- Submissions

Full Text
COJ Nursing & Healthcare
Facilitators and Barriers of Modifiable Behaviours that Reduce the Risk of Developing Type 2 Diabetes in Adulthood: An Integrative Review
Hadwan Mibrad Aldahmashi RN1*, Mohammed Senitan Menzies2 and Vasiliki Betihavas1
1MN Faculty of Medicine & Health, Sydney University, Saudi Arabia
1Department of Public Health, Saudi Electronic University, Saudi Arabia
*Corresponding author: Hadwan Mibrad Aldahmashi RN, MN Faculty of Medicine & Health, Sydney University. Ministry of Health, Saudi Arabia
Submission: April 19, 2019;Published: March 19, 2020
ISSN: 2577-2007Volume6 Issue2
Abstract
Background: The risk of developing type 2 diabetes (T2DM) is significantly increased by various modifiable factors, such as obesity, unhealthy diet and sedentary lifestyle. This implies that T2DM can be partially prevented and its progression and complications can be minimised by altering these modifiable risk factors, particularly among the adult population.
Aim: The main aim of this review was to identify barriers and facilitators of modifiable behaviours for reducing the risk of developing T2DM.
Methods: An integrative review was undertaken. A computerised systematic search for relevant studies was performed on Cumulative Literature Index of Nursing and Allied Health Literature (CINAHL), MEDLINE and Sociological Abstracts. Thematic synthesis was performed to analyse the included studies.
Results: Following critical appraisal a total of 19 studies, six quantitative and 13 qualitative, were reviewed. Three main themes concerning modifiable behaviours were identified from the studies: physical activity, diet and smoking. The review identified numerous internal and external factors affecting for these modifiable behaviours, which were classified and synthesised under two main themes: (1) barriers to and (2) facilitators of modifiable behaviours. Four subthemes were identified and discussed as barrier to modifiable behaviours, including
Personal factors, such as health and emotional issues.
Social factors, such as lack of social support;
Informational factors, such as inadequate knowledge and awareness and
Environmental factors, such as climate and individual settings. Conversely, three subthemes were identified as facilitators for modifiable behaviour, including
Personal factors, such as motivation.
Social factors, such as adequate social support and
Informational factors, such as adequate knowledge and awareness.
Conclusion: Numerous factors can facilitate or bar adult engagement in modifiable behaviours that reduce the risk of developing T2DM. Strategies to enhance modifiable behaviours should focus on education and counselling, enhancing individual self-efficacy and promoting social support.
Keywords: Modifiable behaviours; Lifestyle intervention; Physical activity; Diet; Diabetes prevention; Diabetes mellitus; Smoking
Introduction
Overview
Type 2 diabetes mellitus (T2DM) is the most common chronic metabolic disorder and affects millions of people worldwide [1]. An estimated 422 million people worldwide have diabetes, which represents 9% of the global adult population [2]. Approximately 90% of diabetes cases are T2DM. The prevalence rate of diabetes in high-income countries is around 6%, which is slightly lower than the 7% in low-income countries [2]. T2DM is associated with numerous adverse multisystemic morbidities and a significantly high risk of mortality, especially if it is not effectively managed [3]. This means that effective strategies for T2DM management should typically target primary, secondary and tertiary prevention [4]. While genetic factors can contribute to T2DM, there is overwhelming evidence that the risk of developing T2DM is significantly increased by various modifiable factors, such as unhealthy diet and sedentary lifestyle.
Modifiable behaviours that reduce the risk of T2DM
Since various modifiable behaviours contribute to the highest proportion of T2DM cases, they must be adjusted to reduce the disease risk. Hence, modification includes minimising sedentary lifestyle factors by increasing physical activity (PA) and having a healthy dietary intake [5]. However, other considerable modifiable behaviours may include cessation of smoking, decreased alcohol intake, elimination of environmental toxins, sleep pattern and positive lifestyles with minimal stress and anxiety [6]. Increasing PA and dietary fibre intake is effective in reducing the risk of T2DM [5]. For instance, Knowler et al. [7] stated that individuals who are physically active and eat healthy diet have reduced likelihood of developing insulin resistance, impaired glucose regulation and T2DM.
