- Submissions

Full Text
COJ Nursing & Healthcare
The Experience of Beginning Hemodialysis Treatment and Adjusting to Lifestyle Changes
Lissete González Oquendo*, Candela Bonill de las Nieves and José Miguel Morales Asencio
Department of Health Services, Spain
*Corresponding author: Lissete González Oquendo, Abadiño. CP: 48220 Vizcaya, País Vasco, Spain
Submission: May 08, 2020;Published: June 12, 2020

ISSN: 2577-2007Volume6 Issue3
Abstract
Aims and Objectives: General: To understand the experience of beginning hemodialysis treatment and its related adjustments.
Specific: To delve into the experience of beginning hemodialysis, understand patients’ concerns and perceptions about diet and lifestyle changes, comprehend the factors that interfere with adherence, and understand the experience and self-care associated with vascular access and the degree of social acceptance of the disease.
Background: The percentage of patients on hemodialysis who lack dietary adherence is highly variable, ranging from 25% to 86%. This affects morbidity-mortality and involves increased health care costs. Therefore, we studied this phenomenon from a qualitative point of view.
Design: Qualitative phenomenological study.
Methods: Semi-structured interviews of patients who had recently begun hemodialysis at the Fuerteventura general hospital were conducted.
Data analysis was performed using ATLAS Ti 7.0 software, with a focus on phenomenological reduction and inductive coding. And it has followed coreQ checklist to report the findings manuscript.
Result: Three major themes were found: self-care, kidney disease and replacement therapy, and relationships with the environment.
It was observed that patients who perceived greater support from their families had a higher level of adherence. Still, they experienced greater difficulty in adhering to the restrictions on liquid consumption than to following the dietary recommendations.
Conclusion: The experience of living with hemodialysis has a progressive character that ends in adjustment and acceptance. Kidney transplantation and perceived support act as facilitators of adherence.
Relevance to clinical practice: Patients develop mutually supportive relationships that facilitate their adjustment to lifestyle changes. Relationships with professionals are trusting, although patients seek greater closeness with doctors as well as support for making therapeutic decisions.
Keywords: Qualitative research; Emotional adjustment; Treatment adherence and compliance; Renal dialysis; Self-management; Decision making
Appendix 1
Individual interview - semi-structured
Chronic kidney disease
What pathology results in chronic kidney failure?
What does kidney disease mean for you in your daily life?
Hemodialysis
When did they tell you that you should begin hemodialysis treatment?
Why did you choose hemodialysis as a treatment?
What does hemodialysis mean for you in your daily life?
What impact has it had on your life?
How does one experience the hours in a dialysis bed, without moving?
Vascular access
How is your catheter?
How does one live with a catheter? How does it affect your daily life?
When showering, going to the beach, working in the field, with pets…
How is your fistula?
What is fistula puncture like?
How did you experience the first puncture?
Support, social environment
What sort of support do you receive from people close to you in your environment?
How is your relationship with your dialysis companions?
How is your relationship with dialysis personnel?
How do you socialize your disease? How did you tell those around you that you had to go to dialysis?
In a family situation or social event, how does one manage dietary or fluid restrictions? How do you feel in these situations?
Do you avoid going to engagements?
Do you adapt?
If you go, do you skip your diet on these days?
In the event of skipping your diet, how do you feel? (guilty, indifferent because it is a special occasion…)
Mental health
On a psychological level, how do you feel at these times?
What fears do you have?
Knowledge, information received regarding disease, treatment, and diet to follow:
What type of training or information have you been given by health care personnel regarding chronic kidney disease and hemodialysis?
Transplant
When did you receive information about the diet to follow or the recommendations on fluid intake?
Fluid
What do you know about the fluid restrictions you should have?
How does this restriction affect your daily life?
What does this situation mean for you when you must limit your water consumption?
What actions do you take to avoid exceeding your target weight between dialysis sessions?
What things or situations help you not to drink too much?
What things or situations cause you to drink too much?
How do you gauge fluid excess?
What strategies do you use to avoid drinking too much water?
Diet
What knowledge do you have regarding an appropriate diet to follow?
How do you gauge the dietary limitations you should have?
What does dietary limitation mean for your life?
How does dietary restriction affect you, your family, and your social life?
Can you tell me what would motivate you to follow a proper diet?
What things or situations help you to follow your diet?
What things or situations complicate following your diet?
If there is some doubt about what to eat, where do you look for information?
What strategies do you use to reduce potassium in your meals?
Who do you go to for help in adherence to your diet?
What do you feel is important to help people be adherent with diet, to follow the proper diet?
Would you improve something in the procedures followed by professionals with regard to your care, health literacy…?
What else do you feel is important in the experiences you have had during your time on hemodialysis that we have not discussed?
Supplementary File 1
COREQ (Consolidated criteria for Reporting Qualitative research) Checklist. A checklist of items that should be included in reports of qualitative research. You must report the page number in your manuscript where you consider each of the items listed in this checklist. If you have not included this information, either revise your manuscriptaccordingly before submitting or note N/A.
Impact Statement
What does this paper contribute to the wider global clinical community?
- Acceptance and self-care are important for patient adherence.
- Mutual support groups are needed for adjustment to a new lifestyle.
- Participation in decision making regarding treatment improves acceptance of the disease.
- Information decreases anxiety and improves adherence.
Introduction
When patients begin replacement therapy with hemodialysis, they undergo a very significant change in their lives. They must make regular visits to hemodialysis centers or hospitals to receive treatment, take prescribed medications, and modify their diets; furthermore, they must respect and comply with these three aspects of their care because the success of their therapy and their survival depend on it [1,2]. Adherence is a key concept in nursing practice, and its study is important because lack of adherence to therapeutic regimens is a serious public health problem that increases morbidity and mortality [3].
The definition of adherence is ambiguous and problematic because it describes a complex and multidimensional behavior of the patient, it is dynamic, and it may be influenced by many factors. Nursing has developed a complex meaning of the concept of adherence that implies active participation of the patient in treatment choices and in maintaining good relationships between themselves and health care professionals, including concern with their motivation, health beliefs, and habits, to guarantee compliance with the recommended treatment over the long term; in this context, adherence is viewed as a dynamic process that has flexibility with a patient’s situation [4].
