- Submissions

Full Text
COJ Nursing & Healthcare
The Mediating-Moderating Role of Hopelessness between Quality of Life and Depression in Cancer Patients
Srishti Tody1 and Sunali Khanna2*
1 Private practice, India
2 Nair Hospital Dental College, India
*Corresponding author: Sunali Khanna, President Asian Academy of Oral and Maxillofacial Radiology Vice President Indian Academy of Oral Medicine & Radiology, Diplomate of National Boards of OMR, Member National Academy of Medical Sciences, Nair Hospital Dental College, Mumbai, India
Submission: December 11, 2018;Published: January 16, 2019

ISSN: 2577-2007Volume4 Issue4
Introduction
Cancer patients experience a variety of symptoms. Greater symptom freight has been associated with higher levels of emotional suffering, poor functioning and overall quality of life Heidrich et al. [1]. Quality of life is an important principle in oncology Alejandro et al. [2]. The occurrence of mental disorders is common in cancer patients, particularly at the final stage of the illness, while intense patient distress is a critical public health issue Car et al. [3]. Hopelessness is one of the most frequent and important conditions described in medically ill patients Dunn et al. [4]. Few topics have created as much interest in end-of-life research as the construct of hopelessness Rosenfeld et al. [5]. It has been studied in different contexts and has been found to have a negative impact on subjective well-being and physical outcome Valtonen et al. [6]. It has been argued that, in severe illness, a terminal prognosis is compatible with hopelessness, and the absence of hopelessness solely reflects a lack of knowledge of diagnosis-prognosis [5].
Nevertheless, many patients have hope and can move to more realistic, even though, often short-term goals (e.g., pain management). In addition, hopelessness also predicts general mood outcomes and functioning in the presence of affective disorders Pompili et al. [7]. Hopelessness relates to the tendency to adopt a pessimistic attitude about the illness Patoo et al. [8] and is one of the strongest predictors of end-of-life decision making regarding issues such as physician-assisted suicide, desire for hastened death, advance directives, and requests for life-sustaining interventions [5]. As cancer is a life-threatening illness, it is a source of great distress Linden et al. [9]. Studies using Diagnostic for Statistical Manual of Mental Disorders (DSM) criteria have found that in palliative care the rates of depression are as high as 49.0% Ciaramella & Poli [10]. Moreover, cancer patients who have reported less quality of life experienced more depressive symptoms Colby & Shifren [11]. Screening is important to identify patients who are depressed and would benefit from further support Pinquart & Duberstein [12].
In Greece, depression has been assessed in cancer patients Mystakidou et al. [13] in patients undergoing chemotherapy, Polikandroti et al. [14] in advanced cancer patients Mystakidou et al. [15] and in breast cancer survivors Fafouti et al. [16]. Cancer patients suffering from depression are at increased risk of mortality compared to non-depressed patients [12]. Though hopelessness is associated with depression, it is oriented to the future as opposed to the present state Beck & Weissman [17]. According to DSM hopelessness is not part of depression based on the DSM (APA, 2013). Hopelessness in cancer patients seems not exclusively to correspond to depression, but is related to various other psychosocial factors, such as maladaptive coping Grassi et al. [18]. Decreased quality of life, hopelessness, and depression are some of the most frequent psychological symptoms found in cancer patients Spangenberg et al. [19]. Therefore, the aim of the present study is to investigate the interaction of mental quality of life, hopelessness and depression among cancer patients is not well known.
Methods
The current study was carried out in an outpatient palliative care unit in Greece were 160 consecutive advanced cancer patients visited the unit for palliative care. Inclusion criteria were: cancer diagnosis, patients’ stage IV, age >18 Years, adequate communication with the healthcare professionals, and participants’ written informed consent. Exclusion criteria were: a diagnosis of a psychotic illness or significant cognitive impairment. One hundred twenty-five advanced cancer patients were eligible to enter the study. Twenty-three patients (18.4%) either refused or were unable to complete the assessment forms due to long distance and, thus, were excluded from the study. The final sample consisted of 102 cancer patients. The study was performed in accordance with the Helsinki Declaration and according to European guidelines for good clinical practice. The study was approved by the hospital’s institutional review board, while informed consent was obtained from all patients included in the study.