Importance and relevance
Despite well-established evidence that T2DM can be partially prevented through modifiable behaviour, the prevalence and incidence rates of T2DM continue to rise [8]. Potentially, there may be factors that prevent people from adjusting their modifiable behaviours towards decreasing their risk of developing T2DM. At present, there is no identified literature that categorizes facilitators and barriers for the implementation of modifiable risk behaviour and the development of T2DM. The factors that facilitate or inhibit people’s adoption of positive behaviours to prevent T2DM are not well understood. As such, it is imperative to perform an integrative review to evaluate existing studies and consolidate information about facilitators and barriers towards these factors to identify support strategies for adults at risk of T2DM. Therefore, the aim of this study is to apply an integrative review approach to identify the barriers to, and facilitators of, adopting a healthy lifestyle to prevent T2DM. Hence, the question that this integrative review seeks to answer is what the facilitators of are, and barriers to, modifiable behaviours that reduce the risk of developing T2DM in adulthood
Methods
Search strategy
To identify relevant literature concerning facilitators and barriers of modifiable behaviours, systematic and standardised searches using various search terms and phrases were performed. First, an advanced computerised search for relevant literature was performed across three databases: Cumulative Literature Index of Nursing and Allied Health Literature (CINAHL), MEDLINE and Sociological Abstracts. This approach proved efficient in rapid identification of literature, including study articles concerning the prevention of T2DM. The databases were relevant because of their renowned collections of publications and literature in the medical field. As this review focuses on barriers to, and facilitators of, individual behaviour, the Sociological Abstracts database, which contains behaviour and social science studies, was searched to include related studies. A hand searches of physical journals was also conducted to identify further relevant literature for inclusion in this integrative review.
Inclusion criteria
To review the most relevant literature, studies had to meet the following inclusion criteria:
peer-reviewed primary studies in the English language.
adult population at high risk of developing T2DM
the study had to identify barriers to, and facilitators of, modifiable behaviours for T2DM prevention and risk minimisation.
Exclusion criteria
This integrative study excluded reviews, guidelines, seminars and case studies without methodologies, procedures or scientific presentations of results. Second, the review excluded studies that focused on sample presence of diabetes or other health conditions (e.g., cancer and heart illness). This is because other conditions have different management plans and may not depend exclusively on modifiable behaviours. Third, any article that did not address clear barriers or facilitators of modifiable behaviours for T2DM risk prevention and minimisation were excluded.
Search outcome
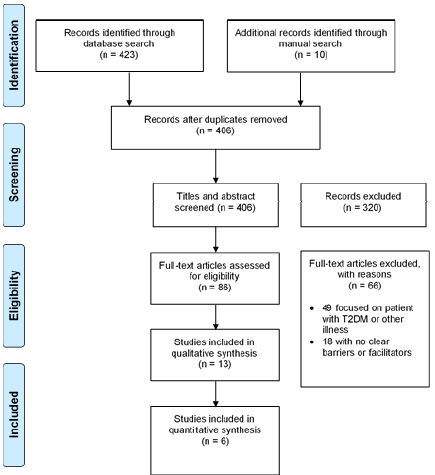
A total of 423 studies were mined from online databases and 10 were found through the manual search (Figure 1). Of those a total of 19 studies, met the inclusion criteria and appraisal quality and were selected for inclusion in this integrative review.
Figure 1: PRISMA flow diagram of search outcomes.
Quality appraisal
Critical appraisal is an important procedure in any integrative review to ensure the inclusion of high-quality studies [9]. For this reason, each individual study considered for this integrative review was investigated and critically appraised to ascertain its validity and reliability. This was done with a standardised critical appraisal tool based on Critical Appraisal Skills Programme (CASP) procedures. Corresponding quality assessment tools were used to account for the varying designs of the retrieved studies. These included four variants of the CASP and Centre for Evidence Based Management (CEBMa) checklists to tailor a quality appraisal to each study [9,10].
Findings
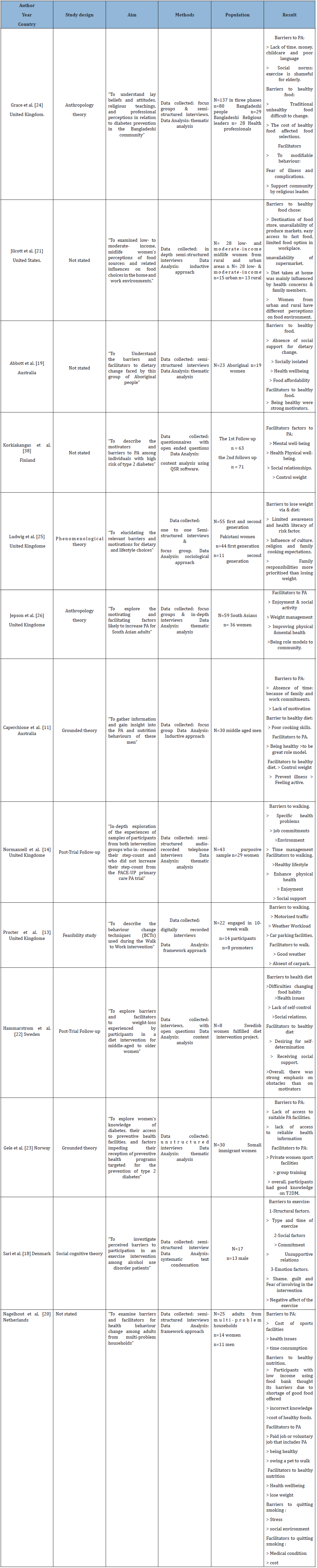
A total of 19 studies were included in this review to address the research question: what are the facilitators of, and barriers to, modifiable behaviours that reduce the risk of developing T2DM in adulthood? Included studies were undertaken in nine developed countries with a total of 1513 participants. The study characteristics of the included quantitative and qualitative studies have been identified in Tables 1 & 2 respectively.
