- Submissions

Full Text
COJ Biomedical Science & Research
Can the Health Care System Be Effective? - The Research Results
Jasińska J*
Department of Medicine, Poland
*Corresponding author: Jasińska J, Department of Medicine, Poland
Submission: November 13, 2020; Published: December 14, 2020

Volume1 Issue4December 2020
Abstract
The different definitions of efficiency (in their medical meanings) are presented as the result of metareviews found in scientific databases. Efficacy and efficiency are often mismatched with effectiveness in the research of healthcare systems in different countries.In addition to the classic Bismarck’s and Beveridge’s models the modern concepts of health systems include personalized medicine, recognition of health as economic value. However, the basic problem in the Polish healthcare system is the low quality of overly specific and often changed legislation
Introduction
Healthcare is a special area of research and description in the field of change management.
This area is characterized by a particular variety of forms and types of business. Also, changes
in this area, due to the fact that they are closely related to the provision of health services,
are becoming more social than technical or economic. The aforementioned diversity has
certain consequences. They mainly reflect interpretation problems. For this reason, the
following task has been undertaken to organize the scopes of terms, especially the names of
organizations that make up the health services market. For efficient change management in
this area, the organization of names allows, first of all, to precisely define the requirements
for participants of changes. It also facilitates the classification of potential changes. Moreover,
the unification of terminology in healthcare creates an opportunity to look at the system with
greater transparency and facilitates the description of the relationship between individual
elements of the structure of this system, and makes it possible to improve the organizational
system in a situation of financial constraints and the simultaneous need to meet patients’
expectations.
The used term “health protection” is understood as all activities aimed at preventing and
treating diseases, maintaining human biopsychosocial abilities, extending life, ensuring proper
development for new generations and improving the quality of human life. Healthcare creates
the necessary organizational conditions in which scientific and technical achievements can be
optimally used for the benefit of human health. The World Health Organization’s Committee
of Experts suggests adopting the term “Health Care” (the correct translation should be “caring
for health”) to denote an organized action for the health of the public. This term is also used
in our literature interchangeably as “health care”. In other words, health care is a system of
all those activities that are done to prevent, treat and eliminate the consequences of diseases
and to maintain physical, mental and social abilities of people, prolonging life and ensuring
their successful development.
In other words - health protection means a system of all those activities that are performed
to prevent, treat and eliminate the consequences of diseases and to maintain physical, mental
and social abilities of people, prolonging life and ensuring their successful development.
The term “health care” covers almost all human species activities, including education,
culture and the economy. Shortell, Kaluzny distinguish the following components of the
security system health:
a. healthcare - medical medicine,
b. health protection - a set of activities for public health being carried out
c. by various sectors of socio-economic life,
d. healthcare and healthcare management structures,
e. sources and routes of financing all activities for health.
Terminological issues are important when we take into account
the determinants of health according to Lalonde [1]. The impact of
restorative medicine on the health of the population is in the order
of a dozen or so percent, while over 50% are factors dependent
on lifestyle. According to the report Romanow [2], health is not
an individual matter of every citizen, but a common good, which
should result in a specific health policy.
Healthcare organizations are often referred to as being unique,
specific, or at least distinct from other organizations. Moreover,
these differences are considered significant, especially in the field
of change management.
The quoted shortell and Kaluzny mention the following among
the most frequently mentioned differences:
more difficult measurement of work results,
a. Greater diversity in work,
b. The work is more comprehensive,
c. Most of the work is immediate and cannot be postponed,
d. The work allows for a small tolerance of ambiguity or
error,
e. Activities at work are highly independent of each other
and require a high degree of coordination between different groups
of specialists,
f. Work requires an extremely high degree of specialization,
g. Members of the organization are highly specialized and
are more loyal to their professional groups than to the organization,
h. In many health care organizations, there is a dual service
(clinical and administrative) subordination, especially in hospitals,
which can create some coordination and accountability problems
and difficulties due to confusion of competences.