Instruments
The Medical Outcomes Study SF-12 consists of two dimensions-a physical component (SF12-PCS) and a mental component (SF12- MCS) summary score was used Ware et al. [20]. Higher scores indicate better health Arora & Pisu [21]. Hopelessness of patients was measured by the Greek version of the Beck Hopelessness Scale (BHS) Beck et al. [17]. It is a 20-item self-report inventory with Cronbach alpha of patients was 0.937. It was designed to tap a general tendency towards pessimism and negative expectancies. Beck et al. [17] extracted three factors (affective, motivational, and cognitive) Beck et al. [17], Beck & Steer [22]. Depressive symptomatology was measured by the Greek version of the Beck Depression Inventory (BDI) was used (Cronbach alpha= .906) Mystakidou et al. [23]. The BDI Ward et al. [24]. It is a 21 items self-report scale, measuring characteristic attitudes and symptoms of depression
Statistical analyses
Firstly, correlations between quality of life, hopelessness, and depression were explored using Spearman’s correlation coefficients. Secondly, regression-based PROCESS with bootstrapping 5,000 samples Preacher & Hayes [25] was used to evaluate in what extent the effect of quality of life was mediated through hopelessness and depression. Depression as the dependent variable, quality of life as the predictor, and hopelessness as mediator were considered significant if the 95% bias-corrected confidence interval of the indirect effect did not include 0. Unstandardized indirect effects were computed for each of 5,000 bootstrapped samples, and the 95% confidence interval was computed by determining the indirect effects at the 2.5 and 97.5 percentiles. Finally, a moderating analysis was performed with PROCESS model investigating the role of hopelessness on the relationship between quality of life and depression. Statistical significance was set at p< .05. Statistical analyses were conducted using SPSS version 21 (IBM Corp, Armonk, NY) and the macro PROCESS for mediation and moderation analyses.
Result
Descriptive statistics
Table 1:Demographic and disease related patient’s characteristics.

Table 2:Correlation between quality of life, hopelessness, depression, and age.
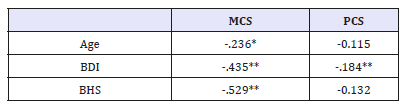
All values are presented as Spearman’s correlation coefficient * p<.05, ** p<.0005
Means, standard deviations, and percentages of the assessed variables are presented in Table 1. As shown in Table 2, there was a strong negative correlation between age and mental quality of life (r=-.236, p<.05). Moreover, depression had a strong negative correlation with mental quality of life (r=-.435; p<.0005), and physical quality of life (r=-.184; p<.0005). On the other hand, hopelessness had a strong negative correlation with mental quality of life (r=-.529; p<.05).
Moderation analyses
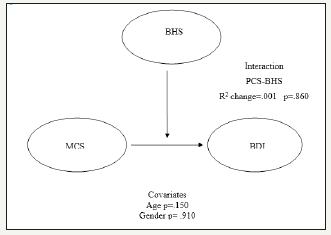
Process analyses were explored to examine if the relationship between mental quality of life and depression (controlling for age and gender) is strong for patients with hopelessness. For depression, the main effects of mental quality of life and hopelessness (controlling for age and gender), as well as the interaction effects accounted for 30% of the variance [R2= .30, F (5.96) = 10.12, p<.001)]. However, the interaction for mental quality of life and depression and mental quality of life and hopelessness were not significant [R2 Change=.001, F(1.109) = .03, p=.860] suggesting no moderation effect of hopelessness (Figure 1).
Figure 1:Moderation effect of BHS between MCS and BDI.
MCS: Mental Component Score
PCS: Physical Component Score
BDI: Beck Depression Inventory
BHS: Beck Hopelessness Scale
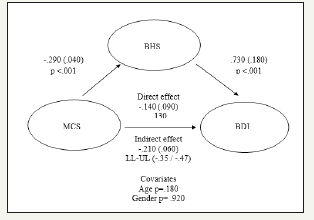
Mediation analyses
Mediation analysis was assessed so as to explore whether hopelessness mediates the association between mental quality of life and depression. The bootstrapping method was applied. In the current analysis, depression was the dependent variable, mental quality of life was entered as the independent variable and hopelessness as the mediator, while age and gender acted as covariates. All variables were examined with the SPSS macro model Preacher & Hayes [25]. Results have shown that mental quality of life was a significant predictor of hopelessness (beta=-.29, SE=.04, p<.001) and hopelessness was a significant predictor of depression (beta=.70, SE=.18, p<.001). The direct effect of mental quality of life to depression was not statistically significant after controlling of covariates and mediator (beta=.14, SE=.19, p=.130). The indirect effect was explored using a bootstrap estimation approach with 5,000 samples Preacher & Hayes [25]. Therefore, the indirect coefficient for hopelessness was significant (beta=-.210, SE=.06, CI = (-.47/-.35), after controlling of covariates, consistent with partial mediation. The ratio of indirect to total effect for hopelessness (beta=.60, SE=.17) indicates that hopelessness accounts for approximately 60% of the shared variance between mental quality of life and depression (Figure 2).
Figure 2:Mediation effect of BHS, between MCS and BDI.