Table 1: Description of the quantitative studies.

Table 2: Description of the qualitative studies.
The first stage of the review involved general classification of studies based on the major modifiable behaviours for reducing the risk of T2DM that they investigated. The studies were clustered into three major groups under the three dominant behaviours: PA, diet and smoking (Table 3). The second stage involved further clustering of the studies’ concepts, ideas, findings and results as either facilitators or barriers. Since most investigated both facilitators and barriers of the modifiable risk factors, a third step was simultaneously applied. This involved classification of the facilitators or barriers into either internal or external and produced four sub-categories under each of the modifiable behaviours (Table 3).
Table 3: Summary of the themes.
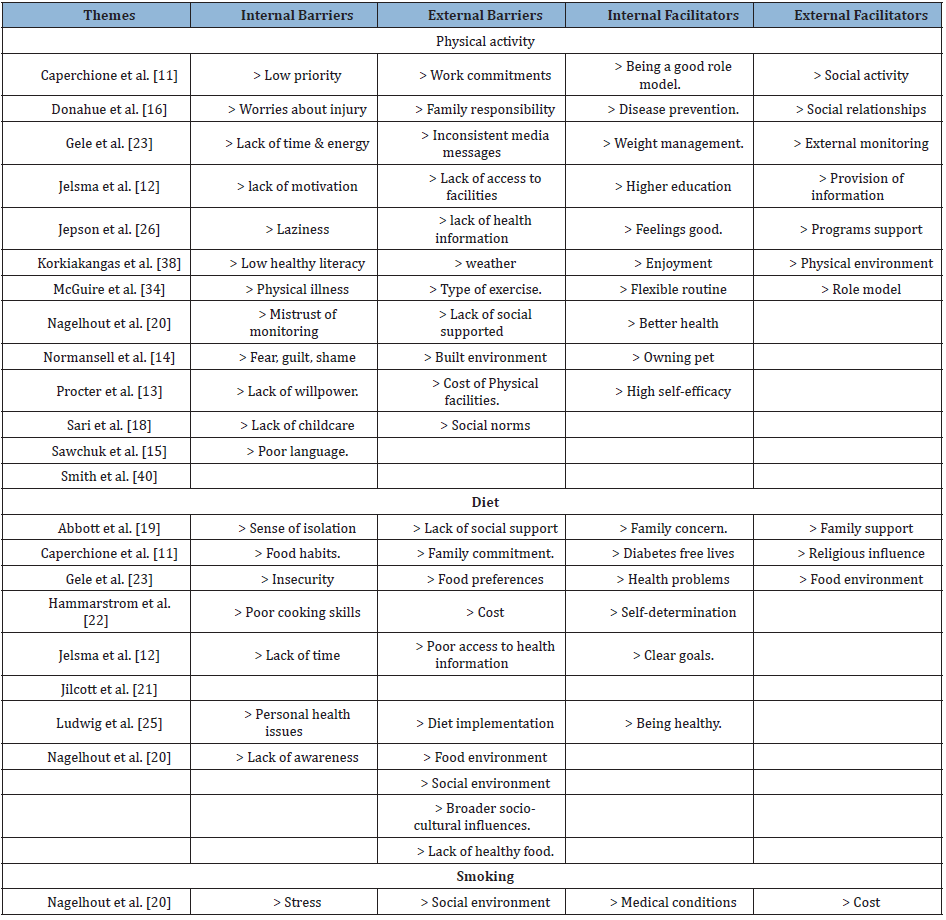
Physical activity
Internal facilitators: The review identified various internal facilitators of PA. These included high self-efficacy weight management, the need to be a good role model, disease prevention, physical and mental health and wellbeing improvement, effective self-monitoring strategies and dog ownership [11]. The study conducted by Smith et al. [12] identified self-efficacy, contributed to sufficient PA. The study also identified that self-efficacy enables effectively planning time and engaging in exercise. Two of the reviewed studies investigated education as an internal motivator for participation in PA. The qualitative study done by Caperchione et al. [11] confirmed that better knowledge was a positive determinant for PA [12-15]. A quantitative survey by Donahue et al. [16] found that 56% of the 258 participants, who attended 14 community centres in North Carolina, engaged in at least 150 minutes of PA weekly. Remarkably, those with higher education levels were more likely to exercise (OR 1.72; 95% CI 1.08-2.75). Therefore, it can be assumed then that education and adequate information enhanced comprehension of the health benefits of exercise.
