- Submissions

Full Text
COJ Nursing & Healthcare
Mental Health Issue of Health Care Professionals During COVID-19 Pandemic: A Rapid Review
Xiong CL1* and Hematram Yadav2
F1Department of Social and Preventive Medicine Public Health, Faculty of Medicine, Malaysia
F2Public Health Consultant, Ex-Director of Family Health, Ministry of Health, Malaysia
*Corresponding author: Xiong CL, Department of Social and Preventive Medicine Public Health, Faculty of Medicine, University of Malaya, Jalan University, Wilayah Persekutuan Kuala Lumpur, Malaysia
Submission: June 26, 2020Published: December 22, 2020

ISSN: 2577-2007Volume6 Issue5
Abstract
Aim and objectives: To estimate the mental health status of health care professionals during COVID-19 pandemic.
Background: During this COVID-19 pandemic, health professionals face mental health challenges including stress, anxiety and depression, and insomnia. The mental health issues could be due to COVID- 19 cases in the community and in hospitals.
Methods: A meta-analysis was done on the mental health status of health professionals during the COVID-19 pandemic globally. The English and Chinese database were searched for the purpose of this review and the data bases included PubMed, PubMed Central, Web of Science from the Cochrane Library, and China National Knowledge Infrastructure. The review included 26 studies published from February 18 to April 28, 2020. Inclusion criteria and exclusion criteria were set before screening the data base.
Result: The prevalence of stress among health professionals was 31.3%, depression 25.2%, anxiety 28.5% and insomnia was 45.5% in Wuhan, Hubei province of China. However, the prevalence of stress was 53.1%, depression was 34.0% anxiety 33.0% and insomnia was 14.1% in other parts of China. The prevalence of insomnia among health workers was higher in Hubei province compared to other provinces, 45.5% and 33.5% respectively Health professionals with psychological distress or severe mental health issues were reported higher in Hubei province (24.5%) compared with other provinces in China (14.1%). This meta-analysis shows that there is high incidence of mental health issues in the areas affected by COVID-19 compared to the other provinces.
Conclusion: Currently there is very little attention provided to mental health issues in the general population and to the health professionals in the COVID-19 affected areas. There is an urgent need to implement mental health issues interventions in countries affected by COVID-19.
Keywords: Coronavirus 2019; COVID-19; Mental health; Stress; Health professionals
Introduction
COVID-19 was first noticed in Wuhan, Hubei Province in China in December 2019 before it became a pandemic. The World Health Organization (WHO) announced the outbreak of a new coronavirus disease, COVID-19, as a Public Health Emergency of International Concern (PHEIC) in January 2020 [1]. COVID-19 is a highly contagious disease and it leads to severe pneumonia, acute respiratory distress syndrome, and mortality in some cases. Higher morbidity and mortality rate is reported in some high-risk groups such as the elderly and especially those co-morbidity [2,3]. Previous experience from Severe Acute Respiratory Syndrome (SARS) and Middle Eastern Respiratory Syndrome (MERS) showed that the emerging infectious disease outbreaks always had a psychological impact on generally population and health care professionals. The rapid transmission and uncertainty of the prognosis of COVID-19 resulted in different levels of mental health issues among the general population [4-6].
The Personal Protective Equipment (PPE), intensive care unit beds, and ventilators may not be able to meet the increasing number of COVID-19 cases [2,7] and this may cause mental distress among the health professionals and also in the community. During this COVID-19 pandemic, frontline health professionals face challenges including stress both physical and psychological. The mental health issues could be due to health professionals exposed to suspected and confirmed cases. Some overworked health professionals experience stigma or even fear from their families and the community. These situations
has resulted in several publications on mental health issues
among the general population as well among health professionals
during this COVID-19 pandemic worldwide [8-13]. The objective
of this study is to assess the mental health issues related to the
COVID-19 pandemic among health care professionals using a
Meta-analysis. Hopefully an evidence-based intervention strategy
may be developed to maintain mental wellbeing among health
professionals during this pandemic.