Background
Literature
A systematic review conducted by Matteson et al. [5] concluded that the population with chronic kidney disease is a homogenous population with similar characteristics. Although this homogeneity would be expected to facilitate the success of health literacy programs due to the population's characteristics in terms of adherence, heterogeneity with respect to treatment adherence rate was observed, with rates of non-adherence ranging from 25% to 86% [6]. Hence, interest developed in approaching this phenomenon from a qualitative point of view with the objective of understanding the view of the protagonist as opposed to the homogenizing view of health care providers, which may in itself act as a barrier to designing interventions that are personalized and adapted to the characteristics of chronic kidney disease (CKD) patients [2,5,7-9].
With respect to this, qualitative studies aimed at understanding the view of patients receiving hemodialysis treatment appeared in the literature [10-13]. In one study, Smith et al. [13] focused exclusively on management of fluid restrictions without exploring the rest of the lived experiences of a patient on hemodialysis. In another study, Chun-Chih et al. [10] named as a limitation the lack of understanding of the psychosocial needs of participants and how they face their life experiences in hemodialysis. Krespi et al. [12] related the beliefs of their informants to their treatment adherence. Finally, Griva et al. [11] explored the barriers to and facilitators of hemodialysis treatment adherence in their informants.
Despite the existence of these previous studies, in the present study the intention is to understand generally the experience of persons beginning dialysis treatment, encompassing all of the separate parts that have previously been studied; still, it is novel to include persons who have recently begun hemodialysis. In addition, we were interested in delving into the experiences of these patients in light of the news of actually needing to begin hemodialysis treatment, their experiences during the first session, whether any changes occurred after a few weeks of treatment, the worries they had, and their experiences with regard to the management and self-care of vascular access and the social acceptance of the disease. Our intention was to describe the manner in which individuals experience going to the hospital to receive treatment three times a week and dealing with the particular restrictions necessary for patients receiving hemodialysis treatment, such as fluid restriction, dietary changes, and management of vascular access, as well as the social experiences associated with the disease, using as a data source the individuals who have lived this phenomenon and ultimately to arrive at an understanding of this reality as a whole.
This focus allows us to understand, based on the personal point of view of the informant, where the problems that impede adherence are generated form its origin and what factors contribute to changes in adherence or self-care over time on hemodialysis treatment and thus to identify areas of educational intervention that are adequate for the needs of each person. And also allowed us to identify the problems, concerns, and needs of patients beginning hemodialysis treatment and how these shape their life experience of treatment and their adherence to it.
Methods
This qualitative phenomenological study was conducted from July 2015 to July 2016 at the Virgen de la Peña general hospital on the island of Fuerteventura in Puerto del Rosario. The study population consisted of persons who had recently begun to receive hemodialysis treatment at the general hospital of Fuerteventura. We used purposive sampling; the service's supervisor acted as a "Gatekeeper", advising when new patients begin hemodialysis treatment, at which time we had our first contact with the informant in the dialysis room.
In the sampling process, the following selection criteria were used. The inclusion criteria were, men and women ≥18 years of age, recently beginning hemodialysis renal replacement therapy at the General Hospital of Fuerteventura, that is, patients who had been on dialysis for a maximum of three months. Persons whose native language were Spanish or English, and with adequate cognitive and communication capacities, who voluntarily agreed to participate in the study, and signed an informed consent statement.
The exclusion criteria were, persons who did not wish to participate in the study or who did not sign the informed consent statement, and persons with a diagnosis of dementia or cognitive impairment. The sampling process followed the principle of data saturation such that participants were recruited until a point was reached at which new testimonials and analysis no longer increased the degree of information, codes, categories, and topics. Likewise, the principle of maximum diversity was applied by selecting persons with varied profiles with respect to prior morbidity, age, and country of birth.
Data were obtained by means of semi-structured interviews (Appendix 1) after performing three pilot interviews to assure epoché or bracketing. These first three interviews were conducted by open questions about the most important aspects regarding the experience of beginning hemodialysis treatment and the changes involved. The main themes identified in these three interviews helped in structuring the following semi-structured interview script.
First, rapport was established with informants before focusing the conversation directly on the interests of the study. This was done by asking questions such as “How do you feel?” “How is your hemodialysis treatment going?” The answers to these two questions gave us information on the participants’ concerns and helped us learn a little about the informants. The answers and the nonverbal information conveyed to us by the patients were recorded in the field notes. Interviews were conducted by the primary researcher, in the dialysis room during treatment or in the participants' homes, depending on their preference; each interview lasted for approximately 60 minutes. In each interview, topics not included in the script that emerged spontaneously in the discussion with informants were accepted.
ATLAS Ti 7.0 software was used for data analysis. The analysis was conducted with a focus on phenomenological reduction and with an overall focus on inductive coding. The linking of data was completed using reflection, refinement of phenomenological reflection, writing and rewriting and concluded with obtaining a more universal sphere from the particular descriptions of each informant [14]. And it has followed coreQ checklist [15] to report the findings manuscript (Supplementary file 1).
Supplementary File 1. COREQ (Consolidated criteria for REporting Qualitative research) Checklist
A checklist of items that should be included in reports of qualitative research. You must report the page number in your manuscript where you consider each of the items listed in this checklist. If you have not included this information, either revise your manuscript accordingly before submitting or note N/A.
Developed from: Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32- item checklist for interviews and focus groups. International Journal for Quality in Health Care. 2007. Volume 19, Number 6: pp. 349–357.
To ensure the credibility and validity of the data, the confidence criteria of Guba and Lincoln, were applied.
- Credibility indicates that the results were derived from information obtained in discussion with the participants and not from other sources. The researchers spent adequate time with the interviews, developed rapport with the participants, and ensured the triangulation of data and codes.
- Transferability indicates that the search for applicability of the results in contexts distinct from the context in which the results were obtained. The researchers explained exhaustively the data collection as well as described the phenomenon in abundance of data.