External facilitators: The main external facilitator of PA was the enhancement of health information and social support. Jelsma et al. [12] identified that participants enhanced social support for engaging in PA after lifestyle counselling sessions with a health professional. A study by Procter et al. [13] investigated the feasibility of a 10-week Walk to Work behaviour change technique in 22 employees. It revealed that the main promoters of engagement in the intervention included additional support and encouragement. Effective support of PA programs was also identified as an important facilitator of exercise by Normansell et al. [14]. Their study revealed that supporting the participant by supplying adequate information on health importance of PA, enhancing self-monitoring, reviewing goals, providing feedback and using rewards all facilitated their engagement in exercise. Other studies, such as Sawchuk et al. [15], reported that American Indians were more likely to engage in PA if they were near interesting locations.
Internal barriers: The review identified internal barriers to physical activities, such as low self-efficacy, limited motivation, poor physical and mental wellbeing, limited time, low perceived benefit, emotional issues, inflexible routines and a lack of energy [16]. For instance, Smith et al. [17] identified that 26.5% of their 226 study participants had sedentary lifestyles, with only 36% having sufficient exercise, according to official recommendations. One of the main barriers was insufficient time (37.6%) for engaging in PA. The study identified that women who were under time pressure or tired had low self-efficacy. Other factors that hindered participants’ engagement in PA included worries about injury difficulties in allocating time [16]. Similarly, Normansell et al. [14] identified that inflexible routines and work commitments hindered proper PA. Hence, it can be surmised that interventions aimed at improving engagement in exercise should be flexible.
External barriers: External barriers were inconsistent media messages, inadequate knowledge, inaccessibility of tailored health information and training, cost implications, a lack of social support and environmental issues. A study by Caperchione et al [11] identified that middle-aged men do not exercise regularly because of inconsistent media messages about the benefits and best types of PA that they should engage in. The study also identified other external barriers such as increased work commitments and family responsibilities. In terms of social support, Kaiser et al. [18] identified that low social support was associated with low adherence to a healthy lifestyle, including physical exercise. Similarly, Sari et al. [19] revealed that the participants were impeded by social barriers in the form of as a requirement for accountability and unsupportive relatives. This illustrated that an individual’s social environment is essential for facilitating engagement in PA. In relation to environmental issues, Procter et al. [13] identified that barriers to the effective exercise intervention (Walk to Work) included wider contextual issues, such as economic climate and unprecedented weather, as well as organisational factors in the form of workload and availability of parking facilities.
Diet
Internal facilitators: Internal facilitators of healthy diet and nutrition practices included improved knowledge, disease prevention and self-determination [19]. A qualitative study by Abbott et al. [20] found that Aboriginal persons who had taken a cooking course at the Aboriginal Medical Service Western Sydney (2002–2007) had improved knowledge of nutrition and better cooking skills. Their implementation of the desired dietary changes was motivated by various internal factors, such as medical diagnoses, including both prediabetes and diabetes. Caperchione et al. [11] reinforced this idea by revealing that a need for disease prevention and remaining healthy were motivators of healthy eating. Nagelhout et al. [21] identified that having health conditions (such as diabetes) motivated the participants to eat healthily. This finding was also supported by Jilcott et al. [22], who found that health concerns motivated participants to engage in healthy eating and nutritional practices. Moreover, Abbott et al. [20] found that beyond self-concern, some study participants were motivated to implement dietary changes by their desire to influence their relatives to lead healthier lives and live without diabetes.
External facilitators: The review identified a number of external facilitators of healthy dietary practices, including proper support and religious influence [23]. For instance, Hammarstrom et al. [23] revealed that external facilitators included support from family, friends and the healthy diet project itself. Likewise, a prospective study by Kaiser et al. [18] identified low levels of social support as a barrier to adherence to healthy lifestyles and dietary habits. Thus, social support, including that of family and friends, was considered a great source of encouragement to continue engaging in healthy nutrition towards weight-loss. Program support was also important in facilitating healthy dietary practices. For instance, Jelsma et al. [12] revealed that programs-both face-to-face and telehealth-counselling sessions provided women with high BMIs and histories of GDM with enhanced self-efficacy towards healthy diets. This was also an important observation in a study by Hammarstrom et al. [23], which revealed that support from family members, friends and the intervention program enhanced healthy nutrition practices in women in Northern Sweden.
