- Submissions

Full Text
COJ Nursing & Healthcare
Examining the 2:1 Model of Fieldwork for Occupational and Physical Therapy Students
Kate Barlow¹*, Victoria Lehr¹, Diana Kenney² and Michael Salemi³
¹Division of Occupational Therapy, USA
²Division of Physical Therapy, USA
³Department of Occupational Therapy, USA
*Corresponding author: Kate Barlow, Division of Occupational Therapy, Springfield, MA 01109, USA
Submission: August 28, 2020;Published: September 18 2020

ISSN: 2577-2007Volume6 Issue5
Abstract
The COVID-19 pandemic has disrupted clinical placements, not just in the United States, but globally. A Call to Action is proposed to consider the 2:1 model of fieldwork as a viable solution to combat the potential fieldwork crisis that is looming on the horizon. The 2:1 model pairs two students for each fieldwork educator. Although the efficacy of this model has already been proven through prior research, a standardized framework is lacking for implementing the use of the 2:1 model. The aim of this study was to explore the perceptions of fieldwork educators and students on the successful factors of the 2 to 1 model in clinical education. A survey study was completed with occupational and physical therapy students (N=10) who participated in the 2:1 model of fieldwork. Results showed the students perceived the 2:1 model to be an effective model of clinical supervision. Communication, not individual time spent with the student, was what students reported as the most important factor to the effectiveness of the model. Limitations of the study include a small sample size and lack of validation of the survey tool. Future research on the perspectives of the fieldwork educators is recommended.
Keywords: Clinical instructor; Clinical supervision; Clinical placements; Fieldwork; Models of fieldwork
Examining the 2:1 Model of Fieldwork for Occupational and Physical Therapy Students
The current COVID-19 pandemic has disrupted the fieldwork placements, not just in the United States, but globally (Table 1). For the field of occupational and physical therapy to recover from this disaster, a Call to Action is proposed. The 2:1 model of fieldwork implies that each fieldwork educator (FWE) supervises 2 students. Implementing the 2:1 model of fieldwork is one of the ways in which practicing clinicians can be a part of the solution to this crisis.
Currently in the fields of occupational therapy (OT) and physical therapy (PT)/physiotherapy, students must complete fieldwork or clinical education placements to demonstrate core competencies of their hands-on clinical skills to be eligible for licensure [1]. Several factors are impeding the clinical development of future therapists. The growth of OT and PT programs has led to an increasing shortage of clinical education sites available for students [2]. In addition, the COVID-19 pandemic restrictions have further delayed the ability for students to complete their clinical requirements. Several alternative supervisory practice models have been developed to try and increase the student placements. Most of these alternative approaches consist of peer or collaborative learning, such as the 2:1 model, which consists of 2 students to 1 FWE/clinical instructor (CI). In OT, the therapist who provides supervision is referred to as a FWE. In PT, the supervisor is referred to as a CI; these terms will be used interchangeably in this report.
Table 1: Global Occupational Therapy Perspectives on the COVID-19 Pandemic.
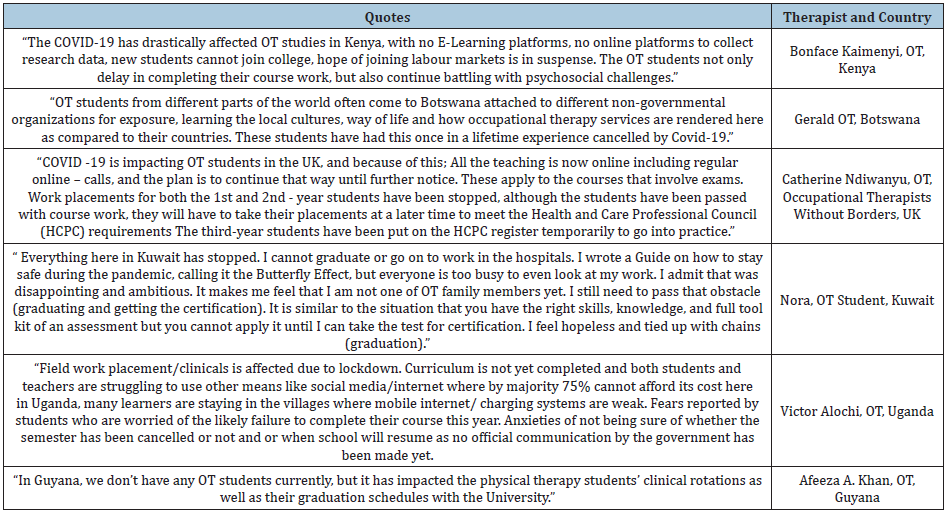
Note: Quotes are from personal communication with the first author (Kate Barlow) in April 2020. Kate Barlow is the founder and host of an international mentorship program. All of the therapists who provided quotes are members of the mentorship program and gave permission for their quotes to be published.
