- Submissions

Full Text
COJ Nursing & Healthcare
Recall of Casualty Care During the Gulf War (1991) by British Non-regular Services’ Health Professional Veterans
Deidre Wild*
Senior Research Fellow (Hon), Faculty of Health and Life Sciences, UK
*Corresponding author: Deidre Wild, Senior Research Fellow (Hon), Faculty of Health and Life Sciences, UK
Submission: March 25, 2019; Published: June 13, 2019

ISSN: 2577-2007Volume5 Issue2
Abstract
In November 1990, in response to the size of the Iraqi conventional (Ballistic) and unconventional (biological and chemical) weaponry threat in the Middle East, and the potential for a high number of casualties, the British Government acknowledged an insufficient number of regular military medical personnel available for war-service. This resulted in a request to part-time military Voluntary Services (VS) health professionals (doctors, nurses, and other professions allied to medicine) to volunteer [1]. The number responding was too small, hence ex-regular Reservists were mandatorily called up. The present study recruited 95 of these VS and Reserve health professional veterans to complete an extensive postal questionnaire some six months after their return about their Gulf War (GW) experiences. These included casualty care in field hospitals in the desert and in general hospitals sited near Saudi cities such as Riyadh. The data were both quantitative and qualitative and enabled a voice to be given to a generally under-researched group of British GW veterans.
Keywords: Gulf War; Allied/Enemy casualties; Care; Non-regular services’ health professional veterans
Acronyms: UK: United Kingdom; VS: Voluntary Services; GW: Gulf War; TA: Territorial Army; HPV: Health Professional Veteran; SPSS: Statistical Package for the Social Sciences; ECG: Electrocardiogram; US: United States
Literature Review
Before the GW land offensive began, Wild & Brooking [2] highlighted the importance of the impending GW as a new casualty care source of learning for civilian nurses both from stand-by for war casualties in UK (United Kingdom) hospitals and for those who volunteered or were called-up, to active military service in the war-zone in Saudi Arabia [2]. Following the GW, some operational challenges and deficits observed in one British field hospital were identified which could have acted as ethical stressors during deployment. Deficits included, the absence of defibrillators and ECG monitors; The limited supply of local anaesthetics; The absence of an intensive care facility (Although essential equipment for respiratory support for several patients at one time was provide, and the poor positioning and tipping of the stretcher-topped field operating table. The effects of extremes of temperature, sand, and flooding upon tented operating facilities were also reported and in addition, it was noted that only half of the medical officers working in the resuscitation department of the field hospital were trained anaesthetists [3,4].
The experience of a Canadian field hospital contingency working with a British field hospital provided critical insights into the issues facing the multinational medical collaboration in the GW [5]. These comprised difficulties with the calculation of personnel requirements within a potentially fast changing scenario; different approaches to the timing of wound debridement in the treatment of burns, difficulty in making changes to treatment protocols when more than one nation is working side by side and subject to separate protocols, and the use of different equipment by some Coalition nations. Although none of the above literature [3-5] report that these challenges were overly problematic in the low casualty circumstances of the GW, all of the authors conclude that had there been a more prolonged and intense land war, or one that was complicated by unconventional weaponry agents, the situation could have been much more problematic.
Smith [6] an American Chief Nurse provides a concise description of the development and organisational requirements of the American hospital facility in the GW [6]. She gives the main challenges as: the adaptation of peacetime documentation and communication systems to the War’s requirements, and the educating of staff to them that was not fully achieved by the time they arrived in the field. Difficulties also arose in getting medical equipment and personnel arriving in Saudi Arabia in January and February of 1991 (the time period in which the present study’s HPV sample arrived) to assigned locations and some ex Vietnam-era mobile hospital units and equipment proved ill-suited to the desert environment.
In contrast, other authors focus their accounts of the GW upon the efficacy of the casualty evacuation system. Although the speed of the Coalition forces victory under-utilised the UK casualty evacuation system, many important lessons were learned by regular and auxiliary forces in communications, organisation, and life-saving trauma skills [7]. However, a three times higher median evacuation-time after the commencement of the land offensive than before it, emphasises the need for more appropriate triage, transport and communication facilities to optimise resources [8].