Internal barriers: The internal barriers to healthy dietary practices included a sense of isolation, family influence, personal struggles and poor cooking abilities [20] identified that Aboriginal persons were hindered by various internal barriers, such as a sense of isolation. Those who implemented the desired dietary practices were afraid to be isolated from family members who did not support the new diet. Abbott et al. [20] also identified other personal factors including poor dental care and psychological illness in the form of depression. These likely incapacitated individuals physically and mentally, respectively, and rendered them unable to implement the desired dietary changes. A study by Hammarstrom et al. [23] also identified that middle-aged women faced physical struggles that hindered their effective participation in healthy nutrition interventions. These physical struggles included difficulties in altering food habits and patterns, inadequate self-control and insecurities. Caperchione et al. [11] identified poor cooking skills and abilities as a further internal barrier to healthy eating. Jelsma et al. [12] also mentioned prohibition by a lack of time, easy availability of unnatural food at home and desires for pre-packaged food such as sweets.
External barriers: The review identified various external barriers including lack of family support, unsuitable environments, high food costs, work commitments and cultural practices [11,12,20,22,24-26]. Abbott et al. [20] identified that Aboriginal persons struggled to implement dietary changes and were impeded by a lack of family support for meal alterations and different generational food preferences. Thus, the individuals were forced to compromise according to familial dietary preferences and needs [20].
The environment was also identified as a major factor impeding participants’ engagement in healthy nutrition. A qualitative study by Jilcott et al. [22] involving 28 women of both low and moderate income (aged 37-67 years) from rural and urban areas found that the participants’ perceptions of their food environment influenced their diet choices. Women in rural settings did not have adequately healthy diets compared to those in urban areas because of the existence of fewer supermarkets and produce stands in rural areas [22-25]. In terms of social environment, Jilcott et al. [22] revealed that women’s food choices were greatly influenced by co-workers and the surrounding food environment, including limited availability of healthier food choices. Hence, it can be deduced that the environment affected food accessibility and thus, individuals’ eating patterns.
Smoking
Internal facilitators: The only internal facilitators of stopping smoking were medical conditions [20]. These included both the fear of developing a disease and actual diagnosis, specifically with such as diabetes, cardiovascular disease and COPD. Some participants may also have quit smoking because of the perceived health risk of smoking itself. Nagelhout et al. [21] argued that the observed phenomenon can be explained by a health belief model, where individuals tend to engage in activities that may reduce their perceived health risk. The study also identified some individuals who quit smoking because they were curious to experience what quitting was like.
External facilitators: Nagelhout et al. [21] also reported that cost was a major factor that motivated the participants to quit smoking. This included both the high cost of cigarettes and the fact that some participants perceived smoking as an economic problem and a waste of money and resources. A study by Grace et al. [25] identified that religious leaders were essential in providing considerable support of healthy behaviours to prevent diabetes. This included Islamic teachings on the cessation of unhealthy behaviours, such as smoking and drinking alcohol.
Internal barriers: Only Nagelhout et al. [21] identified an internal barrier to cessation of smoking stress. The participants utilised smoking as a means of relieving stress, which also contributed to a return smoking after quitting. The researchers argued that smoking was promoted as a negative adaptation to stress in the form of household, family and social issues including limited income.
External barriers: One of the main barriers to quitting smoking was the social environment. According to Nagelhout et al. [21], participants who had quite reported that they returned to smoking because of friends who smoked. Similarly, Grace et al. [25] revealed that cultural influences, including the desire to comply with cultural norms, such as drinking and smoking, increases an individual’s tendency to engage in these unhealthy practices.
Discussion
Facilitators of modifiable behaviours
Personal factors: This integrative review identified various personal factors that facilitate behaviour modification to reduce the adult risk of developing T2DM. The main influencer is motivation: a reason that guides or prompts an individual to act or behave in a particular way [13]. The studies reviewed identified various factors that motivate adults to exercise, eat a healthy diet or stop smoking and found that individuals who had high level of motivation engaged adequately in PA, consumed healthy diets and avoided risky behaviours, such as smoking [14,27]. Similar studies indicated that this is the same in positively motivated individuals [5]. From a theoretical perspective, the self-determination theory states that motivation elicits individuals’ internal resources such as rational thinking and positive decision-making, which improves their abilities and capacities for an action or behaviour [28].
Social factors: The reviewed studies identified that adults who have adequate social support through supportive relationships (including family support in the form of verbal encouragement and support from friends) engage in PA, practice healthy nutritional habits and avoid risky unhealthy behaviours like smoking [14,23]. Additionally, this review revealed that adults who derive adequate support from healthcare systems and prevention programs have a positive tendency to effectively participating in healthy interventions [23]. According to Grace et al. [25] enhancement and facilitation of social support can facilitate healthy behaviour modification, which is integral in disease preventions. This is essentially because social support enhances emotional, tangible, informational and companionship support, which increases an individual’s capacity for decision-making, enhances knowledge and awareness and increases acquisition and accessibility of resources that enhance behaviour modification [29].