- Consistency, the replicability of the data was guaranteed through meticulous descriptions of informants, itemization of the data analysis techniques, delimiting of the physical and social context in which the data collection took place, and verification of codes through triangulation.
- Neutrality, a permanent reflective consciousness was taken into account regarding personal perspective through the control of reflectivity. This was accomplished by conducting an initial reflectivity analysis prior to beginning the study, keeping a field journal, using the technique of bracketing for the preparation of the semi-structured interview script, and maintaining impartiality in structuring the results.
A phenomenological perspective with an eidetic focus was constantly maintained to ensure that the information collected was highly descriptive and involved a low level of inference, along with obtaining feedback on results returned to participants and triangulation in the coding. The primary researcher who collected the data had no professional relationship with any of the participants.
Authorization to conduct this study was obtained from the Ethics and Research Committee of the Mother-and-Child Insular University Hospital Complex [Comité de Ética e Investigación del Complejo Hospitalario Universitario Insular Materno Infantil (CHUIMI)] because the General Hospital of Fuerteventura Virgen de La Peña does not maintain a specialized unit of this type and depends on CHUIMI to function as the hospital of reference for specialties not provided at Fuerteventura. Additional permission was obtained from the management of the General Hospital of Fuerteventura and from the dialysis service of the hospital.
Prior to beginning the interviews, the informants received information about the process, were asked to give permission to be recorded using an audio recorder, were read the informed consent, and were provided with privacy and time to re-read the informed consent documents, decide whether they would like to participate and sign the documents. After the interview was conducted, it was transcribed and hand-delivered to the participant so that the participant could read it and make any changes that he or she considered appropriate.