Methods and Materials
A meta -analysis was done using published papers from
PubMed, PubMed Central, Web of Science, the Cochrane Library,
Google Scholar, and China National Knowledge Infrastructure from
January 2020 through May 2020. The search languages used were
English and Chinese and the keywords used included coronavirus
disease 2019, COVID-19, novel coronavirus pneumonia, mental
health, depression, anxiety, insomnia, psychological distress,
stress, medical staff, health care workers, and health professionals.
The eligible articles were imported into Endnote to avoid any
duplication. Meta-analysis was performed in evaluating the pooled
effect size of depression and anxiety status because of limited
amount of data available.
Owing to the rapid and widespread of COVID-19 worldwide,
a rapid review approach was used to obtain information of this
highly transmissible disease [14]. Dual review of 25% of abstracts
was done and STROBE was not used for the quality control of the
studies that were selected and data abstraction was conducted by a
single reviewer [15].
References
Figure 1:Flow diagram of article selection.
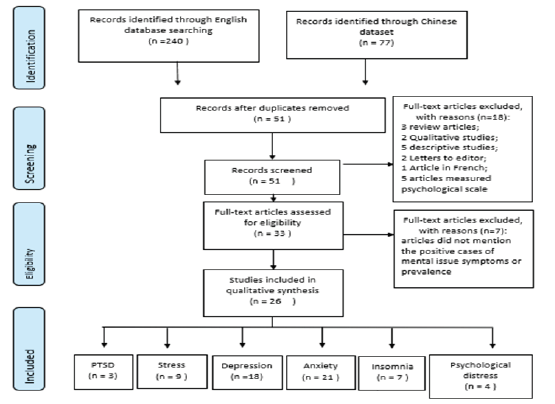
Figure 1 shows the process of how the papers were selected
for the study. A total of 317 papers were identified initially but
only 26 papers were reviewed finally. All the studies were selected
using pre-defined inclusion and exclusion criteria. Table 1 shows
the list of full text of articles assessed for eligibility. Only the crosssectional,
cohort and case-control study designs were included.
Descriptive and narrative study designs, protocols and letters
to the editor were excluded. Study population included health
professional including medical doctors, nurses, and medical
technicians who were currently working in the hospitals or in other
health settings. Data extraction was done using a Microsoft Excel
table and the main areas studied included the prevalence of mental
health issues, including Post-Traumatic Stress Disorder (PTSD),
stress, depression, anxiety, insomnia, and psychological distress or
severe mental disease in general.
The risk for bias assessment was not conducted in this rapid
review. However, we noticed the key limitations of each article,
and paid close attention when we drew the conclusion. Publication
bias were checked by Begg’s rank method and funnel plot using R
version 3.6.1. P-value>0.05 indicates no significant publication bias
[16].
Random effect method heterogeneity test was analyzed to
estimate the research with the prevalence of each of the psychiatric
symptom in health professionals as study outcomes. The results
showed the existence of heterogeneity among the articles being
chosen. The probable factors may be due to geographic variation
and therefore a subgroup analysis was performed.
Result
Most of the studies were cross-sectional except for one article from Mei et al. [17], which was a case-control study. Of the final 26 studies, 3 studies had interpreted the prevalence of post-traumatic stress disorder (PTSD) among medical workers; 9 studies depicted the prevalence of stress in health professionals; 18 studies presented the prevalence of depression status in medical workers; 21 studies investigated the prevalence of anxiety among medical staff; 7 studies have showed the prevalence of insomnia in medical staff; and 4 studies demonstrated the prevalence of psychological distress or severe mental disease in medical staff.
