lambert M, et al. (2007) Nurses' involvement in 'do not resuscitate' decisions on acute elder care wards. J Adv Nurs 57(4): 404-409.
- Beckstrand R, Callister L (2006) Kirchhoff K. Providing a "good death" critical care nurses' suggestions for improving end-of-life care. American Journal of Critical Care 15(1): 38-45.
- Fortunatti CP, Silva N, Rojas MA, Munoz M (2018) Needs of relatives of critical patients in an academic hospital in Chile. Intensive Nursing 29(1): 32-40.
- Ashrafian S, Feizollahzadeh H, Rahmani A, Davoodi A (2018) The unmet needs of the family caregivers of patients with cancer visiting a Referral Hospital in Iran. Asia Pac J Oncol Nurs 5(3): 342-352.
- Ghabeesh SH, Snieneh H, Shahror L, Sneineh F, Alhawamdeh M (2014) Exploring the Self-Perceived Needs for Family Members Having Adult Critically Ill Loved Person: Descriptive Study. Health 6(21): 3005-3012.
- Carlson B, Riegel B, Thomason T (1998) Visitation: policy versus practice. Dimens Crit Care Nurs 17(1): 40-4 7
- Gurley MJ (1995) Determining ICU visiting hours. Medsurg Nurs 4(1): 40-43.
- Clark AP, Carter PA (2002) Why do nurses see families as “trouble?” Clin Nurse Spec 16(1): 40-41.
- Griffin T (2003) Facing challenges to family centered care. I: Conflicts over visitation. Pediatr Nurs 29(2): 135-137.
- Maxton FJ (1997) Old habits die hard: Changing paediatric nurses’ perceptions of families in ICU. Intensive Crit Care Nurs 13(3): 145-150.
- Rowland C, Hanratty B, Pilling M, Berg BD, Grande G (2017) The contributions of family care-givers at end of life: a national post-bereavement census survey of cancer carers’ hours of care and expenditures. Palliat Med 31(4): 346-355.
- Sklenarova H, Krümpelmann A, Haun MW, Friederich KC, Johannes H, et al. (2015) When do we need to care about the caregiver? Supportive care needs, anxiety, and depression among informal caregivers of patients with cancer and cancer survivors. Cancer 121(9): 1513-1519.
- Rha SY, Park Y, Song SK, Lee CE, Lee J, et al. (2015) Caregiving burden and the quality of life of family caregivers of cancer patients: the relationship and correlates. Eur J Oncol Nurs 19(4): 376-382.
- Clark K (2017) Care at the very end-of-life: dying cancer patients and their chosen family’s needs. Cancers 9(2):11
- Cui J, Song LJ, Zhou LJ, Meng H, Zhao JJ, et al. (2014) Needs of family caregivers of advanced cancer patients: a survey in Shanghai of China. Eur J Cancer Care 23(4): 562-569.
- Mosher CEP, Adams RN, Helft PR, Neil BHO, Shahda S, et al. (2016) Family caregiving challenges in advanced colorectal cancer: patient and caregiver perspectives. Support Care Cancer 24(5): 2017-2024.
© 2021 Hayam Ibrahim Asfour. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