Some authors suggest that high and consistent exposure to stress can lead to burnout [9]. In a review article written before the GW, Brooking [10] observes that in treating battle casualties, the Army Medical Service is party more to war’s failure in terms of human vulnerability, than its military and political successes. She notes that the occupational stressors found in civilian medical and nursing professionals could arise under combat conditions, in particular for those in the Territorial Army (TA) VS and in addition to the other stressors that affect all personnel in a war-zone.
The experiences of American nurse volunteers in the Vietnam War were qualitatively contrasted with those who had accompanied Florence Nightingale to Scutari in the Crimean War over a century earlier [11]. Similar stressors for both Wars were identified as: the extent of human suffering; the constant flow of military and civilian casualties; unfamiliar diseases; lack of supplies; deplorable conditions in some hospitals, and the effects of climate on the working environment. The adverse stress effects from both wars upon the nurses’ post war psychological health were similarly attributed to their experience of death and repressed bereavement emotions during the respective conflicts.
Brooking [10] also draws attention to war-related ethical issues for TA VS nurses and doctors as a further source of stress that sets them apart from other support and combatant military personnel. For, contrary to civilian triage where treating those with the greatest need is undertaken first, the military’s mass casualty triage system when under pressure would treat first the casualties who are the most likely to have a good survival potential, and who require less life-saving surgical time [12]. The military casualty triage system (Also in operation in the GW), is described as a major source of stress in a qualitative study of nurse veterans of the Vietnam War [13].
Methodology
Design
A longitudinal mixed method design was employed using postal questionnaires to collect data at three time points, each six months apart, with the first commencing 6 months after the end of the war (September 1991) Data for this article was collected in this first questionnaire.
Method and materials
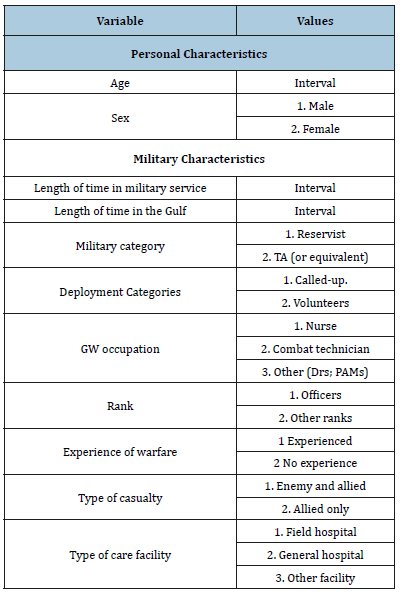
The first questionnaire was developed from literature concerning wars preceding the GW; contemporary reports on aspects of the GW [14] and testimonies from the Pilot Study’s 7 HPV participants. The draft pool of dichotomous and scale items was generated and content and format were suggested and amended with input from the Pilot Study’s HPVs who also contributed to the main study. Both open and closed questions were included, the former enabling added depth to the exploratory approach. In this way, the qualitative and quantitative methods enhanced understanding more so than either method on its own [15]. The variables of interest for this article are given in Table 1:
Table 1:The article’s variables and values of interest.
Participants and recruitment procedure
The first of three stages of the recruitment of the study’s participants was opportunistic. One HPV Reservist nurse (a work colleague known to the author) held a personal contact list of 74 HPVs (including herself) who had returned together by air to the UK in March 1991 following the end of the GW. As it would have been unethical for the author to have had direct access to those on the address list, the colleague agreed to act as an intermediary by forwarding a letter to them from the author with details of the study and a pre-paid postal envelope for the return of their contact details and a completed consent form. In the event, 57 (47 ex-regular Reservists and 10 VS TA) of the 74 HPVs gave their agreement to participate in the study.
In the second recruitment stage, a purposeful increase of the VS TA group to that of Stage 1 Reservists and in similar health professional roles was made. This was achieved by asking the 10 consenting VS TA participants from Stage 1, to act as ‘Intermediaries’ in making a ‘Snowball’ access to similar other GW veterans within their own or other TA units. To facilitate this, each of them was supplied with 5 introductory letters (n=50) with pre-paid return contact slips for direct return to the author. As a result, a further 33 TA HPVs agreed to participate in the study raising the total for the VS TA to 43. Although there was no way of knowing if all of the 50 letters provided, had been issued, the percentage estimate for those giving consent (post receipt of study information) to join the study, was at a high level (66%).
