- Submissions

Full Text
COJ Nursing & Healthcare
How is Care Complexity Associated with Medication Confidence and Adherence? An Analysis of the SAFE-PHASE Study in Singapore
Ying Guo1,2*, Heather Whitson1,2, Truls Østbye1,3, Alison Luciano2 and Rahul Malhotra4,5
1 Duke-NUS Medical School, Singapore
2 Center for Study of Aging and Human Development, Duke University, USA
3 Department of Community and Family Medicine, Duke University, USA
4 Centre for Ageing Research and Education, Duke-NUS Medical School, Singapore
5 Health Services and Systems Research, Duke-NUS Medical School, Singapore
*Corresponding author: Ying Guo, Duke-NUS Medical School, Singapore, Tel: 65-82692487; Email:gy23@duke.edu/guo.ying@duke.edu
Submission: July 23, 2018;Published: August 27, 2018
ISSN: 2577-2007Volume4 Issue1
Abstract
As the number of patients with high morbidity and medication burden increases, it is important to understand care patterns and patient behaviors in complex populations. Few studies on confidence and medication adherence have been conducted among older East Asian populations [1-4]. The aim of this study was to investigate whether older adults who demonstrate care complexity (multiple providers or outpatient healthcare visits) express varying levels of confidence in medication use and non-adherence. Participants of a nationally representative survey of older Singaporeans were selected for analysis (N=1302). Associations of interest were assessed using logistic regression, controlling for age, gender, ethnicity [5], education, medications and comorbidities. Compared to participants who had no visits to a provider in the past 3 months, participants with one visit to a single provider (OR=3.05, 95% CI 1.81 - 5.14), two visits -each to a different provider (OR=2.49, 95% CI 1.34 - 4.65) and multiple visits or providers (OR=2.51, 95% CI 1.62 - 5.03) expressed lower confidence in medication use [6]. There was no association between care complexity and medication non-adherence. Among older Singaporeans, high care complexity was associated with lower confidence in medication use, but not to medication non-adherence
Keywords: Geriatric health/Gerontology; Medication adherence; Health care reforms; Health care services; Multiple chronic conditions
Introduction
Older adults, and especially those with multiple chronic conditions, often see several providers and access outpatient care frequently, yet coordination between these points of care remains inadequate [7]. Complexity of healthcare, most often seen in the elderly, can be a risk factor for lack of confidence about medication recommendations, or relate to non-adherence to medication regimens [1-10]. Medication adherence (also called compliance)- the extent to which patients take medication as prescribed by their healthcare provider-is a shared responsibility between patient and physician [1-3]. Approximately 50% of older adults (age >65) in the United States do not adhere to at least one of their chronic medications [2]. It is therefore important to identify barriers to medication adherence, which has become a growing problem, often overlooked in the busy primary care setting. According to Singapore’s Ministry of Health, Singapore has a life expectancy which has increased by 10years over the last 3 decades: from 72 years in 1980 to 82 years in 2010. By 2030, a fifth of Singaporeans will be 65years and older. As an influx of elderly persons enter the health system each year, so will the rising cost of disability and morbidity burden. Few studies on medication adherence have been conducted on East Asian populations [4].
Non-adherence is a phenomenon determined by a complex set of issues including physician-patient communication, cognitive decline, and the cost of medication. Interventions aimed at increasing adherence have focused on these factors [5]. However, these interventions often assume that the problem lies in a deficit of information and thus, correction of such deficit will change behaviors [3,5]. The possibility remains that patients may choose to be non-adherent, or lack resources to be adherent, despite receiving correct information [3,6]. According to Pham et al. [3], non-adherence may not simply be a knowledge discrepancy, but can involve feelings, reactions to the physician, cost, availability, and competing medical belief systems.
Previous work has shown that discrepancies in medication adherence are more common in older people and those who have polypharmacy, multiple chronic conditions, or multiple providers [1,7]. Previous studies have shown that poor adherence to medications puts patients at risk of adverse effects or toxicity, increased hospital admissions, health care costs, worsening of disease, deaths, and incorrect evaluation of the effectiveness of a therapeutic regimen leading to overmedication [1-3]. Inorder to facilitate better adherence and prevent medication-related adverse outcomes, it is important to identify individuals at heightened risk of non-adherence [8-11]. With increasing numbers of effective self-administered treatments, there is imminent need for better understanding and management of non-adherence [5].