From the above characteristics, the organization of health care is “extraordinary”. These are organizations that have a combination of all of the characteristics listed above. The nature of the specialization, technical skills, substantive values resulting from ethics, professional attitudes pose special challenges to healthcare, and especially to the management of healthcare organizations.
Basic concepts related to health protection
The creator of the world’s first integrated health care system
was Sir Edwin Chadwick (1800-1890). The aim of this system was
to keep employees in the best possible health until old age. Models
of health care systems: Siemaszki, Bismarck and Beveridge were
created much later and are emanations of politics in individual
countries. Bismarck’s model resulted not so much from concern for
the health of citizens as for the votes of voters.
The Beveridge model was an expression of the concept of the
welfare state. While Siemaszko’s model was created in the 1930s,
when infectious diseases (typhus, tuberculosis, Spanish flu), as well
as hunger and living conditions were the main health problems.
These models were “GP based” rather than multidisciplinary teams,
no costly diagnostic procedures, no surgery options, no antibiotics,
no medications psychotropic drugs, interventional cardiology [3].
They fulfilled their role at the cost of low effectiveness in medical
terms, and thus with significant mortality, e.g. due to pneumonia,
which were treated with quinine, lobelin, ephedrine, pyramidone
and expectorants (Medical Calendar 1937). While the Bismarck
and Beveridge models are still being refined, Siemaszki model has
been abandoned. The concept of “health care system” is primarily
equated with health care, especially in terms of financing healing.
“Our healthcare system now instead of focusing focuses on
patient value and focuses on hospital amenities and profits, costcutting
and cost-effectiveness of patient care. These are important
issues, but without focusing on the patient, they lead to waste and
pain. ‘ This opinion is for the US. The “failure of the health care
system” is identified with the indebtedness of hospitals, the long wait
for a “medical service”, that is, de facto with malfunctions related to
treatment. To better understand health care organizations, Mudie,
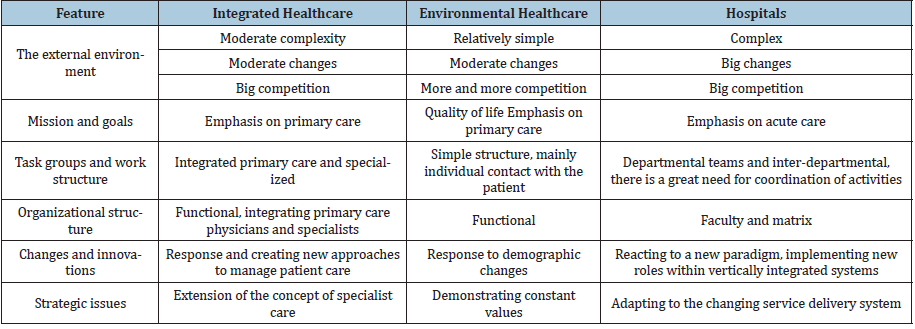
Cottam, Middleton distinguish the following features (Table 1).
Table 1:Features of healthcare organization.
In Poland, the recipe for the health of citizens was to be first the
Health Fund (1920), then the Social Insurance Institution (1934),
after the war: nationalization of hospitals and pharmacies (1948-
1950), industrial medicine (1950s), healthcare teams (1975 ),
independence of health care teams, privatization pharmacies and
open health care (1990s), again Kasa Chorych (quasi-insurance),
commercialization and privatization of hospitals, transfer of
medical treatment to local governments, one payer (NFZ), separate
emergency medical services, benefit baskets, lists of reimbursed
drugs, the Act on activities medicinal. Organizational changes
result from successive legislative changes. It has even come to be
believed that the primary way to solve problems next laws should
be introduced to protect health. In fact, legislation is only the basis
of health policy, which is implemented at various organizational
levels [4].