To maintain anonymity and confidentiality of information, each informant was assigned a code.
Result
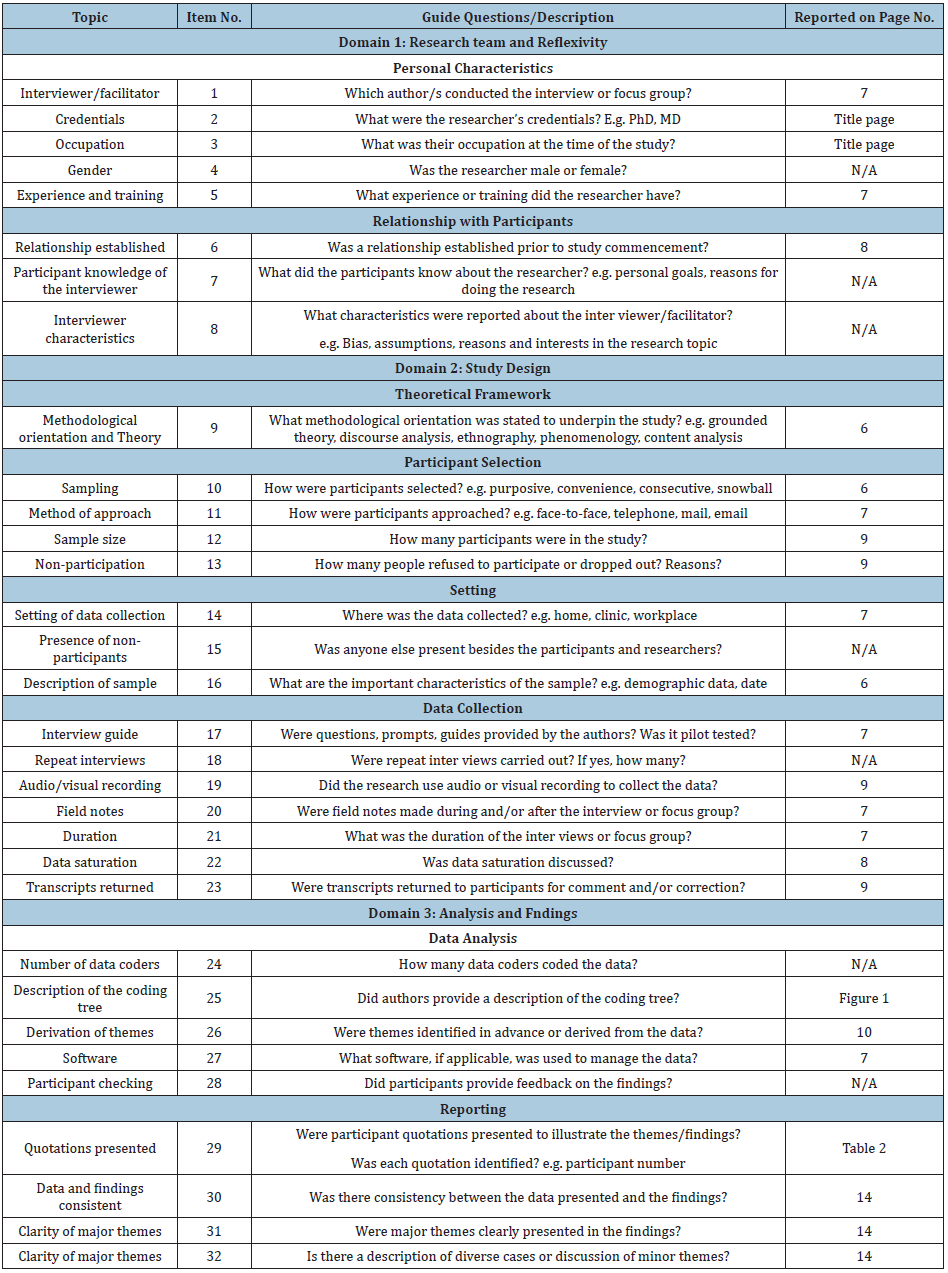
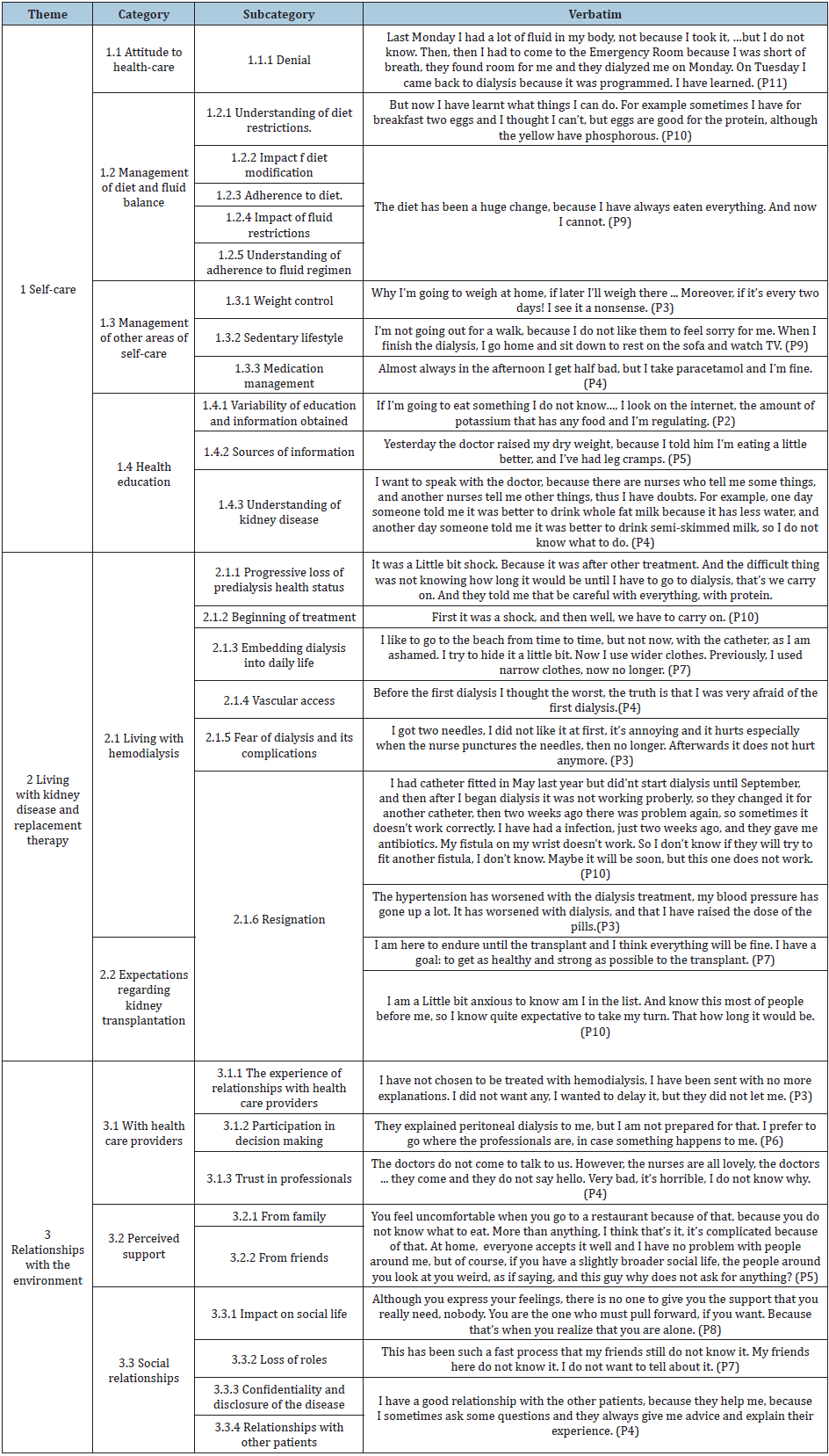
Thirteen subjects were invited to participate, and 11 agreed. Of these, seven were male, and four were female. The average age was 57 years old (between 38 and 74). Seven have no diabetes, and four have diabetes (Table 1). After transcription, coding, categorization, and analysis of the interviews, three major themes were found in the lived experience of patients after beginning hemodialysis. These were self-care, living with kidney disease and replacement therapy, and, finally, relationships with the environment. Figure 1 describe with detail the concept map resulting from the final structure of themes, categories and subcategories. Verbatims that illustrate the themes, categories and subcategories are detailed in Table 2.
Table 2: Characteristics of the 11 participants.

Figure 1: Conceptual map of themes, categories, and subcategories identified in the data analysis.
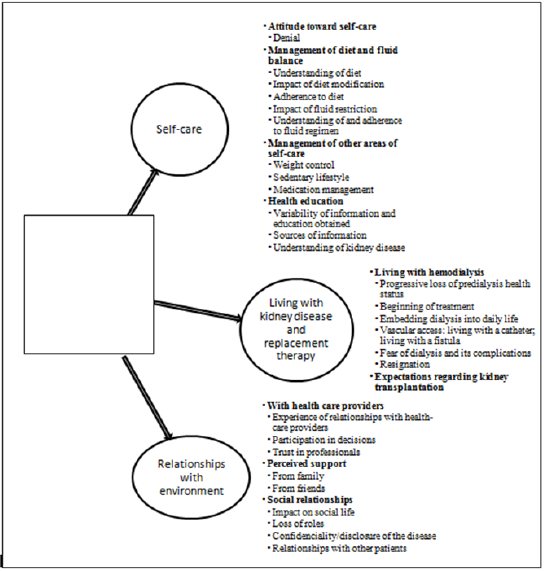
Table 3: Verbatims illustrating the categories identified.
Self-Care
This theme includes four categories, encompassing everything related to the attitude presented by informants with respect to their self-care, the experience of managing diet and fluid balance as one of the major areas with significant impact in their new lives, as well as self-care in other areas such as physical activity and medications. Finally, it includes health education, including data regarding the time at which they received this education, where they sought this information, and their degree of comprehension. Attitude to their self-care: This category refers to behaviors of the informants before the requirements of personal care derived by their health situation and the modifications introduced in their life. It includes the subcategorie denial, as a modality of response to demands of the disease (Table 2).