This analysis is based on the premise that complexity in health care use (characterized by multiple encounters with different providers) may be a risk factor for lower confidence about medication recommendations and relate to poor adherence to medication. If patterns of healthcare service use were found to be a risk factor for medication non-adherence, this could provide a feasible means of targeting patients who may benefit from interventions, such as patient/caregiver education or case management, to bolster adherence. Healthcare service patterns are easily detected in administrative data, and electronic health records can be used to “flag” patients with certain utilization patterns, which could facilitate detection of patients at risk. Thus, the aim of this study was to investigate whether seniors who have high care complexity express lower levels of confidence in medication use and are at high risk of non-adherence.
Materials and Methods
This study was a secondary analysis of cross-sectional data collected in Wave 3 of the Panel on Health and Ageing of Singaporean Elderly (PHASE), a nationally representative longitudinal survey of community-dwelling older adults in Singapore. The researchers obtained written informed consent from older persons or their proxy, if applicable, and used a structured questionnaire for data collection.
Survey Sampling Procedure
Wave 1 of PHASE, conducted in 2009, included communitydwelling older adults (>60 years). A random sample of 8400 older adults, with a target sample size of 5000, stratified by gender, ethnic group and 5-year age groups based on the 2007 population distribution was drawn from the national database of dwellings [12]. Adults aged >75 years, and Malays and Indians were oversampled by a factor of two to ensure sufficient numbers in these groups for analysis (i.e. for more precise point estimates) [12].
A total of 4990 older adults or their proxies (if the older adult was unable to respond due to health reasons; n=458) were interviewed for Wave 1 in person at their residence, yielding a response rate of 69% [12]. A total of 3103 participants (62%) were successfully re-interviewed for Wave 2 (conducted in 2011). And, a total of 1572 participants were successfully re-interviewed for Wave 3 (conducted in 2015). For this analysis, self-reported data collected in Wave 3 of PHASE (also known as SAFE-PHASE) from 1302 older adults who reported taking regular prescription medications, was used.
Outpatient Care Complexity Factors
The primary predictors of interest to characterize the complexity of outpatient healthcare service use were
A. The number of outpatient health care providers consulted in the last 3 months and
B. The number of outpatient visits to a provider in the last 3 months.
This information was determined from survey responses. A composite “care complexity” variable capturing number of providers and number of visits was used to account for the overlap between the two indicators of complexity. The care complexity variable was collapsed into four categories: no visits to a provider in the past 3months, one visit to a single provider, two visits - each to a different provider, and multiple visits or providers.
Medication Confidence and Adherence
The outcomes of interest were confidence in taking prescription medications and medication adherence. Confidence with medication use was assessed with the question “How confident do you feel that you are able to take your prescribed medications correctly?” Possible responses ranged on a Likert scale from 1- Extremely Confident, 2-Quite a bit, 3-Somewhat, 4-A little bit, to 5- Not at all. Medication adherence was assessed with the question “At times do you (subject) forget to take your (subject’s) prescription medications?” Possible responses included Yes or No. In statistical models, decreased confidence was coded “not at all”, “a little bit”, “somewhat”, “quite a bit” confident versus “extremely confident”, while medication adherence was coded 0 times missed taking medication versus 1+.
Possible Confounders
Demographic variables included age, sex, ethnicity (Indian/ Chinese/Malay/Other), and education (No formal education/ Primary/Secondary and above), and number of prescription medications. Participants were also asked if they had ever been diagnosed by a medical professional with the following conditions: Coronary Artery Disease, Cancer, Hypertension, Diabetes, Chronic respiratory failure, Cerebrovascular Disease, Digestive illness, Renal/kidney or Urinary tract ailments, Arthritis, Chronic back pain, Osteoporosis, Fractures, Cataracts, and Glaucoma, or others.
Statistical Analysis
To summarize participant characteristics, continuous variables were reported as means and standard deviations and categorical variables were expressed as counts and percentages. Logistic regression analyses quantified associations between the fourcategory composite “Care complexity” variable and the two selfreported medication use outcomes described above: medication confidence and adherence. Relationships between the key predictor and outcome variables are summarized as odds ratios in unadjusted logistic regression models and fully adjusted logistic regression models. Adjusted models accounted for differences in age, sex, ethnicity, education, number of medications and number of chronic conditions. A two-tailed P-value of < 0.05 was considered statistically significant. Data were analyzed using Stata 14 SE (Table 1).