Table 1
The benefits of the 2:1 placement model include improved student-educator relationships, increased student observation skills, collaboration skills, independence, and increased opportunities for students to give and receive feedback [3,4]. A systematic review by Sevenhuysen et al. [5] assessed 28 articles across 5 allied health professions, including OT, PT, speech language therapy, nutrition and dietetics, and social work. The conclusion of the review is that clinical placement models with multiple students and one FWE accommodates the growing number of healthcare students that can be placed in a clinical setting [5]. Additional research has been conducted to look at the 2:1 model of clinical education’s impact on competency, productivity and time utilized in practice.
Clinical competency scores were compared for 95 students who participated in either 1:1 or 2:1 clinical placements and graduated from a western Canadian entry-level OT program [6]. This study found the clinical competence of students were comparable for both models of fieldwork; the results of the Competency Based Fieldwork Evaluation for Occupational Therapists (CBFE-OT) tool demonstrated no statistical difference between those students who participated in 1:1 and 2:1 placements [6].
FWE productivity was investigated in an acute care hospital in Orlando, Florida and results showed FWE productivity increased while supervising in both the 1:1 and 2:1 models [7]. Further, the study found FWE productivity reached over 125% when going from the 1:1 to 2:1 model [7]. Researchers in Australia found no statistical significance with use of 1:1 or 2:1 models when examining time-use of both speech and language therapy CIs and students [8]. The results of these studies suggest a 2:1 placement model can increase the quantity of placements without negatively impacting quality of CI performance or student competence.
The biggest challenges that FWEs perceived with the 2:1 model of clinical placement was their negative perceptions prior to engaging in the 2:1 model and their inexperience and knowledge to effectively conduct a 2:1 model of clinical education [9]. Sevenhuysen et al. [5] revealed a lack of a standardized framework for implementation or tools to accurately measure outcomes of the 2:1 model. Peer assisted learning was inadequately defined due to the lack of a formalized framework [5]. The FWE concerns from an Australia OT program included potential negative impact on patients, their workload, and management of two students [10]. Additional barriers consisted of increased documentation, planning and organization for the CI, comparison of student pairs, and unhealthy competition between students [3,4].
To ensure successful implementation and address the FWE and student challenges, the literature has emphasized the need for education and preparation prior to 2:1 clinical placements [5]. Bhagwat et al. [8] supported the need for FWEs’ and students’ pre-placement education to decrease their concerns and fears associated with the 2:1 model. A study by Alpine et al. [4] found that pre-placement education for both PT CIs and students was the key to success of these multi-student placements in Ireland. The implementation of intentional student pairings according to their academic abilities arranged by the academic programs would prevent unhealthy competition and negative interactions [9]. Price & Whiteside [10] further suggested academic programs be accessible to FWEs to ensure guidance and support throughout the clinical experience. Adequate preparation of FWEs and students to the 2:1 model of clinical placement would increase the quantity of placements without impacting quality or the clinical experience.
In an Australian study, both the OT and PT FWEs and students preferred a 2:1 model. The students preferred the 2:1 model in the beginning of the clinical experience for the collaboration but preferred the 1:1 model toward the end of their clinical rotation [2]. Respiratory therapy students participating in peer learning at University Health Network in Canada began with a 2:1 collaborative model. When they gained independence with their skills and caseloads, they naturally moved to a 1:1 model [11]. Dorner & Colleagues [11] advocated for the need of one-on-one time for each student with the FWE to ensure successful implementation of this clinical model. Lynam et al. [3] emphasized the necessity for built in one-to-one time for each student with the FWE in order to progress their clinical knowledge and skill.
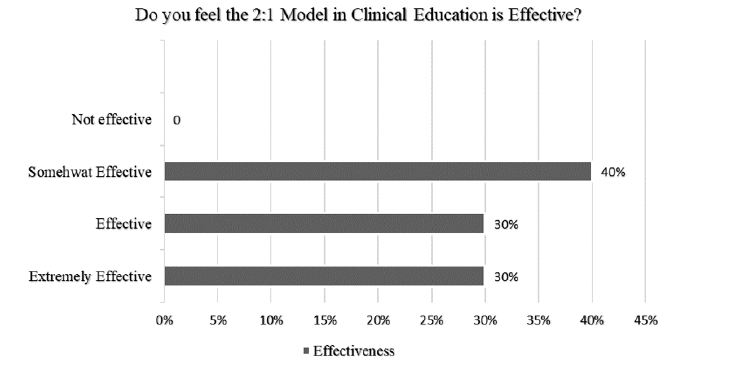
Figure 1: Effectiveness of the 2:1 model of clinical education.