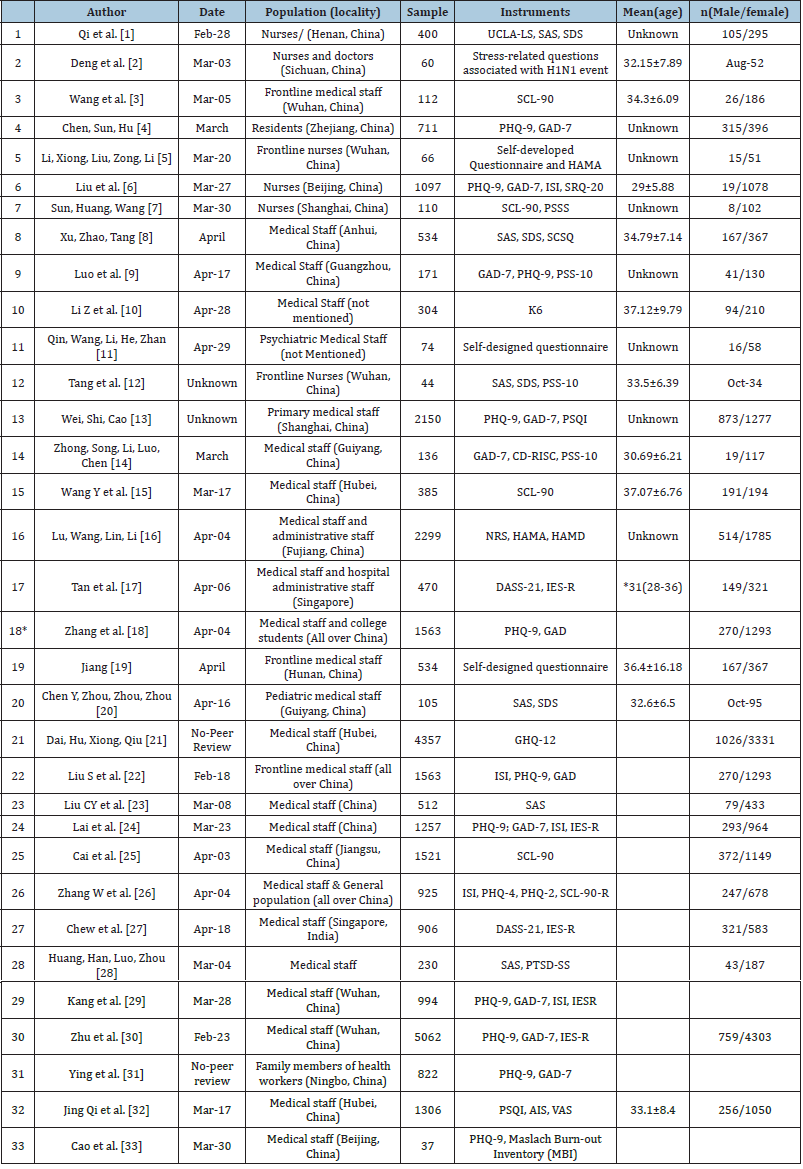
Table 1:Summary of Studies Included in the Review.
The overall prevalence of mental health issues by symptoms
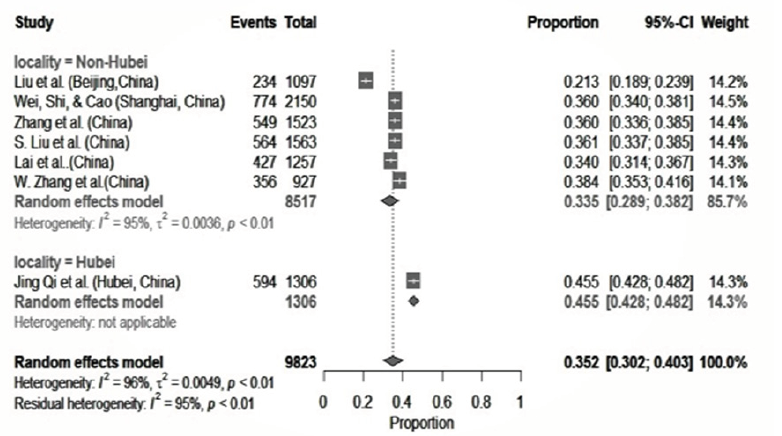
After the meta-analysis was done the prevalence of Post- Traumatic Stress Disorder (PTSD) was 12.8% (95% CI: 0.048- 0.238), stress was 36.3% (95% CI: 0.176-0.573), (Figure 2) depression was 29.4% (95% CI: 0.211-0.385), (Figure 3) anxiety was 30.5% (95% CI: 0.253-0.358), (Figure 4) insomnia or sleep disturbance was 35.2% (95% CI: 0.302-0.403), (Figure 5) and psychological distress or severe mental health was 19.1% (95%CI: 0.065-0.3622).