All values are presented as Beta (S.E)
LL: Lower Limit, UL: Upper Limit
Discussion
This is the first study that examines the mediating-moderating effect of hopelessness between quality of life and depression in palliative cancer patients. Special attention was given to the effect of hopelessness as mediator-moderator in the quality of lifedepression relationship. This study highlights the significance of mental quality of life and hopelessness in advanced cancer patients’ depression. Although the life expectancy of patients with cancer has increased thanks to technological advancements, patients’ quality of life is often poor due to chronic physical and psychological distress Yildirim et al. [26]. Lower mental quality of life (MCS) has been found to leed to higher rates of all-cause mortality, even after accounting for differences in disease, demographics, and comorbidity Alam et al. [27].
Misdiagnosis of mood disorders can be open to doubt because they lessen quality of life, affect compliance with medical therapies and probably reduce survival Reich et al. [28]. Especially in advanced cancer depression is a significant comorbidity Papamichail et al. [29]. The advanced stage of the disease along with the lack of social resources exacerbate depressive disorders Priscilla et al. [30]. Studies have shown that while individuals with depression experience higher levels of hopelessness than those without depression Chochinov [31], also hopelessness can lead to detachment, and depression Sachs et al. [32]. In oncology, several studies have aimed their attention on hopelessness as a maladaptive coping style Rizvi [33]. Moreover, hopelessness has been associated with a desire for hastened death and a lower quality of life Sachs et al. [32].
Another finding of the present study, supported by the literature, is that age was found to have a significant negative correlation with mental quality of life Kenzik et al. [34] and Weaver et al. [35]. Hence age should be taken into consideration when addressing psychological distress and quality of life. Concluding, hopelessness appears to be a significant psychological dimension that needs further research in oncology palliative care, in order to better understand the role of psychological dimensions in medical conditions Fava et al. [36] and develop specialized interventions. In light of the importance of addressing psychopathology among these patients Lottick et al. [37], the proposed mediation model needs to be confirmed in future studies, by including more comprehensive examinations of the assessed variables that impact mental health and well-being [38].
References
- Heidrich SM, Egan JJ, Hengudomsub P, Randolph SM (2006) Symptoms, symptom beliefs, and quality of life of older breast cancer survivors: A comparative study. Oncol Nurs Forum 33(2): 315-322.
- Alejandro DTL, Gambara H, López E, Cruzado JA (2016) Psychological treatments to improve quality of life in cancer contexts: A meta analysis. International Journal of Clinical and Health Psychology 16(2): 211-219.
- Car J, Zycińska J, Lasota W (2012) Assessment of psychological distress and depression in cancer patients. Przeglad epidemiologiczny 66(4): 689-695.
- Dunn SL (2005) Hopelessness as a response to physical illness. Send toJ Nurs Scholarsh 37(2): 148-154.
- Rosenfeld B, Pessin H, Lewis C, Abbey J, Olden M, et al. (2011) Assessing hopelessness in terminally ill cancer patients: Development of the hopelessness assessment inillness questionnaire. Psychol Assess 23(2): 325-336.
- Valtonen M, Laaksonen D, Tolmunen T, Nyyssönen K, Viinamäki H, et al. (2008) Hopelessness- novel facet of the metabolic syndrome. Scand J Public Health 36(8): 795-802.
- Pompili M, Innamorati M, Gonda X, Serafini G, Sarno S, et al. (2013) Affective temperaments and hopelessness as predictors of health and social functioning in mood disorder patients: a prospective follow-up study. J Affect Disord 150(2): 216-222.
- Patoo M, Allahyari AA, Moradi AR, Payandeh M, Hassani L (2018) Studying the relation between mental adjustment to cancer and healthrelated quality of life in breast cancer patients. International Journal of Cancer Management 11(7): e8407.
- Linden W, Vodermaier A, Mackenzie R, Greig D (2012) Anxiety and depression after cancer diagnosis: Prevalence rates by cancer type, gender, and age. J Affect Disord 141(2-3): 343-351.
- Ciaramella A, Poli P (2001) Assessment of depression among cancer patients: The role of pain, cancer type and treatment. Psychooncology 10(2): 156-165.
- Colby DA, Shifren K (2013) Optimism, mental health, and quality of life: A study among breast cancer patients. Psychol Health Med 18(1): 10-20.
- Pinquart M, Duberstein PR (2010) Depression and cancer mortality: A meta-analysis. Psychological Medicine 40(11): 1797-1810.
- Mystakidou K, Parpa E, Tsilika E, Gogou P, Panagiotou I, et al. (2010) Self-efficacy, depression, and physical distress in males and females with cancer. American Journal of Hospice and Palliative Care 27(8): 518-525.
- Polikandroti M, Evaggelou E, Zerva S, Zerdila M, Koukoularis D, et al. (2008) Evaluation of depression in patients undergoing chemotherapy. Health Science Journal 2(3): 162-172.
- Mystakidou K, Tsilika E, Parpa E, Katsouda E, Galanos A, et al. (2005) Assessment of anxiety and depression in advanced cancer patients and their relationship with quality of life. Qual Life Res 14(8): 1825-1833.