Result
This study was a secondary analysis based on a study sample of 1302 older Singaporeans PHASE Wave 3 participants. Table 1 summarizes the demographics, health status, and medication use of study participants. The mean age of participants in the analytic sample was 71 years, with 40% being male. The average number of chronic conditions was 3. A total of 383 participants (24%) reported feeling less than “extremely confident” when asked “how confident do you feel that you are able to take your prescribed medications correctly?” while 309 participants (24%) answered “yes” when asked “At times do you (subject) forget to take your (subject’s) prescription medications?”
Table 1:Demographics characteristics, health status, and medication use*.

health status and medication use based on self-reported responses to PHASE Wave 3 survey
**In last 3 months
In a cross tabulation of number of providers (private general practitioner or a doctor in a public or private hospital or a polyclinic) to healthcare visits seen in the last three months for a health problem they were facing, 746(48%) participants had one visit to a single provider, 193 (12%) had two visits-each to a different provider, and 509(33%) had multiple visits to different providers.
And, 308(20%) reported having no providers and no visits. It was uncommon for participants to report seeing more than three providers or have more than three visits within three months, but some participants reported 5 or more visits or different providers in this timeframe.
Table 2 shows the unadjusted and adjusted estimated odds ratios between the primary combined predictor variable, number of provider and visits, and self-reported confidence in taking medication. Compared to having no provider visits in the past 3 months, having one visit to a single provider (OR=3.05, 95% CI 1.81 - 5.14), two visits-each to a different provider (OR=2.49, 95% CI 1.34-4.65) and multiple visits or providers (OR=2.51, 95% CI 1.62- 5.03), were associated with lower confidence in medication use after adjustment.
Table 2:Relationship between care complexity (number of providers or visits) and low confidence in taking medication.
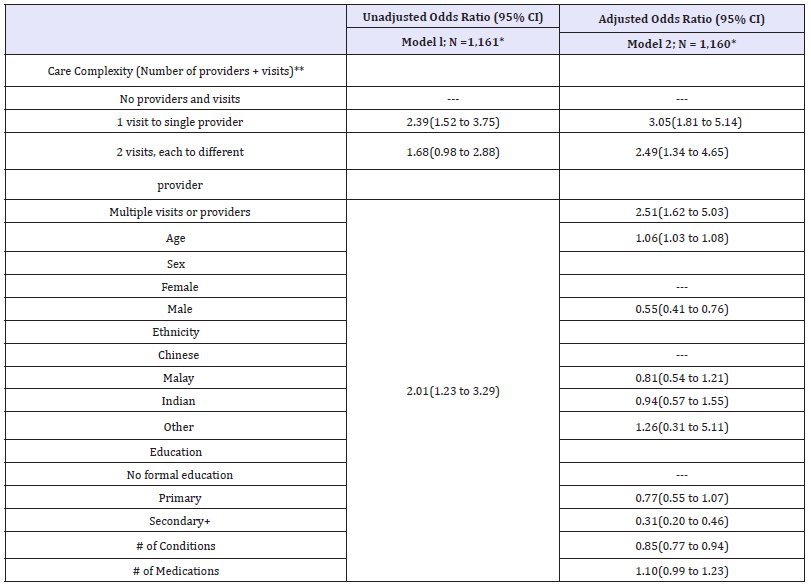
*N after case wise deletion of participants with missing data from one or more variables
**in last 3 months
Table 3:Relationship between care complexity (number of providers or visits) and self-reported medication nonadherence.
