- Submissions

Full Text
COJ Nursing & Healthcare
Managing Sensitive Skin Syndrome in Private Clinic Setting: The Pivotal Role of Clinical Nursing Through a Biopsychosocial Approach
Kam Tim Michael Chan*
Adjunct Professor of Master Course of Common Goods and Public Health, Baptist University, Hong Kong SAR, China
*Corresponding author: Kam Tim Michael Chan, Specialist in Dermatology, Adjunct Professor of Master Course of Common Goods and Public Health, 2128- 2129, Pioneer Centre, 750, Nathan Road, Mongkok, Kowloon, Hong Kong SAR, China
Submission: March 12, 2020;Published: April 15, 2020

ISSN: 2577-2007Volume6 Issue2
Abstract
Sensitive Skin Syndrome (SSS) is a neurocutaneous condition with the undefined etiology, pathogenesis and treatment. It is difficult and challenging for primary health care doctors and dermatologists to manage SSS in a busy private clinical setting. Therefore, many patients with SSS are poorly managed and their negative experiences fail to relieve the neurological symptoms. Also, the prior knowledge and perception of patients to the syndrome may misunderstand the symptoms in subsequent consultations because of nocebo effects. The following based on a biopsychosocial model of somatic symptoms, which focuses on the crucial relationship between the patient and clinic service provider, the following discussion will emphasize on the important role of nursing care in private clinic setting for better SSS management.
Keywords: Sensitive skin syndrome, Biopsychosocial model, Nursing care, Individualized management, Negative perceptions and expectancies, Psychological therapy through learning principles
Abbreviations: IFSI: International Forum for the Study of Itch; QoL: Quality of Life; SSS: Sensitive Skin Syndrome; TEWL: Trans Epidermal Water Loss
Introduction
Sensitive Skin Syndrome (SSS) is a common acute skin condition that prompt patients to seek immediate medical attention in private care clinic setting [1]. The worldwide prevalence of SSS is 40% [2-5]. It was estimated that up to 10% of patients present with manifestations of severe sensitive skin and seek medical consultation [6].
In this field, whether SSS is a syndrome, physiological condition or pathological disease is still debatable [7]. International Forum for the Study of Itch (IFSI) defined SSS as a syndrome of unpleasant sensations, such as stinging, burning, pain, pruritus, and tingling sensations, in response to stimuli that normally should not provoke such sensations [5]. It significantly affects Quality of Life (QoL) and health of patients and their family members. However, these unpleasant sensations cannot be adequately explained by other skin lesions or diseases. Despite advancement of science, neither diagnostic test nor evidenced based treatment study existed for its management.
As a complete system of science, medical dermatology has evolved from simply disease treatment to prevention, health care, nursing maintenance and rehabilitation. Here, SSS is regarded as a spectrum of epidermis neurological continuum with stimulus, cognitive and patient distinct perceptive involvement. Albeit the role of dermatologist in making the clinical diagnosis is indispensable, that of the attending clinical nurse in the management of SSS is pivotal. It is believed that the clinical nurse care is fundamental to alleviating the psychological, social and occupational impacts and burdens of SSS to the patients and the community. The following discussion focuses on the functions of nursing care in the management of SSS based on an established biopsychosocial model and perspective [8].
Functions of the Nursing Care
Explanation and education of patients
SSS is a somatic condition with skin unpleasant sensations or perceptions like pruritus, pain, tightness and burning sensation with uncle aetiology, pathogenesis and prognosis. Clinical nurses can explain the complicated condition in detail to patients by emphasizing its anatomical, neurophysiological and psychological knowledge. According to the evidence-base information nurses not only provide potential causes of the unpleasant sensation, such as epidermal skin damages, dry skin due to trans epidermal water loss (TEWL), neurological dysfunction, involvement of aberrant neuromediators and stress, but also clarify SSS-related myths and misconceptions. For examples, most of the patients always get confused that SSS is a chronic incapacitating disease like atopic eczema or a psychiatric disease.
In addition, patient education clarifies unproven claims and treatments of SSS reported in mass media, including television, newspaper and internets. They facilitate and proclaim unsubstantiated adverse health effects and information, regarding the negative expectancies of SSS patients. Before proper management, for instance, patients have the negative expectancies and prior negative perceptions that simply applying non-sensitive moisturizers will minimize the benefits or even cause negative effects through the nocebo mechanism [9,10]. Therefore, in the case of windmill syndrome due to a self, nurses can explain and reduce the media attention and the frequent reports of complaints which fulfill nocebo mechanism.
Communication and interrogation of patients
A reliable patient-nurse relationship develops and enhances a mutual rapport and trust. Effective and good communications promote the therapeutic roles of the caring nurses. From our experiences, like many other severe recalcitrant skin conditions, SSS patients unlikely disclose their detailed information regarding severity, intensity, duration, time of occurrence of the baffling sensations and the triggering factors of the condition to the doctors, because of negative expectancies and time limited of doctors.