Informational factors: Information is a powerful tool to enhance behaviour modification and the studies reviewed showed that individuals who have adequate information concerning T2DM effectively engage in PA, healthy diets and cessation of smoking [22,24]. The studies also identified that individuals who have adequate information concerning the need for behavioural change, diabetes prevention and management strategies and the benefits of modifiable behaviours tend to embrace positive lifestyles by exercising and eating healthy diets [30,31]. Thus, to facilitate modifiable behaviours that reduce the risk of T2DM, the focus should be on enhancing individuals’ knowledge and awareness through health education, health campaigns and the provision of adequate informational resources to guide them.
Barriers to modifiable behaviours
Personal factors: This review has revealed the numerous personal factors that impede modifiable behaviours to prevent T2DM. These can be largely classified as health issues and self-efficacy. For instance, some studies showed that adults diagnosed with health issues, such as depression, arthrosis and cardiovascular conditions, have low propensity for PA [20,23]. These health issues may limit the person’s physical ability to exercise and introduce nutritional variations [32]. According to the studies reviewed, self-efficacy issues may include a lack of motivation and willpower, inability to find time, difficulties in changing behaviour and poor prioritisation of healthy habits [11,16]. Additional studies have identified limited self-efficacy as prohibitive of behavioural change to prevent chronic diseases [5]. For instance, Amireault et al. [33] found that individuals with low self-efficacy (limited personal motivation and improper prioritisation) do not effectively engage in PA programs and interventions strategies.
Social factors: The review identified social support systems as paramount in behaviour modification as they may determine the level of assistance an individual requires to embrace healthy practices [18]. Leung et al. [29] revealed that limited family support is a significant barrier to healthy nutrition and exercise. Similarly, Ludwig et al. [26] reported that most family members of individuals at risk of developing diabetes have difficulties in adjusting to new diet recommendations to managing diabetes; hence, they provide limited support to the affected family member. Thus, dietary changes may be challenging in an unsupportive family environment. Other studies identified further prohibitive social factors in the form of cultural and religious practices [19,20,25,26]. These largely operate in cases of dietary restrictions [34] and may thwart individuals’ attempts to practice healthy nutrition.
Informational factors: The main informational factor that hinders adults’ engagement in modifiable behaviours that prevent T2DM is a lack of knowledge or awareness of their benefits in preventing and reducing the risk of T2DM [11,35]. This finding has been confirmed by other studies. For instance, Enjezab et al. [30] revealed that improved awareness of the importance of exercise results in increased participation in healthy physical activities. Gele et al. [24] stated that participants who engaged in physical activities and healthy dietary practices had greater knowledge and increased awareness. Arguably, adequate information and knowledge enhance an individual’s decision-making capacity and self-efficacy, which consequently leads to increased healthy behaviours, such as PA, proper nutrition and diet.
Environmental factors: This review found that an individual’s environment can impede their engagement in modifiable behaviours. Environmental impediments to PA and healthy nutrition include unprecedented wet weather, climate change, the built environment and rural settings [13,14]. These findings are supported by other studies. For instance, Jilcott et al. [22] identified that individuals living in rural settings do not practice healthy nutrition and have poor diets compared to those in urban settings. Similarly, Dyck et al. [36] revealed that individuals in rural populations are also unable to effectively participate in physical exercise and activity compared to those who live in urban areas. Arguably, these differences are due to differing availability and accessibility of food and amenities for physical activities in the different settings [22]. Therefore, it can be deduced that those in areas with poor availability of a variety of food and physical exercise facilities, such as in rural areas, may not have adequate healthy nutrition or engage in proper PA. Hence, they may be at increased risk of developing T2DM.
Recommendations
This study recommends that facilitators of modifiable behaviours be enhanced through health education self-efficacy and social environment. First, it is already widely established that education and counselling are effective approaches to enhance facilitators of modifiable behaviours of preventing T2DM [14]. A multi-sectorial partnership between government bodies including health & education may enhance the delivery of program about PA, healthy diet, smoking awareness [37]. Second, this review recommends enhancement of self-efficacy to improve adult engagement in modifiable behaviours that prevent T2DM. Chung- Yan [38] suggested that this can be achieved by providing examples of other individuals who have benefited from PA, heathy nutrition and cessation of smoking. These individuals can act as models in encouraging others to have strong belief in their own ability to change. Last, social environment plays an integral part in facilitating or barring individuals’ engagement in PA, healthy nutrition and not smoking [22]. Thus, to aid participation in these activities, initiatives should improve the social environment by enhancing family and social support systems, improving social networks and increasing accessibility to social resources, such as healthcare facilities [29]. This can be achieved by embracing social marketing in healthcare, formulation of important policies that promote community-based interventions and establishment of social infrastructure [25].