- Fafouti M, Paparigopoulos T, Zervas Y, Rabavilas A, Malamos N, et al. (2010) Depression, anxiety and general psychopathology in breast cancer patients: a cross-sectional control study. In Vivo 24(5): 803-810.
- Beck AT, Weissman A (1974) The measurement of pessimism: The hopelessness scale. J Consult Clin Psychol 42(6): 861-865.
- Grassi L, Travado L, Gil F, Sabato S, Rossi E, et al. (2010) Hopelessness and related variables among cancer patients in the Southern European Psycho-Oncology Study (SEPOS). Psychosomatics 51(3): 201-207.
- Spangenberg L, Zenger M, Torres GF, Mueller V, Reck M, et al. (2016) Dimensionality, stability, and validity of the beck hopelessness scale in cancer patients receiving curative and palliative treatment. J Pain Symptom Manage 51(3): 615-622.
- Ware J E, Kosinski M, Keller SD (1996) A 12-item short-form health survey: Construction of scales and preliminary tests of reliability and validity. Med Care 34(3): 220-233.
- Arora N, Pisu M, Kenzik KM, Ganz PA, Martin MY, et al. (2015) How much do cancer-related symptoms contribute to health-related quality of life in lung and colorectal cancer patients? A report from the Cancer care outcomes research and surveillance (CanCORS) consortium. Cancer 121(16): 2831-2839.
- Beck AT, Steer RA (1988) Manual for the beck hopelessness scale. Psychological Corporation, Texas, USA.
- Mystakidou K, Tsilika E, Parpa E, Smyrniotis V, Galanos A, et al. (2007) Beck depression inventory: Exploring its psychometric properties in a palliative care population of advanced cancer patients. Eur J Cancer Care (Engl) 16(3): 244-250.
- Beck AT, Ward CH, Mendeson M, Mock J, Arbough J (1961) An inventory for measuring depression. Arch Gen Psychiatry 4: 561-571.
- Preacher KJ, Hayes AF (2004) SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments & Computers 36(4): 717-731.
- Yildirim Y, Sertoz OO, Uyar M, Fadiloglu C, Uslu R (2009) Hopelessness in Turkish cancer inpatients: The relation of hopelessness with psychological and disease-related outcomes. Eur J Oncol Nurs 13(2): 81-86.
- Alam R, Patel H, Pierorazio PM (2018) Self-reported quality of life as a predictor of survival in renal cell carcinoma. Journal of Clinical Oncology 36(6): 595.
- Reich M, Lesur A, Perdrizet CC (2008) Depression, quality of life and breast cancer: A review of the literature. Breast Cancer Res Treat 110(1): 9-17.
- Papamichail E, Katsaouni P, Maillis P (2017) Depression, pain and mental state in cancer patients. International Journal of Caring Sciences 10(2): 955-962.
- Priscilla D, Hamidin A, Azhar MZ, Noorjan KO, Salmiah MS, et al. (2011) Assessment of depression and anxiety in haematological cancer patients and their relationship with quality of life. East Asian Arch Psychiatry 21(3): 108-114.
- Chochinov HM (2003) Thinking outside the box: Depression, hope, and meaning at the end of life. Journal of Palliative Medicine 6(6): 973-977.
- Sachs E, Kolva E, Pessin H, Rosenfeld B, Breitbart W (2013) On sinking and swimming: The dialectic of hope, hopelessness, and acceptance in terminal cancer. Am J Hosp Palliat Care 30(2): 121-127.
- Rizvi T (2017) A Study of relationship between hopelessness and coping strategies in cancer patients. The International Journal of Indian Psychology 5(1).
- Kenzik K, Ganz PA, Martin M, Petersen L, Hays RD, et al. (2015) How much do cancer-related symptoms contribute to health-related quality of life in lung and colorectal cancer patients? A report from the cancer care outcomes research and surveillance (CanCORS) consortium. Cancer 121(16): 2831-2839.
- Weaver KE, Forsythe LP, Reeve BB, Alfano CM, Rodriguez JL, et al. (2012) Mental and physical health-related quality of life among U.S. cancer survivors: population estimates from the 2010 National Health Interview Survey. Cancer Epidemiol Biomarkers Prev 21(11): 2108- 2117.
- Fava GA, Fabbri S, Sirri L, Sirri L, Wise TN (2007) Psychological factors affecting medical condition: a new proposal for DSM-V. Psychosomatics 48(2): 103-111.
- Lottick KNS, Vanderwerker LC, Block SD, Zhang B, Prigerson HG (2005) Psychiatric disorders and mental health service use in patients with advanced cancer: A report from the coping with cancer study. Cancer 104(12): 2872-2881.
- American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders (DSM-5) (5th edn), APA, Washington DC, USA.
© 2018 Ktriaki Mystakidou. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