This interrogative role will be effectively carried out by the nurses especially during informal patient-nurse discussion. In this situation, patients will voluntarily report cognitive, behavioural, social and occupational features associated with SSS to the nurse. Assessment of the above and avoidance of the triggering factors are very important management in SSS as there is no effective pharmacological treatment till now. In the psychoneurobiological model, for example, relevant factors like personality (personal factors), stressors (external factors), mediating factors like unreasonable worries, behavior and social factors like social avoidance and lack of support and network are all involved in SSS. Through identification and psychological behavioral intervention, it is possible to develop skills for healthcare professionals and patients to manage these individual factors .
Psychological Therapy through Counselling and Learning Principles
Based on the psychoneurobiological model, which focuses on psychoneurobiological mechanisms, good communication skills from the attending nurses like positive verbal suggestion: “This (treatment) involving moisturizers is going to make you feel better”, social cues like body language and voice cues will have a placebo effect and minimizing nocebo effects on the patients with SSS. The latter one is a common patient experience as many doctors and healthcare service providers were not well-trained in SSS. Also, the patents in many occasions who are dismissed as psychological development is the lack of an organic basis. So, this prior negative unrewarding clinical experience significantly affect the patient’s perception in the future management of SSS.
During subsequent clinical consultation, this prior knowledge predicts a negative perception and results a negative expectancy, particularly under for cosmetics which may induce allergy. Persistent negative expectancies become an important risk factors of sensitization in chronic somatic symptoms, and SSS is related in a psychoneurobiological mechanism [11,12]. Somatic symptom of unpleasant or suffering itch as perceptual dysregulation resulting a negative expectancy was correlated with a neuro-endocrine mechanism through dysregulation of endogenous oxytocin, cortisol and other neurotransmitters in the brain-endocrine-skin axis [12]. Therefore, positive cognitive and behavior psychotherapy, learning principles plus mechanical conditioning are advantages in motivating the bias prior knowledge, perceptions and confounded predictors back to the healthy, mindful, physiologically constructive brain [13].
Adherence, Maintenance and Follow up of a Personalized Care Management Plan
The clinic nurses are also crucial in managing the SSS patients personally as many other neurological conditions, which show highly variable in symptoms, responses, adherence, follow-ups to treatments and management. Such personalized variation includes genetic factors and internal factors like the personality of the patients. Additionally, other factors are considered, such as the positive and negative expectancies, prior knowledge of the condition and the cognitive state of the patients. The conventional model of a stimulus inducing somatic response has shifted to psychoneurobiological pathways, which are significantly affected by prior knowledge as the generative model of perception in our mind. In general, the patients are just like any other individuals; our response and behavior are affected by our previous knowledge, experiences and expectancies. Thus, it is proposed that a personalized approach for effective SSS management is a possible for patients in clinic setting.
Therapy administration, in terms of emollients and topical agents, reduces TWEL and pruritus, and restores the barrier function like calcineurin inhibitors. Other methods such as drug therapy, low dose laser therapy, LED treatment, probiotics have not yet been verified in double blinded controlled study. Therefore, it seems that adherence to emollients or humectants therapy, and life- style modifications are feasible management strategy of SSS with difficult clinical conditions. With this concept, nurses in charge enhance and support the adherence, sensible lifestyle modifications, environmental adjustments and supportive psychotherapy to improve skin condition of the patients. Especially during acute flare, the nurses should advise to the patients through telephone consultation. The nurse should arrange follow-up consultation to monitor the progress and update the new evidencebased the condition of the patients.
Prevention of SSS
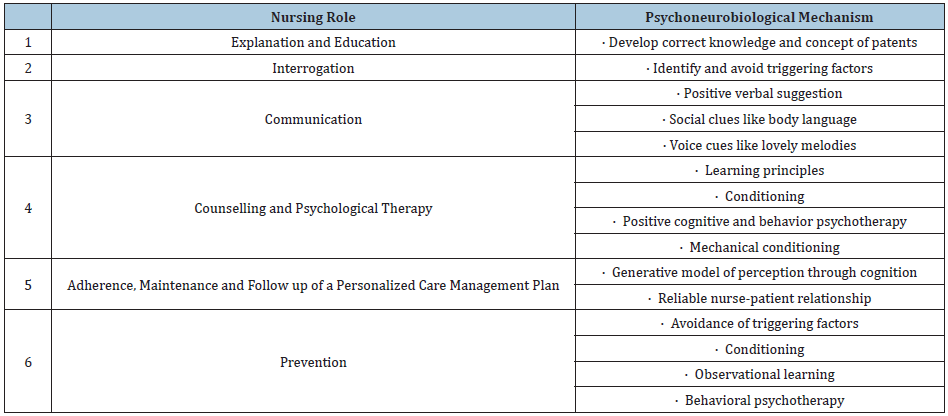
Finally, as other syndromes and diseases, prevention is always better than cure. In this aspect, nurses can advocate and empower the patient on effective approaches to prevent the flareup of SSS. According to a systemic literature of SSS, The common triggering factors are cosmetics, wet air, air conditioning, heat and water. Other possible triggering factors are physical variations in temperature, cold, wind, solar radiation, air conditioning, dry air, chemical, pollution and emotional factors [14]. Verbal suggestions encourages the patients to use non-sensitive skin care products, which exclude known sensitive ingredients like fragrances and irritants. Furthermore, a stable air condition especially in humidity, temperature and pH should be regulated. Thus, psychological and emotional factors, as well as psychological behavioral intervention are useful in the integrative approach of the nursing functions of SSS management. Table 1 summarized general psychoneurobiological approaches of the nursing roles in SSS management.