Managing diet and water balance: It contains not only the knowledge of the informants about the diet and fluids they should take, but also barriers or facilitators to achieve this aspect of self-care. This category was one of that informants narrate with greater significance for them, their family and friends. Subcategories identified features such as their understanding of diet restrictions, the impact of dietary modifications, and the way in which they had to transform their culinary and dietary habits, and how it has affected them in their daily lives. Moreover, adherence to the diet emerges in their discourses, describing behaviours developed to adapt the new diet to their daily life, as well as situations of lack of adherence, sometimes related to the perceived complexity of food preparation, and barriers frequently encountered in everyday situations due to social influence. Furthermore, they also describe adaptive mechanisms that favour adherence to the diet, related to the family and the environment of the patients.
In this category also arose the impact of fluid restrictions, with a high diversity of perceived influences, from those who do not consider that the restriction involves a considerable effort, even those who value this aspect as one of the worst that their disease has brought to them. Management of other areas of self-care. It includes those aspects of self-care related to the control of their weight at home and inter-dialysis weight control, the manifestations of sedentarism that are very present in the informants’ accounts, and the expressions of the participants related to self-medication or lack of adherence to prescribed medication (Table 2).
Health education. Patients transmitted those aspects of education about diet, hydric restrictions, or the care of their vascular access. They stated a high variability of the educational interventions that they received, and the need to unify criteria, because there are occasions that they receive conflicting information. They also refer the importance of the moment in which they receive the educational interventions, (in pre-dialysis consultation or already at the moment when the hemodialysis treatment has been established). They even demand interventions to empower them to make correct decisions regarding their treatment, or to know better the process of hemodialysis, and their nutritional needs. Additionally, they describe multiple sources to obtain information when they have doubts about whether they can eat a certain food, including patients’ organizations or the Internet. Eventually, they expressed very different knowledge on kidney disease, with patients who had an exact knowledge of situations derived from the disease, but many others that denoted a very low level of knowledge and a low capacity to interpret their experiences with their disease (Table 2).
Living with kidney disease and replacement therapy. This theme includes two categories: living with hemodialysis and expectations regarding kidney transplantation. Living with Hemodialysis. This category comprehends the way in which the informants lived the beginning of the treatment, their emotions and impressions on their first day of hemodialysis and the change experienced as the number of sessions lived increased. Likewise, it also incorporates the impact that treatment has had on their daily lives, how informants live during the time during which dialysis is being performed, and the effects derived from it.
They describe their progressive loos of pre-dialysis health status, with important changes in the state of perceived health and the progressive deterioration that they have been experiencing, especially due to diabetes and its complications as a frequent common denominator. The beginning of the treatment is a critical moment, that generates diverse attitudes, both positive and negative, but finally, they have to accept and adapt to this treatment, many times with resignation. Embedding dialysis into their daily life generates multiple behaviors to endure with the routine of dialysis sessions, and changes such as the presence of a vascular access in quotidian situations, or failures in fistulas, or fear of complications of dialysis (Table 2).
Expectations before kidney transplantation. This category includes the attitudes and wishes of the informants regarding the option of opting to receive a kidney transplant, or in the case of diabetic informants, a double transplant, kidney and pancreas. Including on the one hand expressions of hope for the moment of the transplant, and on the other side affirmations of passivity before the transplant (Table 2).
Relationships with the Environment
This theme describes the relationships informants have in all senses of the word, ranging from their relationships with health care providers, their social relationships, and their leisure time to the support they receive from family and friends. It constitutes the phenomenological dimension of the lived experience in relation to others. Three main categories were identified.
Relationship with health providers. It includes statements about the way informants live that relationship they have almost daily with their providers, such as nurses, nursing assistants or doctors. There are descriptions of relationships with professionals that include an acceptance of the level of communicative proactivity offered by them, but also patients who perceive a significant communicational and relational deficit in the staff, something more acute among the medical staff than in that of nurses.
This low proactivity relates to needs not covered in knowledge and coping for the management of their disease. Other notable subcategory identified is that of situations where decision-making is carried out with a poor participation of patients and families, with very asymmetric relationship in most cases. Finally, participants express a perception of control and confidence when they are attended by their usual provider, yet they distrust when they meet new staff because of their concerns on their skills and competence (Table 2).
Perceived support. This category collects information related to any type of support the participant receives from their environment, either from their family or from their friends, as they have perceived it. Their discourses demonstrate the importance of this resource for coping with the disease and the permanent availability of support for patients, although in the case of friendships, perceived links and the influence of support is perceived with much less intensity. Family support constitutes one of the main sources of acceptance, although support from friends is not always ensured (Table 2).
Social relationships. In this category, the aspects dealt with by the informants about their relationships in general, including the social life they have in comparison with what they could have before starting with the hemodialysis treatment, the way in which they socialize the disease with their friendships and acquaintances, and the relationship they have with other patients, the things they talk before they start dialysis and experiences they share. The impact on social life is expressed with feelings of loneliness that they may have as a consequence of dialysis limitations for social performance. Likewise, the loss of roles may involve losing their jobs, or not being able to perform the same domestic tasks or physical exercise as before the start of dialysis. Some patients confessed that they had concerns with confidentiality and disclosure of the disease, since they did not share their disease and the treatment with friends. Eventually, many narratives revealed the existence of links and relationship with other patients, many times in the waiting room, before being able to access the dialysis ward (Table 2).
Discussion
Denial was found to be a type of response to self-care that had a notable impact on the informants' disease perception and course. In relation to denial and resignation, some authors [10,16] found participants who tended to feel that their disease was a punishment for their sins and who prayed to God for forgiveness or looked for a relationship between their disease and their life's destiny.
With regard to diet, the participants who exhibited dietary adherence described facilitators such as family support, above all that of a spouse, or children in the case of elderly persons, or the motivation to be healthy at the time of transplantation; the patients who perceived greater support from their family members had greater overall dietary adherence. These findings coincide completely with those obtained by Griva et al. [11]; participants in that study indicated that family support helped with dietary adherence in terms of food preparation as well as making it possible for them to avoid the negative secondary consequences of lack of adherence.