Finally, in a third recruitment stage, a GW veteran Welfare Officer in the Order of St John of Jerusalem, who having heard of the study, made direct contact with the author to seek inclusion for the 10 Welfare Officers who had been volunteers in the GW. Following the issue of 10 introductory letters with return, contact and consent slips to the organisation’s initial contact for distribution, 5 (50%) of these veterans agreed to become participants.
Nature of the inquiry
We sought to explore how the HPVs viewed their experience of casualty care when given in different locations and facilities (field and general hospitals) and with different casualty groups (Iraqi prisoners of war and allied casualties).
Ethical considerations
Although the study preceded the formal ethical requirements of today’s research, the general principles of doing no harm; securing informed consent; the acceptance of autonomy over compliance, and respect for rights to privacy, anonymity and confidentiality [16] were upheld. Authoritative military and academic advice were taken throughout the study to avoid potentially sensitive issues. All information forwarded to the HPVs cautioned them against breaching the Official Secrets Act. The data were held securely and in accordance with the Data Protection Act, 1987 and its update in 1998.
Analysis
Quantitative dichotomous data were analysed using the Statistical Package for the Social Sciences (SPSS) Version 22. Logistic regression with a forward stepwise Wald was employed to test whether particular personal, professional and/or military characteristics had significant ‘Odds’ likelihoods of occurrence. Qualitative data in the form of the HPVs’ comments were subjected to thematic content analysis and were examined first by two researchers working independently to identify key words or phrases. These were then categorised as labels to capture as closely as possible the meaning of the HPVs’ original words or phrases [17]. The two researchers then made cross comparisons to reach consensus. In some instances, the qualitative data were coded into new variables to permit the use of descriptive statistics.
Result
Sample return-rate for the first questionnaire
The total of 134 contact letters issued across the three recruitment stages resulted in 95 consenting HPVs. An estimated minimum overall response rate of 71% was obtained from the three stages of recruitment. At the time of recruitment to the study, the numbers of volunteer TA and Reserve personnel deployed to the GW had not been reported in the public domain. However, figures given some years after the GW suggest that the 95 HPVs in the participant sample represented some 1 in 100 of the total population of Reserve and TA (or similar voluntary military organisation) deployed personnel [18].
When the data for the two categories for type of casualty involvement (1. Enemy and allied casualties 2. Allied only) were compared with the HPV sample’s characteristics using t test and Chi Square as preliminary analysis (Table 2) no significant difference was observed with age (t=0.56, df=80.98, p>0.05), or length of military service (t=1.17, df=72.33, p>0.05), sex, marital status, parenthood, military category, deployment category or rank (p>0.05, Respectively). However, the comparisons of type of casualty involvement with GW occupation (χ2=14.5, df=1, p>0.01), previous experience of warfare (χ2=8.46, df=1, p>0.01) and with GW location facility (χ2=17.92, df=1, p>0.01) were all significant Table 2.
Table 2:Preliminary Analysis for Type of Casualty Involvement with Sample Characteristics (Chi Square).

*Excluded or missing values **Fishers Exact Test
Caution was applied to the above findings as these significant relationships could be false positives or negatives. To overcome these possibilities, Logistic Regression with a forward stepwise Wald statistic was employed to gain more reliable ‘Odds Ratio’ outcomes. As shown in Table 3., the output from the Logistic Regression model using sample characteristics as Independent Variables (IV) with the two values for type of casualty involvement as a Dependent variable identified age (younger B=-0.10, r=-0.23, p>0.001), previous experience of warfare (experienced B=2.12, r=0.23, p>0.01) and GW location facility (field hospital B=2.35, r=0.32, p>0.001) as the best independent significant predictors of involvement with enemy/allied casualties but GW occupation did not attain its former preliminary significance (p>0.05) Table 3.
Table 3:Significant LR analysis between Type of Casualty with Sample Characteristics (N=68)*
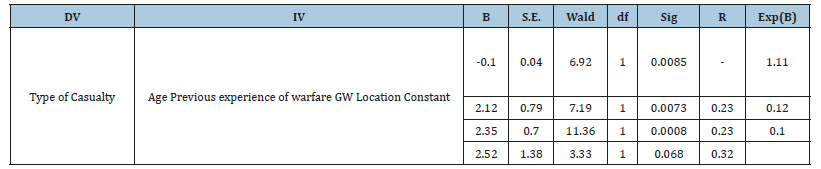
*27missing values.