Table 1: SSS management by psychoneurobiological mechanism through clinic nurse based on biopsychosocial model.
Conclusion
Patients with sensitive skin syndrome require a personalized and integrated approach, by considering various biomedical, neural and psychosocial factors which induce sensitive skin syndrome. In general, nurse can suggest patients to avoid possible triggering factors and use cosmetics with inhibitors of unpleasant sensations, or insensitive skin care products. Other psychotherapies, like verbal suggestions, conditioning and observational learning, will be relevant for some SSS patients especially those with a biased negative prior knowledge predict negative percept to the condition. To date, there is neither clinical trial to support the use of topical or systemic drugs in sensitive skin, nor study to provide data to reach a consensus on sensitive skin management. It concludes that sustainable experienced nursing care play a pivotal role in effective management (Figure 1).
Figure 1: Role of nurses in the management of SSS in clinic setting based on the biopsychosocial model.

Acknowledgement
The author thanks Dr. SKC Cheung for providing medical editorial support.
References
- Chan KTM (2018) Clinical review on sensitive skin: History, epidemiology, pathogenesis and management. J Clin Exp Dermatol Res 9(4): 453.
- Misery L, Myon E, Martin N, Verrière F, Nocera T, et al. (2005) Sensitive skin in France: An epidemiological approach. Ann Dermatol Venereol 132(5): 425-429.
- Misery L, Boussetta S, Nocera T, Perez-Cullell N, Taieb C (2009) Sensitive skin in Europe. J Eur Acad Dermatol Venereol 23(4): 376-381.
- Misery L, Sibaud V, Merial Kieny C, Taieb C (2011) Sensitive skin in the American population: Prevalence, clinical data and role of the dermatologist. Int J Dermatol 50(8): 961-967.
- Misery L, Ständer S, Szepietowski JC, Reich A, Wallengren J, et al. (2017) Definition of sensitive skin: An expert position paper from the special interest group on sensitive skin of the international forum for the study of itch. Acta DermVenereol 97(1): 4-6.
- Chan KTM (2019) A prospective study on the characteristics of sensitive skin syndrome in Chinese patients attending a private clinic-based setting in Hong Kong. J Clin Exp Dermato Res 10(4): 498.
- Chan KTM (2020) Is Sensitive Skin a Disease, Syndrome, a Disorder or Else? Arch Neurol & Neurosci 7(1): 1-3.
- Verhoeven EW, de Klerk S, Kraaimaat FW, van de Kerkhof PC, de Jong EM, et al. (2008) Biopsychosocial Mechanism of Chronic itch in Patients with Skin Disease: A Review. Acta DermVenereol 88(3): 211-218.
- Witthöft M, Rubin GJ (2013) Are media warnings about the adverse health effects of modern life self-fulfilling? An experimental study on idiopathic environmental intolerance attributed to electromagnetic fields (IEI-EMF). J Psychosom Res 74(3): 206-212.
- Winters W, Devriese S, Van Diest I, Nemery B, Veulemans H, et al. (2003) Media warnings about environmental pollution facilitate the acquisition of symptoms in response to chemical substances. Psychosom Med 65(3): 332-338.
- Henningsen P, Gündel H, Kop WJ, Löwe B, Martin A, et al. (2018) Persistent physical symptoms as perceptual dysregulation: A neuropsychobehavioral model and its clinical implications. Psychosom Med 80(5): 422-431.
- Otten M, Pinto Y (2017) A social Bayesian brain; How social knowledge can shape visual perception. Brain Cogn 112: 69-77.
- Ever AW (2017) Using the placebo effect: How expectations and learned immune function can optimize dermatological treatments. Exp Dermatol 26(1): 18-21.
- Brenault E, Barnetche T, Le-Gall Ianotte C, Roudot AC, et al. (2020) Triggering factors in sensitive skin from the worldwide patient’s point of view: a systematic literature review and meta-analysis. J Eur Acad Dermatol Venereol 34(2): 230-238.
© 2020 Kam Tim Michael Chan. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