The 2:1 clinical placement model has yet to become a standard practice but has promising evidence to support expanding its use in future clinical education. Research studies from both Lynam et al. [3] and Myers et al. [9] of collaborative learning utilized peer observation and feedback. The toolkit referenced by Myers et al. [9] included preparation strategies and frequent electronic contact with the students, FWEs, and the academic institutions. Both studies revealed the importance and need for FWEs and students to have preparation prior to implementing this model. They also felt the importance of a close partnership between FWEs and academic institutions. There is still currently no standardized framework that is widely used or accepted for implementing and measuring the use of a 2:1 model. The aim of this study was to explore the perceptions of FWEs and students on the successful factors of the 2 to 1 model in clinical education.
Methods
This study was approved by the college’s Internal Review Board. All students (and their respective FWEs) who were paired with another student at the same level of education, was eligible to participate in the study. The students and FWEs were conveniently sampled, and consent was obtained. The online survey was composed of 11 questions, consisting of open-ended and Likert questions. The two open ended questions on the survey were: “What were the positives to the 2:1 Model?” and “What were the negatives to the 2:1 Model?”.
The survey was developed by two of the authors of the study (XXXXX), both of whom were academic fieldwork coordinators at the time of the study. The OT students were third year master’s level students on their Level II fieldwork. The PT students were first, second and third-year doctoral students on a 12-week clinical internship.
Result
A total of ten OT and PT students completed the survey. No FWE surveys were returned. Students who completed the survey consisted of five OT students and five PT students (four PT students in their third year of the program and one student in their first year of the program). Students were placed in a variety of settings including outpatient, skilled nursing, pediatrics, sports and mental health. All ten students reported the 2:1 model to be an effective model of clinical supervision, ranging from somewhat effective to extremely effective (Figure 1). The students rated that communication was the number one personal characteristic of the FWE that made the 2:1 model successful. Additional factors, in their perspective order, that made the 2:1 model successful were the FWE’s ability to deliver effective feedback, teaching ability and time management skills.
Figure 1
When looking at factors that facilitate success of the 2:1 model of supervision, students ranked the following as extremely important: the years of experience of the supervising therapist, organization, and structured learning opportunities. The amount of individual time the FWE spent with the student did not correlate with the effectiveness of the 2:1 model or whether the student would try the 2:1 model when they become a FWE.
The students also reported on productivity and 60% of the students felt that their FWEs’ productivity increased and 20% felt productivity evened out over time. There were three students who completed their fieldwork in a mental health setting and all three students had a different opinion on productivity. One student felt that productivity was not impacted and another student felt that productivity decreased. The third student completing a level II fieldwork experience in a mental health setting reported that the productivity increased.
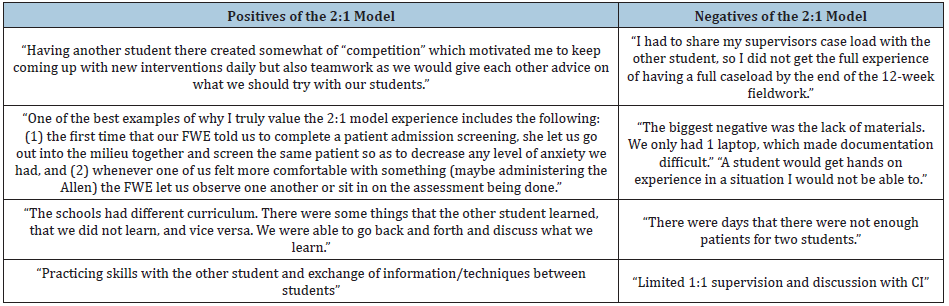
The main positive theme was the collegial support given by the paired students. The negatives of the model reported were the lack of individual time spent with the clinical instructor, lack of materials and the reduction of patients (Table 2).
Table 2: Student Feedback on the 2:1 Model.