Analysis of qualitative data related to type of casualty care
The differences between working in a general hospital and in a field hospital was marked with both locations having unique stressors. The HPVs in general hospitals complained about shared accommodation with other military personnel not to their liking and the curtailment of freedom of movement of female troops that was imposed as a mark of respect towards the Islamic culture of Saudi Arabia.
‘Having to live with other girls within a house where I couldn’t change the environment to suit my needs. I did have a room to myself but I hadn’t chosen my companions and they were not all my cup of tea.’ (Female TA volunteer, junior officer nurse, support general hospital location). ‘The lack of freedom. We were not allowed to go out and it was like being in an open prison. (Female Welfare Officer, volunteer, support general hospital location).
Further criticisms included the shortage and age of equipment and organisational deficits in terms of calculating skill mix: ‘No proper equipment or very old and archaic. Staff mix unrealistic re: knowledge. Unrealistic as to aims and objectives - total fairyland!’ (Female Reservist called up, junior officer nurse, support general hospital location). In contrast, those in desert-based field hospitals, struggled with the basic and unsavoury sanitary conditions within tented accommodation which presented daily challenges, often described with a sense of humour:
A. ‘Defecating into black bags mounted in small, hot wooden kiosks filled with extremely active flies!’ (Male Reservist called-up senior other rank physiotherapist, field location)
B. ‘Lack of privacy. Lack of comfortable sanitary conditions - toilets showers etc. Shortage of water. Boring diet.’ (Female Reservist called-up, junior officer nurse, field location)
Differing professional reactions to wartime casualty care according to their location in the casualty evacuation system were evident in some HPVs’ comments. HPVs working in field locations tended to adopted an impersonal approach towards casualties possibly because the focus was upon treating injuries so that the person could be evacuated or returned to the front-line in the shortest time possible:
A. ‘With war casualties there is a tendency to accept the level of injuries as normal and this tends to produce the effect that concern for the injured is not as sensitive in caring as it should be, or as it would be in civilian life.’ (Male TA volunteer, senior other rank nurse, field hospital).
B. In contrast, the HPVs in support locations described a greater level of personal involvement with their casualties, most likely because they had more time to get to know them as persons rather than as ‘Conditions’ during their protracted recovery period
C. ‘You become closer to them as they have no relatives or friends to talk to. They used to tell you what had happened to them and some of the horrific sights they had seen. A lot of them had had a long uncomfortable journey back to us. They hadn’t seen women for a long time so loved to chat with you. (Female reservist volunteer, junior officer nurse-support hospital).
In the first account of casualty care below, the relationship between the circumstances of injury, stress and the military culture were depicted in addition to survivor guilt from casualties of higher rank with the burden of responsibility for the loss of lives or injury to their men. Whereas in the second comment there is a sense of forlornness towards all aspects of life in a field hospital.
‘The circumstances of injury give rise to exceptionally high levels of stress for the casualty, especially if he had lost colleagues (or is the only survivor). As the rank of the patient rose, so did his feelings of responsibility for his men who were killed or injured. I found I spent as much time counselling as I did physically treating them.’ (Male reservist called-up, senior other rank, physiotherapistsupport facility)
‘The wounds, the enemy, the conditions of work, the stress of all of us.’ (Female reservist called-up, junior officer nurse - field hospital). The 44 HPVs involved with enemy/allied casualties were asked to describe if they had any personal or professional concerns arising from their casualty experience. Of these, 14 (32%) described personal, Organisational and ethical concerns. The remaining 30 (68%) said that they had no concerns. Three themes emerged from their comments. In the first, 4 HPVs felt fear and mistrust between themselves and the Iraqi casualties:
‘A bit difficult at times. They [Iraqis] thought I was going to kill them. I thought they were going to kill me.’ (Female TA volunteer, senior officer nurse - field hospital).
In the second theme, 4 HPVs depicted tension and resentment arising from the care given to allied and enemy casualties within the same facility:
‘At first it was difficult because we had both enemy and allied casualties on the ward together which made things a little tense, with the allied casualties being resentful of the care we gave to the enemy. We also had armed guards which brought home to you that these people were dangerous.’ (Female reservist called-up, junior officer nurse-field hospital).
