- Submissions

Full Text
COJ Nursing & Healthcare
Effect of a 2-Day Hospital Wide Communication Skills Training on Self-Ratings of Nursing Staff
Sobia Ali1*, Zohra Jawed2, Mehnaz Umair3, Anwer Ali Khan4, and Anushah Mirza5
1,3 Department of Health Professions Education, Liaquat National Hospital and Medical College, Pakistan
2,4 Nursing Education Services, Liaquat National Hospital and Medical College, Pakistan
5 3rd year Neuroscience student at University of Texas at Dallas, USA
*Corresponding author: Sobia Ali, Associate Professor, Department of Health Professions Education, Liaquat National Hospital and Medical Collage, Stadium Road Karachi, Karachi, Pakistan
Submission: May 15, 2020;Published: June 29, 2020

ISSN: 2577-2007Volume6 Issue3
Abstract
Introduction: Being the forefront of health care, nurses play a vital role in health promotion and maintenance. Apart from context specific knowledge and skills, nurses are required to have non cognitive soft skills for better health provision.
Objective: To assess the change in participants’ self-rating on communication skills scale before training and 3 months post-training follow up.
Methods: The study participants comprised of all nurses who were employed at Liaquat National Hospital (LNH). 42 Sessions were conducted for 722 nursing staff of LNH between 15th May 2018 to 18th July 2019. This 6-hour course mainly focussed on highlighting the importance of basic concepts of effective communication related to nursing practice. Nurses were asked to fill the communication scale created by Susan Barkman and Krisanna Machtmes (Perdue University). Before the start of each workshop, participants were asked to self-rate their communication on this scale. This self-rating was again done after 3 months of training as a follow up.
Result: Nurses’ pre and post self-rating on various components of communication skills shows a statistically significant change in their responses (follow up training ratings minus before training ratings). 21 out of 23 (91%) of our items showed statistically significant change (p<0.05) in nurses’ ratings except for item numbers 3 and 23 that showed non-significant results (p>0.05).
Conclusion: Present study discussed the development and implementation of a six hour hospital wide CSTC for nurses in a tertiary care settings. Follow-up self-ratings on communication scales after three months of training showed significant improvement on various aspects of communication skills.
Keywords: Communication, Nursing, Education, Training programs, Program evaluation/ methods, Self-efficacy/ratings
Abbreviation: CSTC: Communication Skills Training Course
Introduction
Being the forefront of health care, nurses play a vital role in health promotion and maintenance. Apart from context specific knowledge and skills, nurses are required to have non cognitive soft skills for better health provision. Communication, for example, helps to create an effective relationship during the course of a treatment [1]. The need for effective nursing communication becomes very apparent when it is observed that ineffective communication leads to increased medical errors, difficulty in achieving nursing tasks, greater patient distress, and decreased quality of health care [1-4]. Therefore, establishing effective communication is considered as an essential expertise in the nursing practice [5].
Accreditation bodies, both national and international, emphasize attempts to strengthen communication between patients and health professionals [6,7]. Thus communication skills are considered an important part of basic training during nursing school as well as after graduation [8,9]. Evidence suggests that communication can be improved through training and that short interventions are essential in enhancing these skills [10,11]. However, ensuring sufficient training of nurses, in positive communication with patients and/or families, is challenging. To address this task, a variety of interventions have been developed in the form of courses and workshops using role plays and simulated training as instructional strategies [12-15]. Workshops are the most common intervention for developing skills in any context. Methods for assessing the usefulness of workshops are numerous.
Those include: a retrospective pre-post design, a pre-test followed by a post-test soon after the training phase, and a pre-test followed by a post-test after the actual experience. Literature indicates the varying efficacy of these approaches [16-18]. Presuming that participant’s perceptions/ratings after actual performance would reflect the real picture of training outcome, we designed this study in which we asked the participants to rate themselves on various aspects of communication before the training and after 3 months of training. This way we could assess the difference in their rating that would in turn help measure the effectiveness of communication skills training. We also found that data primarily emphasizes on the quality of communication skills training for nurses on specific groups such as palliative care nursing, oncology nursing or primary care nursing. Limited data is available for assessing the effectiveness of a tertiary care hospital wide communication skill targeted at practicing nurses across various specialities and working sites [19]. This leads to the rationale behind this study with the objective to assess the change in participants’ self-rating on communication skills scale before training and 3 months post-training follow up.
Material and Method
Participants
The study participants comprised of all nurses who were employed at Liaquat National Hospital (LNH). 42 Sessions were conducted for 722 nursing staff of LNH between 15th May 2018 to 18th July 2019. Eligible participants for our study include all nursing staff who receives the training and continue to work after three months of training for follow up self-rating. 86 participants left the job leaving 636 meets the eligibility criteria for this study (Table 1).