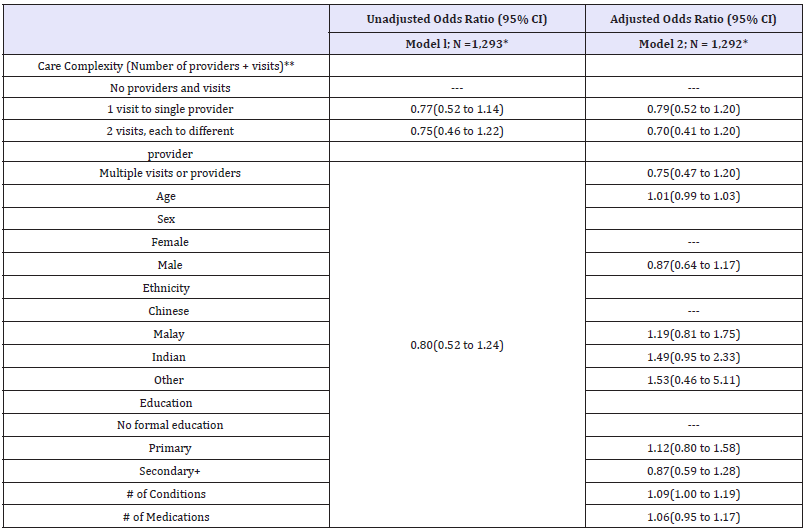
*N after case wise deletion of participants with missing data from one or more variables
**in last 3 months
Table 3 shows the unadjusted and adjusted estimated odds ratios between the combined predictor variable, number of providers and visits, and non-adherence to taking medication. Compared to having no provider visits in the past 3 months, having one visit to a single provider (OR=0.79, 95% CI 0.52-1.20), two visits - each to a different provider (OR=0.70, 95% CI 0.41-1.20), and having multiple visits or providers (OR=0.75, 95% CI 0.47- 1.20), were not significantly associated with non-adherence.
Discussion
In this secondary analysis of a nationally representative survey of older Singaporeans, having high healthcare complexity was associated with lower confidence in medication use, but not with non-adherence to medications.
Some studies have acknowledged the role of self-efficacy or self-confidence in mediating self-reported medication adherence in various HIV or HCV patient populations [10,11]. One study conducted on older Korean patients showed that depression and self-efficacy (or self-confidence) were significant predictors of medication adherence in older patients with hypertension [12]. Although some studies have looked at theoretical models of selfefficacy in the mechanisms of health behaviors change, no known studies have investigated the relationship between care complexity and self-reported confidence in older populations with multiple chronic conditions [13].
There may be many reasons for the lack of association between care complexity and non-adherence in the current study. Most studies published on non-adherence and care complexity largely focus on cardiometabolic conditions such as hypertension, hyperlipidemia, and diabetes. Patients who had increased number of providers had increased number of conditions and increased inpatient admissions [1]. Bedell et al. [10] showed that the majority of patients who failed to take their prescription medication had concerns that focused on the problems of having multiple physicians involved in their care. Using regression models, they found a trend toward medical non-adherence when another physician other than the primary physician was participating in patient care [10]. However, it is important to note that prescription drug therapy is the mainstay treatment for many chronic cardiometabolic conditions [1,10]. In these studies, there was a nonsignificant trend toward increasing discrepancy when the managing physician was a cardiologist rather than an internist [10].
For our study, our participant sample selection was not limited to those with cardiometabolic conditions. We sampled a population with varying degrees of chronic illnesses and morbidity. Patients with significant morbidity burden, whether cardiometabolic in origin or not, often receive referrals to many different specialists or may seek multiple providers to help with their symptoms and concerns. However, elders’ adherence to prescription drugs is also complex and may depend on many medical, personal, and economic factors working synergistically.
Some limitations from our study may further explain why we did not find an association between care complexity and nonadherence. For one, outcome measures were self-reported and may not accurately depict actual medication use behavior, as self-reporting is known to overestimate patient adherence [14]. Second, as adherence in this study was assessed by a dichotomized response to a single survey question, this is subject to recall bias and may be a threat to internal validity. However, previous work has suggested that perfect adherence may be an infeasible goal in people with significant morbidity [15-18].
This study is an initial analysis of patient beliefs in their medication use, But is not able to assess whether self-reported confidence influences adherence to medication, nor the impact on patient outcomes. Although, studies on medication adherence have clearly documented the association between medication misuse and adverse outcomes in both outpatient and inpatient settings [3,7,11,19]. Future study is needed to determine the extent to which patients’ confidence in and compliance with their medication use can be mitigated by novel care methods that promote more coordinated, patient-centered care in patients with multiple outpatient encounters.