Finally, 6 HPVs described ethical issues associated with a perceived inequality of care-giving to enemy casualties and in these circumstances all but two of the HPVs placed emphasis upon this being the observed practice of ‘others’ as opposed to their own practice:
‘I felt that my role was as a medic to care for people - but a number of staff didn’t want to nurse the enemy and it was difficult to keep them to nurse allied casualties only, due to the staff:
casualty ratio.’ (Female reservist called-up, junior officer nurse - field hospital)
A. ‘I thought that certain military personnel mistreated enemy casualties.’ (Female TA volunteer, senior other rank nursefield hospital).
B. ‘I treated each soldier the same. Unfortunately some others did not.’ (Male reservist volunteer, senior other rank nurse - field hospital).
The above comments suggest that some form of practice shortfall occurred during deployment in an unknown number of health professionals with Iraqi prisoners in field hospitals, but the true extent or nature of this cannot be ascertained from these data. However, where such malpractice arose this was a source of tension between troops. For, of 28 HPVs identified with difficult relationships with other military, 19 (67%) cared for enemy and allied casualties in comparison with 9 (33%) of those caring for allied-only casualties. These differences just achieved significance (χ2=3.738, df=1, p=0.05).
Limitations
The participants were neither a representative sample nor was it possible to match HPVs with controls, thus generalisation is not possible. Nevertheless, it is believed that the richness of the combined findings from qualitative and quantitative sources presents a reliable picture of this group of HPVs’ war-related experiences and by inference they could be regarded as trustworthy by other non-regular serving military veterans of the GW and other readers of this topic
Discussion
Of particular relevance to the conduct of the GW, the rapid manoeuvre and movement in modern warfare makes casualty collection and evacuation both dangerous and problematic. As such, it is reported as presenting difficult decisions for doctors [19] and by default for those working with them. Following the experience of the GW, hypothetical difficulties for military surgeons working with wounds contaminated by chemical agents were explored [20]. The authors found that guidance during the GW was inadequate to deal with this eventuality, as was the means of assessing casualty and surgical staff’s contamination risk. This suggests that had chemical agents been used in the GW, these deficiencies could have been particularly problematic for surgical nurses with extended roles, as described by Cooper [21] based in a field hospital as a senior nurse Reservist. The HPVs in general hospitals reported difficulties in adapting from civilian to military practices and to using old equipment, whereas those in field hospitals focussed upon the generally poor and challenging conditions of their desert accommodation and work conditions compounded by the harsh climate.
Care-giving in field hospitals was reported as less personal than that in general hospitals and bears similarity with the findings of Barker’s comparative study of US Vietnam War veteran nurses with those from Scutari during the Crimean War [11]. This could be because the speed of throughput of triaged casualties in field hospitals (once stabilised they were evacuated to general hospitals) left little time or opportunity for personal relationshipbuilding between the carer and those cared for. Ethical concerns related to casualty care were reported by the HPVs nursing both enemy and allied casualties in field hospitals but not in general hospitals. Concerns were raised about the organisational problems associated with caring for Iraqi and allied casualties together in the same ward, and the inadequacy and age of equipment but of greater importance were allegations by some HPVs of the ill treatment of the Iraqi casualties. Neither the identity nor the number of military perpetrators involved were reported by the HPVs.
However, as those who cared for both enemy and allied casualties in field hospitals experienced greater disharmony with other military personnel, and the environment had many other stressors, it seems plausible that some field hospital care staff could have exhibited altered behaviour as a stress response similar to the outcomes of experiments by Milligram [22]. Curtailing the malpractice of others included HPVs’ efforts to lessen contact between perpetrators with Iraqi casualties but the low staff: casualty ratio made this difficult to achieve.
Protection of prisoners of war from ill treatment is embodied in the Geneva Convention [23] and all personnel should know this from training but similar to this British perspective, in a US study of its military ethical training some military personnel did not internalised what was taught [24]. It is of note that training deficits for casualty care were also reported by a third of HPVs in a further article based upon other findings from this study [25].
Conclusion
Participation in warfare is a testing personal experience for military personnel involved in any war but for the HPVs caring for casualties in the GW, they had the additional anticipatory worry that Iraq might release chemical agents against them. Although allied casualties did not meet expectations in terms of number, there was a large number of Iraqi Prisoners of War requiring medical/surgical care. Desert-based field hospitals had the additional problems of the discomfort of the tented living conditions compounded by the climate. Although most HPVs seemed to cope well, the observed malpractice of unidentified ‘other’ military personnel with the Iraqi casualties was a source of inter-military group disharmony in the generally stressful environment of field locations. However, it is not known how prevalent this deviation in care standards was, what form it took, or whether it was reported to a higher command.