Table 1:

Intervention outline
Communication skills training course (CSTC) is an initiative of Liaquat National Hospital under ambit of Nursing Education Services with the aim to enhance patient satisfaction through effective nursing communication. The 6-hour course was designed to be covered in two days i.e. 3-hour session each day. This training session was mainly focussed on highlighting the importance of basic concepts of effective communication related to nursing practice. On Day-1, non- verbal and para-verbal communications along with active listening were discussed and practiced. Day-2, mainly focussed on verbal communication in terms of dealing with aggressive patients and/or families, empathetic communication, and understanding when to limit communicating. Guidelines, schedule and handouts were provided for each session and included a brief didactic theory based overview followed by discussion, video reviews and skills practice using role plays. Active listening exercises were also done during the sessions.
Trainers training
Volunteer participation from selected faculty and staff for training a bulk of nurses serving at LNH was decided. The working team proposed a group of trainers from nursing school faculty and nursing services, basic and clinical sciences faculty, members from Department of Health Professions Education and Department of physiotherapy. These trainers were trained in a separate workshop before the formal launce of the course to develop a pool of trainers. A manual with details of every session was developed also to ensure uniformed facilitation throughout the training period. The working group contributed to the development of the manual.
Data collection
Communication scale developed by Susan Barkman and Krisanna Machtmes (Perdue University) 20 was chosen and used for the study because it matches with our needs and content that was taught in our course. Before the start of each workshop, participants were asked to self-rate their communication on this scale. This self-rating was again done after 3 months of training as a follow up. 23 items scale consists of close ended question with components of basic communication. Participant were asked to rate themselves on 5 point scale of 0-4, where 0=Never, 1=Rarely, 2=Sometimes, 3=Often, 4=Always. To cross-check the validity of responses, two questions were of reverse scoring.
Data analysis
Data was analysed by SPSS version 20. Descriptive statistics about, gender, age, department from which they belong and the year of experience were computed. 2 items were scored in reverse (i.e 0 was considered as 4, 1 was considered as 3 and 2 remain the same). Cronbach’s alpha was calculated for claiming the internal consistency of questionnaire. Wilcoxon signed rank test (two tailed) was used for comparison of paired data (pre-training and post training follow-up). This non parametric test was used because of skewed data.
Result
A total of 636 nursing staff were available for follow up ratings after getting trained in CSTC, of whom 534 (83.96%) filled both pre-training and follow up post-training questionnaires after 3 months. Out of them, 325 (60.8%) were male and 209 (39.2%) were females. Among all the departments, the response was relatively higher from Medicine and allied departments (36.2%).
Table 2: Comparison of pre-workshop and post-workshop follow up ratings of nurses.
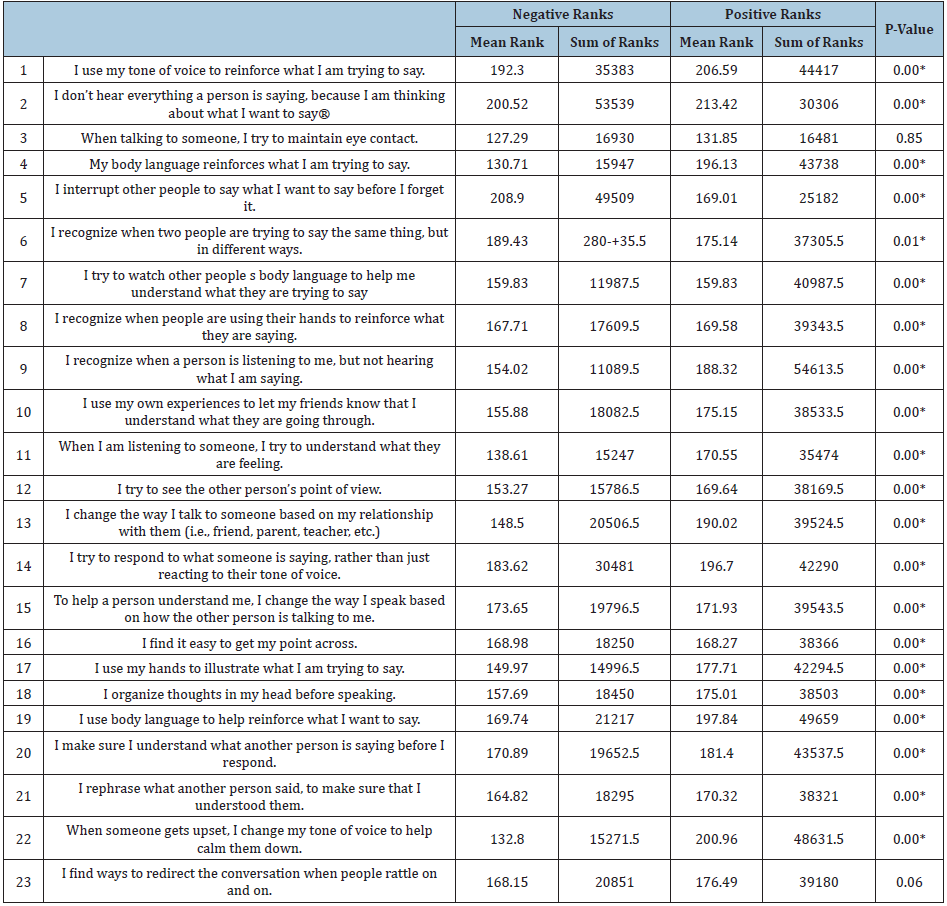
To verify the internal consistency of the scale of all items, we calculated Cronbach’s alpha for the two groups, which was 0.735 for pre-course and 0.797 for post-course follow up. Nurses’ pre and post self-rating on various components of communication skills shows a statistically significant change in their responses (follow up training ratings minus before training ratings (Table 2). 21 out of 23 (91%) of our items showed statistically significant change (p<0.05) in nurses’ ratings except for item numbers 3 and 23 that showed non-significant results (p>0.05). These items were about maintaining eye contact and knowing the ways to redirect the conversation when someone tried to prolong it. In addition, the trend of higher ratings in post-course follow up is prominent in all items except for these two mentioned already.
Discussion