Conclusion
The findings from this paper suggest that older patients with multiple providers and visits to providers may be reporting lower confidence about taking their medication; thus older Singaporeans with higher complexity of care may feel uncertain about aspects of medication use. If so, this may suggest an unmet need for education or case management resources to help these individuals. Based on this study, we did not find evidence that adherence was associated with complexity of care. Although older Singaporeans may be less confident with their use of medications, they may still be reporting adherence or compliance to their medications. Thus, providers may consider probing deeper when verifying adherence with their elderly patients since their lack of self-assurance seems to be discrepant with their self-reported actions of adherence. Although the available data do not reveal why some patients felt lower confidence in their ability to take medications correctly, the results indicate that future study to explore this question is warranted.
References
- Maciejewski ML, Powers BJ, Sanders LL, Farley JF, Hansen RA, et al. (2014) The intersection of patient complexity, prescriber continuity and acute care utilization. J Gen Intern Med 29(4): 594-601.
- Marcum ZA, Gellad WF (2012) Medication adherence to multidrug regimens. Clin Geriatr Med 28(2): 287-300
- Pham CB, Dickman RL (2007) Minimizing adverse drug events in older patients. Am Fam Physician 76(12): 1837-1844.
- Wang Y, Lee J, Toh MP, Tang WE, Ko Y (2012)Validity and reliability of a self-reported measure of medication adherence in patients with Type 2 diabetes mellitus in Singapore. Diabet Med 29(9): e338-e344.
- McDonald HP, Garg AX, Haynes RB (2002) Interventions to enhance patient adherence to medication prescriptions: scientific review. Jama 288(22): 2868-2879.
- Higgins N, Regan C (2004) A systematic review of the effectiveness of interventions to help older people adhere to medication regimes. Age Ageing 33(3): 224-229.
- Osterberg L, Blaschke T (2005) Adherence to medication N Engl J Med 353(5): 487-497.
- Tinetti ME, Fried TR, Boyd CM (2012) Designing health care for the most common chronic condition-multimorbidity. Jama 307(23): 2493-2494.
- Goodman RA, Boyd C, Tinetti ME, Von Kohorn I, Parekh AK, et al. (2012) IOM and DHHS meeting on making clinical practice guidelines appropriate for patients with multiple chronic conditions. Ann Fam Med 12(3): 256-259.
- Bedell SE, Jabbour S, Goldberg R, Glaser H, Gobble S, et al. (2004) Discrepancies in the use of medications - their extent and predictors in an out-patient practice. Arch Intern Med 160(14): 2129-2134.
- Page RL, Ruscin JM (2006)The risk of adverse drug events and hospitalrelated morbidity and mortality among older adults with potentially inappropriate medication use. Am J Geriatr Pharmacother 4(4): 297- 305.
- Chan A, Malhotra C, Malhotra R, Ostbye T (2011) Living arrangements, social networks and depressive symptoms among older men and women in Singapore. Int J Geriatr Psychiatry 26(6): 630-639.
- Erlen JA, Cha ES, Kim KH, Caruthers D, Sereika SM (2011) The HIV medication taking self-efficacy scale: psychometric evaluation. J Adv Nurs 66(11): 2560-2572.
- Reif S, Proeschold BRJ, Yao J, Uehara A, Asiimwe E, Quinlivan EB, et al. (2013) Three types of self-efficacy associated with medication adherence in patients with co occurring HIV and substance use disorders, but only when mood disorders are present J Multidiscip Healthc 6: 229-237.
- Son YJ, Won MH (2017) Depression and medication adherence among older Korean patients with hypertension: Mediating role of self-efficacy. Int J Nurs Pract 23(3):
- Schwarzer R, Lippke S, Luszczynska A (2011) Mechanisms of health behavior change in persons with chronic illness or disability: the Health Action Process Approach (HAPA). Rehabil Psychol 56(3): 161-170.
- Riekert KA, Borrelli B, Bilderback A, Rand CS (2011) The development of a motivational interviewing intervention to promote medication adherence among inner-city, African-American adolescents with asthma. Patient Educ Couns 82(1): 117-122.
- Boyd CM, Darer J, Boult C, Fried LP, Boult L, et al. (2005) Clinical practice guidelines and quality of care for older patients with multiple comorbid diseases: Implications for pay for performance. JAMA 294(6): 716-724.
- Malhotra S, Karan RS, Pandhi P, Jain S (2001) Drug related medical emergencies in the elderly: role of adverse drug reactions and noncompliance. Postgrad Med J77(913): 703-707.
© 2018 Ying Guo. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