On the other hand, participants who are considered to lack dietary adherence reflected a lack of knowledge regarding preparing recipes as a major barrier to adherence. Additionally, these informants felt that they had suffered too much change in their eating habits, even including in some cases the need to prepare two different meals in the home. Also arising was the issue of modifying cultural customs related to nutrition.
With regard to this, Griva et al. [11] observed difficulty in the management of comorbidities in relation to multiple and contradictory dietary recommendations; this coincides with the argument that cultural changes regarding nutrition can distance patients from their families. Likewise, they add that participants indicated a limited understanding of dietary guidelines and did not understand the nutritional value or content of different foods.
Adjusting to fluid restrictions is associated with a variety of outcomes. Non-adherent patients believe that they should be drinking more water to feel better or that they should drink when it is hot outside. However, in the bibliography consulted, lack of adherence to fluid restrictions has been found to be an act of rebellion or to be caused by a lack of training in how to calculate the quantity of fluid ingested or the amount of weight gained [10,13]. Additionally, some authors identified patients who did not adhere to fluid restrictions because they believed that dialysis would compensate for the excess liquid, which led to decreased interest in respecting this limitation [13]. However, this aspect was not identified in the informants in our study.
Participants demand more education regarding appropriate nutrition and wish to received non-contradictory information from health care personnel; they mention having received different instructions about the same thing and indicate that this provokes confusion, a finding that coincides with the results reported by Griva et al. [11].
The information the participants obtained on managing their condition came from medical and nursing personnel, from hospital-created pamphlets, through the kidney disease association (ALCER), from peers in dialysis centers while waiting for treatment, or from the Internet. As regards health literacy, many studies have analyzed the quality of information that can be easily accessed on the Internet regarding diet, kidney disease and its treatment [17-23]. These studies conclude that the information found on the Internet regarding chronic kidney disease is often of poor quality or is difficult to understand or implement; this is true to a greater extent for persons of low economic status, elderly persons, males and ethnic minorities, resulting in a lack of self-care and creating a barrier to a shared decision-making process [20-23].
With regard to the impact of beginning dialysis, it was observed that the attitude participants display is related to their work. There was generally indifference to the situation if they did not work, were retired, or disabled; if they must go to the hospital three times a week, they go. In the same vein, nonconformity due to denial of the disease at the outset was seen; the process of acceptance was difficult, especially in young persons. Participants with comorbidities spoke about their indifference to beginning dialysis as it was just one more treatment.
In contrast, some participants thought about dying after learning that they would have to depend on a machine for four hours three times per week; other participants commented that they could not believe what was happening to them, implying a shock in that moment, with denial of the disease and even despair. These feelings were overcome because they felt they must continue onward, and they became accustomed to the routine, though still without enjoying it; at least, however, they no longer felt fear because they understood what it was.
Many participants experienced physical and psychological improvement, commenting that lack of knowledge provoked uncertainty but that when one knows what it means and what it is, things get better. With that, although they may have begun dialysis with a positive or a negative attitude, they ended up adapting to the situation. However, they recognized the daily impact of not being able to take vacations and to travel. Some believed that they had gone from everything to nothing, without noting physical change; others felt that they had experienced a complete change in their lives, feeling tired and lazy or dizzy after dialysis, and that this impeded them from doing all that they would like to do. They felt they had a different routine of life, mentioning the change in diet, restrictions regarding fluids and alcohol, having to take pills, and having to be at the hospital three days a week.
On the other hand, other participants felt an improvement, mentioning that their blood pressure had improved, their poorly controlled diabetes had improved, they had better appetite, and they breathed better, including one who no longer felt sick. In discussions, they mentioned that treatment is more enjoyable if they have some form of entertainment such as watching television, listening to music, or reading a book. One participant mentioned passing the time by sleeping. When a participant has experienced an increase in dialysis treatment time, the added time is considered a greater burden because they were accustomed to less treatment time.
These results coincide with the results obtained in various qualitative studies [10,12,16,24,25] in which the participants reported feeling fear and shock at beginning treatment thinking of their future, but after a time felt lighter and breathed better and felt gratitude for dialysis because it helped them live longer, although some mentioned physical and psychological problems such as fatigue, lack of sleep, restlessness, dizziness, tingling, and decreased quality of life due to hemodialysis. In a similar manner, they refer to the inconvenience of being unable to travel or work or perform their daily routines normally and independently, a restriction that stresses them and makes them feel unhealthy. As a result, they present symptoms of depression due to decreased quality of life.
Regarding vascular access, the discussions did not include frequent mentions of fistulae. The participants did not report significant problems but only reported feeling brief discomfort at the time of puncture. The reason for this may be that the informants were new to hemodialysis, and many had had a catheter placed and were waiting for the fistula to mature. Because the interviews were with persons relatively new to dialysis, many had catheters, and discussion was more related to the discomfort and inconvenience of having a permanent catheter. Participants mentioned that the catheter caused feelings of stress and a sensation of being unwell because they had been required to change their routines to avoid infections and complications.
With regard to fear of dialysis and its complications, a fear of the unknown was found. On the first day of dialysis, most patients did not know what would happen to them, did not know how it would be, and found themselves lost in myths and fears; however, when the experience was good and they observed that nothing much happened, they relaxed. This finding coincides with the results reported by Aghakhani et al. [17]; there, participants reported having lived with a great deal of anxiety about beginning hemodialysis treatment on their first visit to the hemodialysis center and thinking that they were going to be sick for the rest of their lives.
Regarding transplantation, on one hand passivity was observed due to fear of secondary complications of transplantation. On the other hand, there were participants who felt a motivation to become stronger and healthier after transplantation, although they were anxious to know whether all the tests had been completed and whether or not they had been placed on the transplant list. In this regard, they required more information. These results concur with those obtained in various studies [25,26] there is recurring concern over wait times for kidney transplantation as well as worry about organ rejection and lack of availability of information regarding the management of transplant waiting lists [26]. Salter et al. [25] found some participants who were opposed to transplantation due to the quantity of pills they would have to take afterward, fear of organ failure or rejection, or fear of surgery, as well as for other reasons such as age.