Declaration
I declare that the manuscript is original and is neither published nor communicated for publication elsewhere either in part or in full.
References
- de la Billiere P (1992) Storm command: A personal account of the Gulf War. Harper Collins Publishers, London, p. 117.
- Wild D, Brooking JI (1991) Crisis in the Gulf: The right treatment. Nursing Standard 5(22): 21-22.
- Adley R, Evans DHC, Mahoney PF, Riley B, Rogers CR, et al. (1992) The Gulf War; Anaesthetic experience at 32 field hospital department of Anaesthesia and Resuscitation. Anaesthesia 47(11): 996-999.
- Adley R (1992) Naval Party 1036: Its role in the Gulf conflict. Journal of the Royal Navy Medical Service 78(2): 65-71.
- Hotchin RJ (1993) Report of a lecture. Medical standardisation issues from operations. The Canadian perspective. Report of a lecture. Journal of the Royal Army Medical Corps 139(1): 7-10.
- Smith BJ (1993) The nurse executive in Operation Desert Shield/Desert Storm. Nursing Management 24(1): 68-70.
- Martin TE (1992) Al Jubail- an aeromedical staging facility during the Gulf conflict: Discussion paper. Journal of the Royal Society of Medicine 85(1): 32-36.
- Souka HM (1992) Management of Gulf War casualties. British Journal of Surgery 79(12): 1307-1308.
- Lee R, Ashforth B (1990) On the meaning of Maslach’s three dimensions of burnout. Journal of Applied Psychology 75(6): 743-747.
- Brooking JI (1983) Potential psychological problems of Army medical services personnel in combat with particular reference to the Territorial Army. Journal of the Army Medical Corps 129(3): 146-151.
- Barker ER (1989) Caregivers as casualties. Western Journal of Nursing Research 11(5): 628-631.
- Ryan JM, Cooper GJ, Haywood IR, Milne SM (1991) Field surgery on a future conventional battlefield: strategy and wound management. Ann R Coll Surg Engl 73(1): 13-20.
- Spoonster SL (1987) Women and the vietnam experience. Journal of Nursing Scholarship 19(4): 168-173.
- Gunby P (1991) Physicians provide continuum of care for desert storm fighting forces. Journal of the American Medical Association 265(5): 557-559.
- Creswell W (2003) Research design: qualitative and mixed methods approaches. Sage Publications, USA.
- Merril J, Williams A (1995) Benefice, respect for autonomy and justice: principles in practice. Nurse Res 3(1): 24-34.
- Krippendorff K (2004) Content analysis: An introduction to its methodology. Newbury Park and London: Sage, USA, pp. 272-273.
- Lee HA, Gabriel R, Bolton PJ, Bale AJ, Jackson M (2002) Health status and clinical diagnoses of 3000 UK Gulf War veterans. J R Soc Med 95(10): 491-497.
- Inge P (1982) The doctor in the Army. Journal of the Royal Army Medical Corps 128(1): 28-32.
- Cooper J, Ryan JM, Galbraith KA (1994) The surgical management in war of penetrating wounds contaminated with chemical warfare agents. J R Army Med Corps.140(3): 113-118.
- Cooper C (1991) Saddam Hussein-my part in his downfall. Queen Elizabeth College of Nursing and Health Sciences Magazine. pp. 2-3.
- Milgram S (1963) Behavioural study of obedience. Journal of Abnormal and Social Psychology 67(4): 371-378.
- Scholars for Peace in the Middle East (2005) Understanding the Fourth Geneva Convention.
- Carter BS. (1994) Ethical concerns for physicians deployed to Operation Desert Storm. Military Medicine 159(1): 55-59.
- Wild D (2018) UK Gulf War Health Professional Veterans’ Perceptions of and Recommendations for Pre-Deployment Training: The Past Informing an Uncertain Future? Research and Reviews, Health Care Open Access Journal 2(2): RRHOAJ.MS.ID.000134.
© 2019 Deidre Wild. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