Discussion
This pilot study, although a small sample size, provided important information for academic fieldwork coordinators to ponder if considering the 2:1 model. For this study, the academic fieldwork coordinators did not arrange the 2:1 model with the fieldwork site. Instead, the 2:1 model was determined by the clinical site; therefore, the OT and PT students paired were not both from the same institution. If the academic fieldwork coordinators are going to request the 2:1 model to pair two OT or two PT students together to help recover from the COVID-19 pandemic, pairing two students of matching ability is recommended. Although the students in this study all reported the 2:1 model to be effective, it is important to know what makes the 2:1 model successful.
From these preliminary findings, communication, not individual time spent with the student, was what students perceived as the most important factor to the effectiveness of using the 2:1 model. When deciding whether the 2:1 model is a good fit for a clinical site, factors to consider would be the FWE’s years of experience, the ability to deliver effective feedback and time management skills.
The type of setting and the amount of individual time spent with a student did not appear to be factors which predict success using the 2:1 model. Although the 2:1 model of supervision may be a necessary consideration for the sustainability of the OT and PT clinical education requirements, careful selection of FWEs who are organized and experienced may be crucial to the model’s success.
FWEs considering the 2:1 model would benefit from academic programs providing training on organizational strategies and how to conduct structured learning opportunities with two students. Future studies on the outcomes of FWE training may have a powerful impact on the 2:1 model’s success. The limitations of this study include the small sample size, the lack of reliability and validity of the survey and the lack of FWE insight and perceptions of the model.
Conclusion
In the wake of the COVID-19 pandemic, OTs and PTs that serve the profession as FWEs should consider implementing the 2:1 model of supervision across all practice areas. The vast network of rehabilitation stakeholders, including professional organization leaders, program directors, FWEs, academic fieldwork coordinators and therapy students, can all recognize that the current system that supports OT and PT clinical rotations was experiencing a strain prior to the current global pandemic. Now, with so many therapy students being notified that their clinical placements have been cancelled in the wake of government shutdown and practice setting restrictions, the stress on the fieldwork system has intensified significantly. Implementation of the 2:1 model of fieldwork will effectively double the capacity of therapy students that FWEs can accommodate. Utilization of this fieldwork model in clinical rotations, starting once practice settings reopen to students, will provide a viable solution to combat the potential fieldwork crisis that is looming on the horizon.
References
- Brown T (2013) Relationships between clinical fieldwork, educator performance and health professional students’ perspectives of their practice learning environments. Nursing and Health Sciences 15(4): 510-517.
- O Connor A, Cahill M, McKay E (2012) Revisiting 1:1 and 2:1 clinical placement models: Student and clinical educators perspectives. Australian Occupational Therapy Journal 59(4): 276-283.
- Lynam A, Corish C, Connolly D (2015) Development of a framework to facilitate a collaborative peer learning 2:1 model of practice placement education. Nutrition & Dietetics 72(2): 170-175.
- Alpine LM, Caldas FT, Barrett EM (2019) Evaluation of a 2 to 1 peer placement supervision model by physiotherapy students and their educators. Physiotherapy Theory and Practice 35(8): 748-755.
- Sevenhuysen S, Thorpe J, Molloy E, Keating J, Haines T (2017) Peer-assisted learning in education of allied health professional students in the clinical setting: A Systematic Review. Journal of Allied Health 46(1): 26-35.
- Short M, Lethman AC, Currie L, Drynan DP (2017) Comparing occupational therapy students’ competency scores: 2:1 versus 1:1 fieldwork. International Journal of Practice-based Learning in Health and Social Care 5(1): 1-11.
- Pabian PS, Dyson J, Levine C (2017) Physical therapist productivity using a collaborative clinical education model within an acute care setting: A longitudinal study. Journal of Physical Therapy Education 31(2): 11-17.
- Bhagwat M, Hewetson R, Jones L, Hill A, Nunn J, et al. (2018) Comparison of paired and single clinical placement models: A time-use analysis. International Journal of Language and Communication Disorders 53(3): 468-479.
- Myers K, Davis A, Thomas S, Bilyeu C (2019) Clinical instructor perceptions of the collaborative clinical education model: Providing solutions for success in physical therapy education. The Internet Journal of Allied Health Sciences and Practice 17(4): 1-9.
- Price D, Whiteside M (2016) Implementing the 2:1 model in occupational therapy: Strategies for practice. Australian Occupational Therapy Journal 63(2): 123-129.
- Dorner S, Fowler T, Montano M, Janisse R, Lowe M, et al. (2019) Implementing a peer-learning approach for the clinical education of respiratory therapy students. Canadian Journal of Respiratory Therapy 55: 21-27.
© 2020 Kate Barlow. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






