- Submissions

Full Text
COJ Nursing & Healthcare
Effect of Clozapine on Appetite, Weight and Insulin Resistance in Schizophrenia Patient in Mental Health Psychiatry Outpatient Clinics KFSH&RC (Case Report)
Eltoum E*
Depatrment of Medicine, Khartoum, Sudan
*Corresponding author: Eltoum E, Depatrment of Medicine, Khartoum, Sudan
Submission: October 01, 2018Published: March 18, 2019

ISSN: 2577-2007Volume4 Issue5
Abstract
Background: Schizophrenia is a psychotic disorder with a complex pathophysiology and requires treatment that includes long term administration of antipsychotics that is said to be associated with metabolic syndrome.
Objective: To estimate the prevalence of metabolic syndrome in patients taken clozapine at King Faisal Specialist Hospital &Research Centre, Outpatient clinics.
Methods: This study was conducted at outpatient setting, KFSH&RC. Total patients included in this study are 39 patients. All patients were on maintenance dose of clozapine therapy. Measurement of anthropometric (body weight (BMI), waist circumference, blood pressure) and biochemical parameters (glucose, insulin, triglycerides, LDL, HDL) were recorded, Data analyses were collected during their regular follow-ups.
Result: The prevalence of the metabolic syndrome was significantly higher among clozapine patients according to all literature but in this study 3 patients out of 39 were affected. The analysis revealed significant associations with age, body mass index, and duration of clozapine medication & family history.
This finding is consistent with literature about associated with clozapine& mentioned risk factor. Our three affected patients had the following result.
BMI: (A-27- B-41.3) male with normal (16-30)
BMI: (C-49.1) female with normal (16-30)
Blood sugar range: (A-GLUF is11.5mmol/l) with HDL 1.41 normal (1.04-1.55mmol/l), LDL 3.98 optimal < 2.59mmol) =accordingly to the national cholesterol education program (NCEP us has set the following guide lines (references values)
B-GLUF: (5.4mmol/L, HDL.0.90mmol/l, LDL2.74mmol/l
C-GLUF: (9.5mmol/l, HDL1.20 mmol/l, LDL3.07 mmol/l
Demographical Data
Age=for all 39 patients (C-34, A-47, B-47 years) age group (20 yeas-3-patients, 30 years-10 patients, 40 years-12 patients, 50 years-11 patients, 60-70years about 3 patients.
Gender: For all 39 were about 26 males, 13 female patients (2 Males 1 Female)
Marital status: Single 19 patients, married, 15 patients, divorced- 5 patients
Exclusion criteria
A. Patient who is taking clozapine combined with another antipsychotic.
B. Children
C. Elderly patient with Dementia
Conclusion
Patients receiving clozapine are at significantly increased risk for developing the metabolic syndrome. Psychiatrists and other providers should consider performing regular physical health monitoring to prevent long-term adverse health consequences. Metabolic syndrome is a collection of risk factors that are associated with increased morbidity and mortality due to cardiovascular disease [1]. Schizophrenia has long been associated with elements of the metabolic syndrome, and numerous studies have found increased mortality because of cardiovascular disease [2-4].
Several possibilities have been suggested to explain these associations in schizophrenia, including poor diet, lack of exercise, cigarette smoking, and stress, as well as abnormalities of the hypothalamic-pituitary-adrenal axis [5-7]. In recent years, treatment with antipsychotic medications has been recognized as an additional risk factor for the development of metabolic abnormalities [8]. Clozapine was approved by the Food and Drug Administration in, yet it remains the only antipsychotic medication with established efficacy in treatment-resistant schizophrenia patients [9].