It was found that there are situations in which there is limited participation in the decision-making process; in the discussions, the patients reported that they had very limited participation in choosing the replacement therapy most appropriate for them according to their interests and quality-of-life prognosis. The informants showed confidence in the therapeutic decisions made by doctors and respected them, believing that they are the best. Along these lines, Ladin et al. [27] found that the patients interviewed had the sense that they had not made the decision to begin dialysis treatment; it had been a decision influenced by a perception of imminent death or by the belief that they should decide to begin dialysis as the doctors were supposed to be the ones to make this decision. They conclude that the medical team and the family often override the patient's preferences and do not respect their autonomy in decision making.
In this study, it was found in discussions that all but one of the participants perceived support received from family as very helpful in making it possible for them to cope with the disease on a daily basis and that family is a great help in food preparation and dietary adherence; however, one informant felt that the family was burdensome and judgmental.
According to some authors, family support is important, providing a fundamental pillar for accepting and surviving a chronic disease; it helps patients with nutrition and activities of daily living, alleviates stress, and motivates them in their self-care so as to not be a burden on their loved ones [11,13,24].
In contrast, Davison [28] observed that family can be a barrier to advanced care planning for participants because, in the presence of their families, some participants were unable to speak honestly about their hopes and desires, which led them to feel hopeless and isolated. In the results obtained by Chun-Chih et al. [10], informants reported having created a state of isolation because they believe that, until a person goes through what they are experiencing, they will be unable to understand how difficult it is for them.
This can be compared with some discussions with participants in the present study who felt that they had friendships in which they could find support but that if one continues to have the same problems, one is alone, and the support will not be enough. They felt isolated because they believed that although they express their feelings no one gives them the support they need and they are alone with their disease. Some expressed feeling shame and discomfort when they go out to spend time with friends or family and cannot order something to drink. As a result, in some cases, they believe that it is important for those around them to understand the disease they suffer from, as this would make it easier to accept their disease and prevent uncomfortable situations. Still other participants did not want to accept their disease and preferred to hide it, not wanting to provoke pity from their friends or acquaintances.
Finally, informants expressed a loss of role, provoking discouragement; this was a common theme in discussions with informants. They expressed a lack of motivation, a lack of energy for performing daily activities, and boredom because they did not know how to pass the time with nothing to do. This sensation led them to fall into despair because they do not feel better and because they feel tired and do not leave their homes. They expressed feeling bitter and, in one case, needed a psychologist as part of the care team.
This coincides with the results of various studies [10,11,16,24]. There is a loss of purpose and of quality of life. Due to fatigue and the time that treatment demands, dialysis patients no longer had time to work or to enjoy leisure time and self-care; this provokes depressive episodes with powerlessness and anxiety about the future because they feel bound to the dialysis machine and feel a loss of independence.
The participants in this study reported that they received help and support from their peers in the dialysis waiting room before going in for treatment. Some mentioned sharing experiences with certain foods, commented on the excess weight they carried each day, advised each other about procedures they had experienced such as testing for the transplant list, the waiting times that transplants usually involve, or catheter removal in preparation for use of vascular access. Similarly, on other occasions they spoke of things other than their disease such as fishing or soccer. This complicity becomes a feeling of companionship or friendship, creating a bond of mutual support and trust. Salter et al. [25] found that some participants felt they received greater emotional support from their companions than from their families and friends and that in this way they managed to create close bonds of mutual support. Patients grew to know about each other because the dialysis setting facilitates this sort of information exchange among patients [11], and this communication amongst them eases the time spent waiting for their connection to the dialysis machine.
Among the limitations of this study, the most important is the difficulty in finding a sample of participants. In addition, it was also difficult to arrange some interviews due to lack of commitment and availability of the participants. With some participants, a shyness or fear of making mistakes in discussions was detected. Furthermore, the cultural and health care context in which this study was conducted may not be similar to that found in other geographic areas, and a comparison in other health care settings in our geographic area is necessary to test the transferability of the results.
Conclusion
The lived experience of persons suffering from chronic kidney disease revolves around three major axes: a sudden change in the disease resulting in the need for renal replacement therapy, the experience of self-care, and relationships with immediate social and family environments. The way in which patients perform self-care is shaped by the attitudes they develop around self-care behaviors, health literacy, and adjustment to self-care as it relates to dietary and fluid restrictions as one of the major areas of adjustment required in this disease.
Kidney transplantation is a source of hope in everyone interviewed and acts as a positive motivation for the patients to maintain adherence to the behaviors required in caring for their disease. Also, perceived support from family members and friends is a fundamental pillar that shapes and changes adjustment processes and self-care, especially in areas such as diet and fluid balance, in which more barriers may appear. Patients can create relationships of mutual support with each other that in some cases are quite substantial. Nephrology services and nurses should explore the possibilities of this capacity for support among equals when planning care for these patients [29].
The findings of this study represent contributions that may help focus the clinical practice of professionals in nephrology services and may help them identify problems that could otherwise pass unnoticed or be normalized by professionals in terms of their significance. Planning services and interventions for persons beginning renal replacement therapy should take into account the major impact that self-care has on the lived experience of these patients.
Relevance to Clinical Practice
The importance of adherence to treatment and acceptance of the disease, self-care, and support from the immediate environment of persons in hemodialysis, as well as the creation of support groups in waiting rooms or during treatment, have been demonstrated in this study.
Good health literacy should be implemented from the early stages so that the patient is able to participate in the process of decision-making regarding his or her treatment with a real awareness of the implications of his decisions; this increases acceptance and self-care and improves relationships with health care providers. Accurate information regarding transplant waiting lists and required tests reduces anxiety, increases confidence in health care providers, and improves quality of life.
References
- Kim Y, Evangelista LS, Phillips LR, Pavlish C, Kopple JD (2010) The End-Stage Renal Disease Adherence Questionnaire (ESRD-AQ): testting the psychometric properties in patients receiving in center Hemodialysis. Nephrology Nursing Journal 37(4): 377-393.