Figure 2:Meta-analysis on stress among health care professionals during COVID-19.
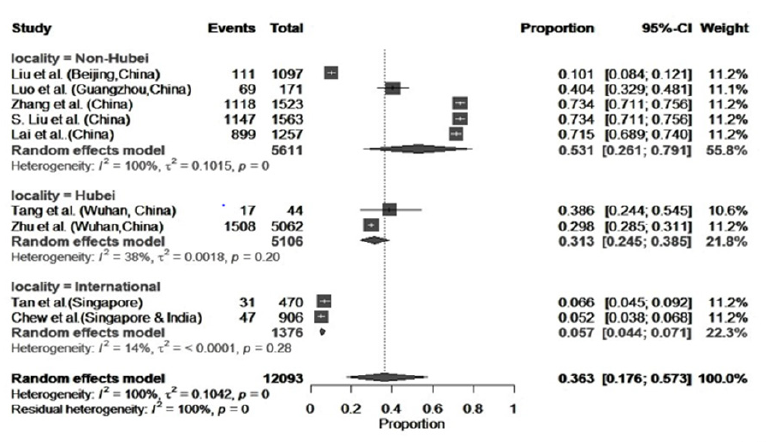
Subgroup analysis and sensitivity analysis
A subgroup analysis was done to determine the heterogeneity among the studies, and whether they were comparable. Figure 2 shows the subgroup analysis of stress of three geographic categories: Hubei; other provinces in China and outside China, the I2 statistic indicated that the percentage of variation across was due to heterogeneity rather than by chance [18]. Meta-analysis on the prevalence of stress among health professionals, from two studies from Hubei province indicated homogeneity [19,20]. The prevalence of stress among health professionals in Hubei province was 31.3% (95% CI: 0.245=0.386) and prevalence in other provinces in China the was much higher (53.07%, 95% CI: 0.261-0.792). Similarly, the prevalence of depression reported on health professionals in other provinces of China was 34.0%, (95% CI: 0.244-0.443), and this was higher than in Hubei which was 25.20%, (95% CI: 0.134-0.388), The prevalence of anxiety among health workers in Hubei province was: 28.5%, (95% CI: 0.221- 0.354) and this was higher than in other provinces 33.0%. (95% CI: 0.268-0.395. The prevalence of insomnia among medical workers was higher in Hubei province compared to other provinces, 45.5% and 33.5% respectively (Figure 5). Health professionals with psychological distress or severe mental health issues were reported higher in Hubei province (24.5%) compared with other provinces in China (14.1%).
Discussion
The most common mental health problems during this COVID-19 pandemic in Hubei province in China were insomnia (45.5%), stress (31.3%) and anxiety (28.5%). However, in other parts of China insomnia was lower (33.5%), stress and anxiety were higher (53.0%) and (33%) respectively. The prevalence of stress in Hubei province was consistent with SARS pandemic in 2003 which was 35% among doctors and 25% among nurses [21]. The prevalence of stress, depression and anxiety were lower in Hubei Province compared to other provinces in China, and this heterogeneity may be due to geographic variation rather than occupational variation. It could be explained ‘Psychological Typhoon Eye Effect’ [22], that people in the epicentre seem to be more calm and have less post-traumatic concern about their safety and health, compared to other parts of the country. Similar results was also found on the psychological status during the SARS outbreak in 2003 [23]. Although our study focussed on health professionals, the results of our study are consistent with a study among different populations in China during COVID-19 outbreak [24].
Figure 3:Meta-analysis on depression among health care professionals during COVID-19.