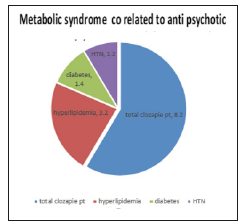
Despite its efficacy, growing evidence suggests that clozapine has a substantial effect on metabolic parameters. In a metaanalysis of over 80 studies examining weight gain [10], Clozapine treatment was associated with an average gain of 9.8lb. Over 10 weeks-the most of any antipsychotic drug. More case reports of clozapine-associated glucose abnormalities have been submitted to the Food and Drug Administration [11] and published [12] than for any other antipsychotic drug (Figure 1). Reports have also associated clozapine treatment with the development of Hypertriglyceridemia [13], Increased total cholesterol levels [14], and Hypertension [15]. The purpose of this study was to assess the prevalence of the metabolic syndrome among a group of outpatients receiving clozapine. The National Cholesterol Education Program’s definition of the metabolic syndrome was chosen for our study purposes because of its ease of use in clinical practice [16].
Figure 1:
References
- Lakka HM, Laaksonen DE, Lakka TA, Niskanen LK, Kumpusalo E, et al. (2002) The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA 288(21): 2709-2716.
- Ryan MCM, Thakore JH (2002) Physical consequences of schizophrenia and its treatment: The metabolic syndrome. Life Sci 71(3): 239-257.
- Curkendall SM, Jingping M, Glasser DB, Rose Stang M, Jones JK (2004) Cardiovascular disease in patients with schizophrenia in Saskatchewan, Canada. J Clin Psychiatry 65(5): 715-720.
- Brown S (1997) Excess mortality of schizophrenia: A meta-analysis. Br J Psychiatry 171: 502-508.
- Ryan MC, Collins P, Thakore JH (2003) Impaired fasting glucose tolerance in first-episode, drug-naive patients with schizophrenia. Am J Psychiatry 160(2): 284-289.
- Dixon L, Weiden P, Delahanty J, Goldberg R, Postrado L, et al. (2000) Prevalence and correlates of diabetes in national schizophrenia samples. Schizophr Bull 26(4): 903-912.
- Holmberg SK, Kane C (1999) Health and self-care practices of persons with schizophrenia. Psychiatr Serv 50(6): 827-829.
- Lehman AF, Lieberman JA, Dixon LB, McGlashan TH, Miller AL, et al. (2004) Practice guideline for the treatment of patients with schizophrenia, (2nd edn), Am J Psychiatry 161(2 Suppl): 1-56.
- Chakos M, Lieberman J, Hoffman E, Bradford D, Sheitman B (2001) Effectiveness of second-generation antipsychotics in patients with treatment- resistant schizophrenia: A review and meta-analysis of randomized trials. Am J Psychiatry 158(4): 518-526.
- Allison DB, Mentore JM, Heo M, Chandler LP, Cappelleri JC, et al. (1999) Antipsychotic-induced weight gain: A comprehensive research synthesis. Am J Psychiatry 156(11): 1686-1696.
- Citrome LL, Jaffe AB (2003) Relationship of atypical antipsychotics with development of diabetes mellitus. Ann Pharmacother 37(12): 1849- 1857.
- Lamberti JS, Costea GO, Olson D, Crilly JF, Maharaj K, et al. (2005) Diabetes mellitus among outpatients receiving clozapine: Prevalence and clinical-demographic correlates. J Clin Psychiatry 66(7): 900-906.
- Meyer JM, Koro CE (2004) The effects of antipsychotic therapy on serum lipids: A comprehensive review. Schizophr Res 70(1): 1-17.
- Casey DE (2004) Dyslipidemia and a typical antipsychoic drugs. J Clin Psychiatry 65(Suppl): 27-35.
- Henderson DC, Daley TB, Kunkel L, Rodrigues Scott M, Koul P, et al. (2004) Clozapine and hypertension: A chart review of 82 patients. J Clin Psychiatry 65(5): 686-689.
- Expert panel on detection, Evaluation, and Treatment of high blood cholesterol in adults (2001) Executive summary of the third report of the national cholesterol education program (NCEP) expert panel of detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). JAMA 285(19): 2486-2497.
© 2019 Eltoum E. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