This study demonstrated the development and implementation of a rigorous communication skills training program for nurses situated at a tertiary care hospital. Providing a communication skills training curriculum that discusses the related communication difficulties faced by nurses, illustrated the organization’s dedication to promote and facilitate the engagement of nurses with patients, families, colleagues and physicians [20].
Based on our findings, after training in communication skills, there is a substantial increase in self-assessment of different aspects of communication skills. Participants who had a threemonth follow-up period showed significantly increased ratings in the use of communication skills. By comparing pre and post course ratings after three months rather than immediately after training, the comparison in self-rating is more accurate and efficient evidence of the changes associated with this type of training [21- 23]. Justification of selecting this approach for our study is also based on the principles that ratings after actual performance are considered more valid and provide a clearer picture of training outcome [17].
Most of the items in our questionnaire showed significant gain in self rating. These findings matches with evaluation of similar workshops/courses that reported self-assessment improvement in participants’ abilities [5,24]. Since higher self-efficacy is linked to the more effective performance of learned skills, this increase in self-rating will result in a more successful implementation of the skills learned in CSTC.
“When talking to someone, I try to maintain eye contact” was the first statement in the communication scale in which there was no significant difference between the mean ranks of self-rating on two occasions (positive rank minus negative ranks, p>0.05). The reason behind this could be the effect of other confounding variables of our study other than the pre course and post course follow up timings of data collection. The possible justification of this rating may be due to cultural and social context of the participants [24].
Another item that showed non-significant change in self rating was “I find ways to redirect the conversation when people rattle on and on”. This is an interesting finding that participants find it difficult to redirect the conversation that in turn may cause frustration and feelings of wasted time and effort. The obvious reasoning behind this argument is that the objectives of the workshop revolves mainly around the basic communications and did not address the conversational agility which is considered as higher communication [25].
Limitations
The follow up self-rating and hospital wide distribution of participants are the strengths of our study, but it has certain limitations as well. First, the response rate is fairly high from nurses that belong to medicine and allied departments, but lower for others. This may affect the generalizability of the findings to the groups that showed less response. Second, we used the questionnaire, which was not validated in our context. There is ongoing research by the authors on validating the scale by factor analysis. Finally, although CSTC represented a structured approach to teaching communication, training by multiple facilitators is likely to have variation with different groups of learners.
Conclusion
Present study discussed the development and implementation of a six hour hospital wide CSTC for nurses in a tertiary care settings. Follow-up self-ratings on communication scales after three months of training showed significant improvement on various aspect of communication skills. This study also supports the evidence that even a short course, when implemented, can be an efficient way to improve communication self-efficiency. This is principally important from the point of view of busy nursing schedule and hospital resources that hamper the longer multiple days’ courses.
Recommendation
The positive findings of the study encourage the continuation of the course along with demanding evaluation. Further studies are recommended to explore the long term impact of communication skills courses in other health care settings. In addition, there is a need to explore the relationship between the results of self-ratings with the patients’ outcome.