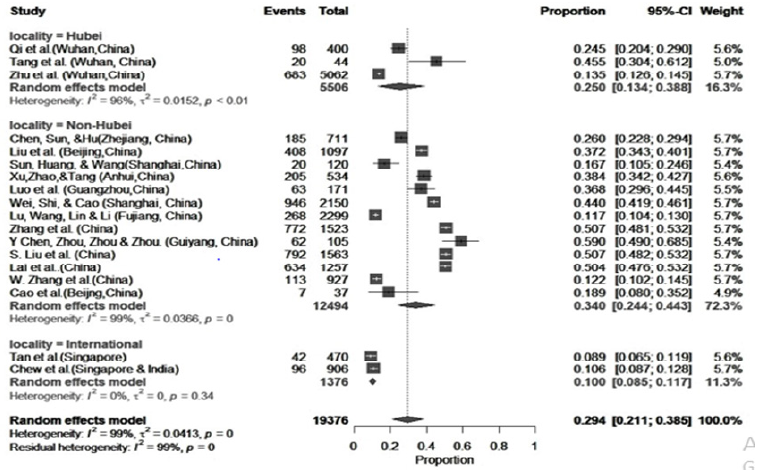
Figure 4:Meta-analysis on anxiety among health care professionals during COVID-19.
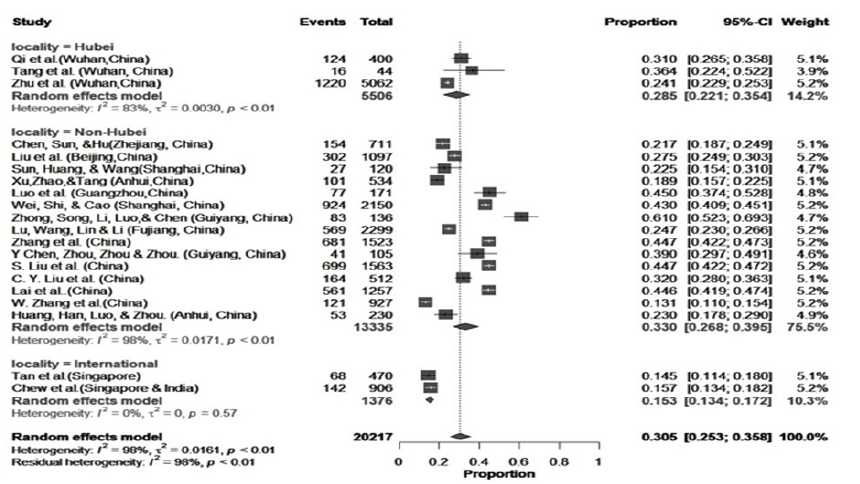
Figure 5:Meta-analysis on insomnia among health care professionals during COVID-19.
Our meta-analysis failed to achieve I2 <50%, and this could be due to the geographic variations, age or gender structure of the study population, and the instruments or the questionnaire being used. Other studies in China had also revealed that female and young adult group were more susceptible to mental health issues [25,26]. However, studies in Italy and Nigeria [27,28], did not find any evidence on mental health of health professional by gender and age groups. Mental health issues among the health professionals and in the community is a worrying concern since the number of COVID-19 is still increasing. In many countries. We need to be prepared to address these issues and take necessary steps in the prevention of these issues [29].
Conclusion
This limited meta-analysis shows that there is high prevalence of mental health issues in the areas affected by COVID=19. It is important that we address the mental health issues early and there is an urgent need to implement mental health interventions identified in the countries affected by COVID-19.
Limitations
Online self-reporting survey was commonly used by the reviewed scholars and this may introduce information and selection bias. Besides, some of the articles had small sample size (n<200) and this may affect the effect size of our analysis.
References
- WHO (2020) Mental health and psychosocial considerations during the COVID-19 outbreak 2020.
- (2020) Control CD and Prevention, Coronavirus disease 2019 (COVID-19) situation summary.