Limitations
This integrative review has identified facilitators and barriers of modifiable behaviours that prevent the development of T2DM in adulthood. However, there are some limitations. First, the review has identified the factors affecting PA and diet but has not exhaustively investigated other factors such as cessation of smoking and alcohol consumption. This is because only a single study concerned smoking, making it difficult to adequately addressed. The second limitation is that the population of focus was adults; hence the findings may not be applicable across all population’s groups or to children. Also, T2DM tend to be diagnosed in adulthood and modifiable factors such as PA, unhealthy eating and tobacco smoking may have been learned behaviours from childhood. Lastly, despite well-established evidence that T2DM prevalence rate highly increasing in middle- and low-income countries [39,40], the review only discovered studies from developed countries.
Conclusion
This integrative review has identified numerous facilitators and barriers of modifiable behaviours that reduce the risk of T2DM development (exercise, healthy nutrition and not smoking). They include both internal and external factors: personal factors, emotional issues, and health problems as well as social, environmental and informational factors. The most important finding here is that these factors are interlinked and have effect each other through synergistic and exclusive interactions. Indeed, the presence or absence of one factor may reinforce or diminish the effects of another. Therefore, any strategy aimed at enhancing the facilitators of modifiable behaviours that prevent T2DM should be integrated and comprehensive in nature and tailored to target the unique needs and concerns of an individual.
References
- International Diabetes Federation (2013) IDF diabetes atlas. In: (8th edn), Brussels, Belgium.
- World Health Organization (2016) Global report on diabetes.
- Gregg EW, Sattar N, Ali MK (2016) The changing face of diabetes complications. Lancet Diabetes & Endocrinology 4(6): 537-547.
- Wennehorst K, Mildenstein K, Saliger B, Tigges C, Diehl H, et al. (2016) A comprehensive lifestyle intervention to prevent type 2 diabetes and 50 cardiovascular diseases: The german CHIP trial. Prevention Science 17(3): 386-397.
- Noble N, Paul C, Turon H, Oldmeadow C (2015) Which modifiable health risk behaviors are related? A systematic review of the clustering of smoking, nutrition, alcohol and physical activity (‘SNAP’) health risk factors. Preventive Medicine 81: 16-41.
- Spruijt MD, Reilly GA, Cook L, Page KA, Quinn C (2014) Behavioral contributions to the pathogenesis of type 2 diabetes. Current Diabetes Reports 14(4): 475.
- Knowler WC, Barrett E, Fowler SE, Hamman RF, Lachin JM, et al. (2002) Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. The New England Journal of Medicine 346(6): 393-403.
- Alouki K, Delisle H, Bermúdez TC, Johri M (2016) Lifestyle interventions to prevent type 2 diabetes: A systematic review of economic evaluation studies. Journal of Diabetes Research 2: 1-14.
- Elwood JM (2017) Critical appraisal of epidemiological studies and clinical trials (4th), Oxford: Oxford University Press, New York, USA, 67(7): 583-584.
- University of South Australia (2018) Critical appraisal tools, Austaralia.
- Caperchione CM, Vandelanotte C, Kolt GS, Duncan M, Ellison M, et al. (2012) What a man wants: Understanding the challenges and motivations to physical activity participation and healthy eating in middle-aged Australian men. American Journal of Mens Health 6(6): 453-461.
- Jelsma J, Poppel M, Smith B, Cinnadaio N, Bauman A, et al. (2018) Changing psychosocial determinants of physical activity and diet in women with a history of gestational diabetes mellitus. Diabetes/Metabolism Research and Reviews 34(1).
- Procter S, Mutrie N, Davis A, Audrey S (2014) Views and experiences of behavior change techniques to encourage walking to work: A qualitative study. BMC Public Health 14: 1-13.
- Normansell R, Smith J, Victor C, Cook D, Kerry S, et al. (2014) Numbers are not the whole story: A qualitative exploration of barriers and facilitators to increased physical activity in a primary care-based walking intervention. BMC Public Health 14: 1272.
- Sawchuk C, Russo J, Bogart A, Charles S, Goldberg J, et al. (2011) Barriers and facilitators to walking and physical activity among American Indian elders. Preventing Chronic Disease 8(3): A63.
- Donahue KE, Mielenz TJ, Sloane PD, Callahan LF, Devellis RF (2006) Identifying supports and barriers to physical activity in patients at risk for diabetes. Preventing Chronic Disease 3(4): A119.
- Smith BJ, Cheung NW, Bauman AE, Zehle K, Lean M (2005) Postpartum physical activity and related psychosocial factors among women with recent gestational diabetes mellitus. Diabetes Care 28(11): 2650-2654.