References
- Khodadadi E, Ebrahimi H, Moghaddasian S, Babapour J (2013) The effect of communication skills training on quality of care, self-efficacy, job satisfaction and communication skills rate of nurses in hospitals of Tabriz. Iran Int J Caring Sci 2: 27-37.
- Zimmerman JE, Shortell SM, Rousseau DM (1993) Improving intensive care: Observations based on organizational case studies in nine intensive care units: A prospective, multicenter study. Crit Care Med 21: 1443-1451.
- Thorne SE, Bultz BD, Baile WF (2005) Is there a cost to poor communication in cancer care? a critical review of the literature. J Psychosoc Oncol 14: 875-884.
- Kennedy M, Denise M, Fasolino M, John P, Gullen M, et al. (2014) Improving the patient experience through provider communication skills building. Patient Exp J 1(1): 56-60.
- Brighton LJ, Selman LE, Gough N, Nadicksbernd JJ, Bristowe K, et al. (2018) Difficult Conversations: evaluation of multiprofessional training. BMJ Support Palliat 8(1): 45-48.
- The Joint Commission (2015) Facts about Patient-Centered Communications.
- Curriculum of Bachelors of Science in Nursing (BSN).
- McCabe C (2004) Nurse-patient communication: an exploration of patients' experiences. J Clin Nurs 13(1): 41-49.
- McGilton K, Irwin-Robinson H, Boscart V, Spanjevic L (2006) Communication enhancement: nurse and patient satisfaction outcomes in a complex continuing care facility. J Adv Nurs 54(1): 35-44.
- Boscart VM (2009) A communication intervention for nursing staff in chronic care. J Adv Nurs 65: 1823-1832.
- Happ MB, Garrett KL, Tate JA (2014) Effect of a multi-level intervention on nurse-patient communication in the intensive care unit: results of the SPEACS trial. Heart Lung Circ 43(2): 89-98.
- Saslaw M, Sirota DR, Jones DP, Rosenbaum M, Kaplan S (2017) Effects of a hospital-wide physician communication skills training workshop on self-efficacy, attitudes and behavior. Patient Exp J 4(3): 48-54.
- Dalcól C, Garanhani ML, Fonseca LF, Carvalho BG (2018) Communication skills and teaching-learning strategies: perception of nursing students. Cogitare Enferm 23(3): e53743.
- Alhassan M (2019) Effect of a 2-day communication skills training on nursing and midwifery students’ empathy: a randomised controlled trial. BMJ 9(3): e023666.
- O'Hagan S, Manias E, Elder C, Pill J, Woodward‐Kron R, et al. (2014) What counts as effective communication in nursing? Evidence from nurse educators' and clinicians' feedback on nurse interactions with simulated patients. J Adv Nurs 70(6): 1344-1355.
- Bhanji F, Gottesman R, De Grave W, Steinert Y, Winer LR (2012) The retrospective pre-post: A practical method to evaluate learning from an educational program. Acad Emerg Med 19: 189-194.
- O’Sullivan PS, Irby DM (2011) Reframing research on faculty development. Acad Med 86: 421-428.
- Ali S, Shoaib H, Rehman R (2016) Exploring the usefulness of interviewers’ training before and after Multiple Mini Interviews (MMI) for undergraduate medical students’ selection: Was it really helpful? Pak J Med Sci 32(6): 1459-1463.
- Barth J, Lannen P (2011) Efficacy of communication skills training courses in oncology: a systematic review and meta-analysis. Ann Oncol 22(5): 1030-1040.
- Barkman SJ, Machtmes KL (2002) Designing quantitative instruments. West Lafayette, Purdue University, Indiana.
- Johansson J, Skeff K, Stratos G (2009) Clinical teaching improvement: The transportability of the Stanford Faculty Development Program. Med Teach 31: e377-e382.
- Leslie K, Baker L, Egan Lee E, Esdaile M, Reeves S (2013) Advancing Faculty Development in Medical Education: A Systematic Review. Acad Med 88: 1038-1045.
- Plack MM, Goldman EF, Wesner M, Manikoth N, Haywood Y (2015) How learning transfers: A study of how graduates of a faculty education fellowship influenced the behaviours and practices of their peers and organizations. Acad Med 90: 372-378.
- Khodadi E, Ebrahimi H, Moghaddasian S, Babapour J (2013) The effect of Communication skills training on quality of care, self-efficacy, job satisfaction communication scale rate of nurses in hospital of Tabriz Iran. Int J Caring Sci 2(1): 27-37.
- Mahajan R (2015) The key role of communication skills in the life of professionals. IOSR-JHSS 20: 36-39.
© 2020 Sobia Ali. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