- Wu Z, Googan JM (2020) Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese center for disease control and prevention. JAMA 323(13): 1239-1242.
- Chou R (2020) Epidemiology of and risk factors for coronavirus infection in health care workers: A living rapid review. Annals of Internal Medicine 172(2): 120-136.
- Lung FW (2009) Mental symptoms in different health professionals during the sars attack: a follow-up study. Psychiatr Q 80(2): 107-116.
- Lee SM (2018) Psychological impact of the 2015 MERS outbreak on hospital workers and quarantined hemodialysis patients. Compr Psychiatry 87: 123-127.
- Shaker MS (2020) COVID-19: pandemic contingency planning for the allergy and immunology clinic. J Allergy Clin Immunol Pract 8(5): 1477-1488.
- Cai W (2020) A cross-sectional study on mental health among health care workers during the outbreak of Corona virus disease 2019. Asian J Psychiatr 51: 102111.
- Cao J (2020) A study of basic needs and psychological wellbeing of medical workers in the fever clinic of a tertiary general hospital in Beijing during the COVID-19 outbreak. Psychother Psychosom 89(4): 252-254.
- Chen YJ, Hu J (2020) Analysis of mental health status of residents during COVID-19 epidemic. Clinical Education of General Practice.
- Chew NW (2020) A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav Immun 88: 559-565.
- Maher A (2020) COVID-19 outbreak situation and its psychological impact among surgeon in training in France. World J Urol 23: 1-2.
- Tan BY (2020) Psychological impact of the covid-19 pandemic on health care workers in singapore. Ann Intern Med 173(4): 317-320.
- Haby MM (2016) What are the best methodologies for rapid reviews of the research evidence for evidence-informed decision making in health policy and practice: a rapid review. Health Res Policy Syst 14(1): 83.
- Elliott JH (2017) Living systematic review: introduction-the why, what, when, and how. J Clin Epidemiol 91: 23-30.
- Begg CB (1994) The handbook of research synthesis. 25: 299-409.
- MEI J (2020) Analysis of psychological and sleep state of medical stuff with novel coronavirus pneumonia. Herald of Medicine 39(3): 345-349.
- Jones HE (2019) Quantifying how diagnostic test accuracy depends on threshold in a meta-analysis. Stat Med 38(24): 4789-4803.
- Tang H (2020) Investigation and analysis on mental health status of frontline nurses in wuhan during covid-19 epidemic. International Infections Diseases.
- Zhu Z, Yebin, Guo, Miao, Wang, et al. (2020) COVID-19 in Wuhan: immediate psychological impact on 5062 health workers. MedRxiv.
- Chan AO, Huak CY (2004) Psychological impact of the 2003 severe acute respiratory syndrome outbreak on health care workers in a medium size regional general hospital in Singapore. Occupational Medicine 54(3): 190-196.
- Li S (2009) Psychological typhoon eye in the 2008 wenchuan earthquake. PloS one 4(3): e4964.
- Xie XF, Eric, Zheng, Zhang (2011) The ‘typhoon eye effect’: determinants of distress during the SARS epidemic. Journal of Risk Research 14(9): 1091-1107.
- Li W (2020) Psychological status among different populations during COVID-19 epidemic: a systematic review and meta-analysis. Journal of Tongji University, China.
- Qiu J, Shen, Wang, Bin, Xu (2020) A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatr 33(2): e100213.
- Liu N, Zhang, Wei, Sun, Wu, et al. (2020) Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: Gender differences matter. Psychiatry Res 287: 112921.
- Simione L, Gnagnarella C (2020) Differences between health workers and general population in risk perception, behaviors, and psychological distress related to COVID-19 spread in Italy. Front Psychol 11:2166.
- Olaseni AO, Abayomi OO, Samson, Rotimi (2020) Psychological distress experiences of nigerians amid covid-19 pandemic. SSRN.
- Duan L, Zhu G (2020) Psychological interventions for people affected by the COVID-19 epidemic. Lancet Psychiatry 7(4): 300-302.
© 2020 Xiong CL. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