- Kaiser B, Jeannot E, Razurel C (2016) Determinants of health behaviors after gestational diabetes mellitus: A prospective cohort study in Geneva. Journal of Midwifery & Women's Health 61(5): 571-577.
- Sari S, Muller AE, Roessler KK (2017) Exercising alcohol patients don't lack motivation but struggle with structures, emotions and social context-a qualitative dropout study. BMC Family Practice 18: 45.
- Abbott P, Davison J, Moore L, Rubinstein R, Abbott P, et al. (2010) Barriers and enhancers to dietary behaviour change for aboriginal people attending a diabetes cooking course. Health Promotion Journal of Australia 21(1): 33-38.
- Nagelhout G, Hogeling L, Spruijt R, Postma N, Vries dH (2017) Barriers and facilitators for health behavior change among adults from multi-problem households: a qualitative study. International Journal of Environmental Research and Public Health 14(10): 1229.
- Jilcott SB, Laraia BA, Evenson KR, Ammerman AS (2009) Perceptions of the community food environment and related influences on food choice among midlife women residing in rural and urban areas: a qualitative analysis. Women & Health 49(2-3): 164-180.
- Hammarstrom A, Wiklund A, Lindahl B, Larsson C, Ahlgren C (2014) Experiences of barriers and facilitators to weight-loss in a diet intervention-a qualitative study of women in Northern Sweden. BMC Women's Health 14: 1-10.
- Gele AA, Torheim LE, Pettersen KS, Kumar B (2015) Beyond culture and language: Access to diabetes preventive health services among Somali women in Norway. Journal of Diabetes Research, pp. 1-9.
- Grace C, Begum R, Subhani S, Kopelman P, Greenhalgh T (2008) Prevention of type 2 diabetes in British Bangladeshis: qualitative study of community, religious, and professional perspectives. BMJ 337: a1931.
- Ludwig AF, Cox P, Ellahi B (2011) Social and cultural construction of obesity among Pakistani Muslim women in North West England. Public Health Nutrition 14(10): 1842-1850.
- Jepson R, Harris FM, Bowes A, Robertson R, Avan G, et al. (2012) Physical activity in South Asians: An in-depth qualitative study to explore motivations and facilitators. PLOS ONE 7(10): e45333.
- Ryan RM, Deci EL (2000) Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. American Psychologist 55(1): 68-78.
- Leung J, Pachana NA, McLaughlin D (2014) Social support and health-related quality of life in women with breast cancer: A longitudinal study. Psycho-oncology 23(9): 1014-1020.
- Enjezab B, Farajzadegan Z, Taleghani F, Aflatoonian A (2012) Internal motivations and barriers effective on the healthy lifestyle of middle-aged women: A qualitative approach. Iranian Journal of Nursing and Midwifery Research 17(5): 390-398.
- Shi H, Nakamura K, Takano T (2004) Health values and health-information-seeking in relation to positive change of health practice among middle-aged urban men. Preventive Medicine 39(6): 1164-1171.
- Groth SW, David T (2008) New mothers views of weight and exercise. MCN, the American Journal of Maternal/Child Nursing 33(6): 364-370.
- Amireault S, Godin G, Vézinaim L (2013) Determinants of physical activity maintenance: A systematic review and meta-analyses. Health Psychology Review 7(1): 55-91.
- Pharr JR, Francis CD, Terry C, Clark MC (2014) Culture, caregiving, and health: Exploring the influence of culture on family caregiver experiences. ISRN Public Health, pp. 1-8.
- McGuire A, Seib C, Anderson D (2016) Factors predicting barriers to exercise in midlife Australian women. Maturitas 87: 61-66.
- Dyck DV, Cardon G, Deforche B, Bourdeaudhuij D (2011) Urban-rural differences in physical activity in Belgian adults and the importance of psychosocial factors. Journal of Urban Health 88(1): 154-167.
- Willis C, Greene J, Riley B (2017) Understanding and improving multi-sectoral partnerships for chronic disease prevention: Blending conceptual and practical insights. Evidence & Policy: A Journal of Research, Debate and Practice 13(4): 623-645.
- Chung YC (2014) Psychological determinants of exercise behavior of nursing students. Contemporary Nurse 49(1): 60-67.
- Korkiakangas E, Taanila AM, Keinanen KS (2011) Motivation to physical activity among adults with high risk of type 2 diabetes who participated in the Oulu sub study of the Finnish diabetes prevention study. Health & Social Care in the Community 19(1): 15-22.
- Beanlands H, Horsburgh ME, Fox S, Howe A, Locking H, et al. (2005) Caregiving by family and friends of adults receiving dialysis. Nephrology Nursing Journal: Journal of the American Nephrology Nurses Association 32(6): 621-631.
© 2020 Hadwan Mibrad Aldahmashi RN. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