- Vlaminck H, Maes B, Jacobs A, Reyntjens S, Evers G (2001) The dialysis diet and fluid non-adherence questionnaire: Validity testing of a self-report instrument for clinical practice. Journal of Clinical Nursing 10: 707-715.
- Gardner CL (2015) Adherence: a concept analysis. International Journal of Nursing Knowledge 26(2): 96-101.
- Lehane E, McCarthy G (2009) Medication non-adherence. Exploring the conceptual mire. International Journal of Nursing Practice 15: 25-31.
- Matteson ML, Russel C (2010) Interventions to improve hemodialysis adherence: a systematic review of randomized- controlled trials. Hemodialysis International 14: 370-382.
- Gonzalez Oquendo L, Morales Asencio JM, Bonill de Las Nieves C (2017) Contributing factors for therapeutic diet adherence in patients receiving haemodialysis treatment: an integrative review. J Clin Nurs 26(23-24): 3893-3905.
- Gerbino G, Dimonte V, Albasi C, Lasorsa C, Vitale C, et al. (2011) Adherence to therapy in patients on hemodialysis. G Ital Nefrol 28(4): 416-424.
- Russel CL, Cronk NJ, Herron M, Knowles N, Matteson ML, et al. (2011) Motivational Interviewing in Dialysis Adherence Study (MIDAS). Nephrology Nursing Journal 38(3): 229-236.
- Walsh E, Lehane E (2011) An exploration of the relationship between adherence with dietary sodium restrictions and health beliefs regarding these restrictions in Irish patients receiving haemodialysis. Journal of Clinical Nursing 20(3-4): 331-340.
- Chun Chih L, Chin Yen H, I Ju P (2015) A Qualitative approach of psychosocial adaptation process in patients undergoing long-term hemodialysis. Asian Nursing Research 9: 35-41.
- Griva K, Ng HJ, Loei J, Mooppil N, McBain H, et al. (2013) Managing treatment for end-stage renal disease-a qualitative study exploring cultural perspectives on facilitators and barriers to treatment adherence. Psychology & Health 28(1): 13-29.
- Krespi R, Bone M, Ahmad R, Worthington B, Salmon P (2004) Haemodialysis patients’ beliefs about renal failure and its treatment. Patient Education and Counseling 53: 189-196.
- Smith K, Coston M, Glock K, Elasy TA, Wallston KA, et al. (2010) Patient perspectives on fluid management in chronic hemodialysis. Journal of Renal Nutrition 20(5): 334-341.
- Morse JM (2003) Emerging from data: The cognitive processes of analysis in qualitative research. In Critical issues in qualitative research methods. University of Antioquia pp. 30-51.
- Tong A, Sainsbury P, Craig J (2007) Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. International Journal for Quality in Health Care 19(6): 349-357.
- Aghakhani N, Sharif F, Molazem Z, Habibzadeh H (2014) Content analysis and qualitative study of hemodialysis patients, family experience and perceived social support. Iranian Red Crescent Medical Journal 16(3): e13748.
- Cavanaugh KL, Wingard RL, Hakim RM, Eden S, Shintani A, et al. (2010) Low health literacy associates with increased mortality in ESRD. Journal of the American Society of Nephrology 21(11): 1979-1985.
- Fraser SD, Roderick PJ, Casey M, Taal MW, Yuen HM, et al. (2013) Prevalence and associations of limited health literacy in chronic kidney disease: a systematic review. Nephrology Dialysis Transplantation 28(1): 129-137.
- Green JA, Mor MK, Shields AM, Sevick MA, Arnold RM, et al. (2013) Associations of health literacy with dialysis adherence and health resource utilization in patients receiving maintenance hemodialysis. American Journal of Kidney Diseases 62(1): 73-80.
- Lai AY, Ishikawa H, Kiuchi T, Mooppil N, Griva K (2013) Communicative and critical health literacy, and self-management behaviors in end-stage renal disease patients with diabetes on hemodialysis. Patient Education and Counseling 91(2): 221-227.
- Lambert K, Mullan J, Mansfield K, Koukomous A, Mesiti L (2017) Evaluation of the quality and health literacy demand of online renal diet information. Journal of Human Nutrition and Dietetics 30(5): 634-645.
- Taylor DM, Fraser S, Dudley C, Oniscu Gc, Tomson C, et al. (2017) Health literacy and patient outcomes in chronic kidney disease: A systematic review. Nephrology Dialysis Transplantation 1-14.
- Taylor DM, Fraser SDS, Bradley JA, Bradley C, Draper H, et al. (2017) A systematic review of the prevalence and associations of limited health literacy in CKD. Clinical Journal of the American Society of Nephrology 12(7): 1070-1084.
- Niu H, Liu J (2017) The psychological trajectory from diagnosis to approching end of life in patients undergoing hemodialysis in China: A qualitative study. International Journal of Nursing Sciences 4: 29-33.
- Salter ML, Kumar K, Law AH, Gupta N, Marks K, et al. (2015) Perceptions about hemodialysis and transplantation among African American adults with end-stage renal disease: Inferences from focus groups. BMC Nephrology 16: 49.
- Calestani M, Tonkin Crine S, Pruthi R, Leydon G, Ravanan R, et al. (2014) Patient attitudes towards kidney transplant listing: qualitative findings from the ATTOM study. Nephrology Dialysis Transplantation 29: 2144-2150.
- Ladin K, Lin N, Hahn E, Zhang G, Koch Weser S, et al. (2017) Engangement in decision-making and patient satisfaction: a qualitative study of older patients’ perceptions of dialysis initiation and modality decisions. Nephrology Dialysis Transplantation 32(8): 1394-1401.
- Davison SN (2006) Faciliting advance care planning for patients with end-stage renal disease: the patient perspective. Clinical Journal of the American Society of Nephrology 1: 1023-1028.
- Prieto MA, Escudero MJ, Suess A, March JC, Ruiz A, et al. (2011) Analysis of perceived quality and patient expectations in the dialysis care process. Annals of The Health System Of Navarra 34(1): 21-31.
© 2020 Lissete González Oquendo. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