In recent years, the concept of basing the assessment and
financing of hospital health services depending on the achieved
health effect (value-based purchasing - VBP, pay for performance -
P4P) has become popular, and the erroneous thesis that “imbalance
between the producer of health services and the consumer is so
huge that in most cases you can sell him anything at any price ”he
still has his supporters. Just like the assumptions that the health
needs of the population are unlimited, and the introduction of an
electronic patient card will simplify the work of doctors and even
solve the problems of queues. It was only “the COVID-19 crisis
made many European societies realize that the health care systems
in force in their countries are ineffective and do not work”.
Therefore, questions arise whether the health care system
can be effective as a whole, what is the methodology for assessing
the effectiveness of the system, what are the legal causes of the
current failures of the health care system in Poland, and are these
phenomena occurring in countries other than Poland? The aim of
the study was an attempt to determine the current state of research
and theoretical concepts regarding the effectiveness of health
care systems as well as the legal and structural conditions for the
effectiveness of the system, with particular emphasis on Poland.
Material and Methods
Medical (PubMed, High Wire Press, Cochrane Collaboration)
and multi-specialist (EBSCO, Springer link) Internet databases
were reviewed to determine the theoretical basis for measuring the
effectiveness of the health care system (as a whole). The keywords
were: effectiveness, efficiency, efficacy, health care system. The
inclusion criteria were publication in professional journals, the
Evidence Based Medicine methodology, analysis of the entire health
care system, and numerical data on health outcomes.
The exclusion criteria were works related to specific issues, e.g.
effectiveness in various disease entities, works that do not meet
the EBM criteria and works older than 10 years - due to legislative
changes that have occurred in the last decade. An attempt was also
made to evaluate the determinants influencing the effectiveness of
healthcare in Poland, based on the legal acts included in the ISAP
database. Official statistical data on the structure of health care and health protection contained in the materials of the Central
Statistical Office in Poland (2018) were also used.
Results
The terms “health care system” and “health care system” - distinguished in Polish literature - in Anglo-Saxon terminology are referred to as health system or healthcare system. The database review results for keywords and for the phrase “effectiveness of health care system” are presented in Table 2.
Table 2:Database review results.
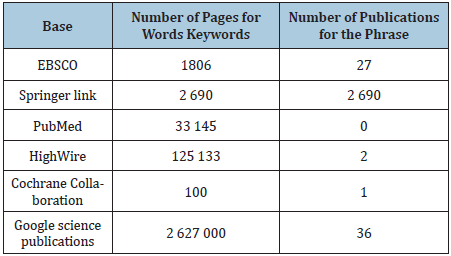
Only 2 publications meeting the search criteria were found in medical databases, while in the EBSCO database - 27 items. In the Cochrane Collaboration database, only one work (meta-review) concerned the methodology for assessing the effectiveness of the health care system. The obtained results indicate significant methodological difficulties in assessing the effectiveness of the health care system. The results of searching for legal acts according to entries in the Polish Internet System of Legal Acts (ISAP) are presented in Table 3.
Table 3:
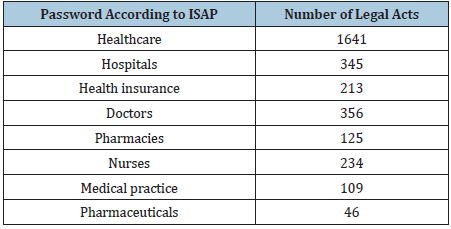
The search results in the ISAP system include both current and
obsolete acts. Apart from the acts and resolutions of the Parliament,
there are: related acts, repealed acts, acts deemed repealed,
implementing acts, amending acts, amended acts, European
directives, references. There are laws often amended, which does
not reflect the quality of the law, e.g. the Act on health care services
financed from public funds (2004), amending 43 other legal acts,
was amended (after the adoption of a consolidated text in 2018)
31 times in less than 4 years. Law on medical activity, repealed 12
other acts, was amended 4 times in 2 years, and regulates many overly detailed issues, e.g. standards working time of employees
of healthcare entities (as if the labor law did not exist). Some legal
acts regulate in detail obvious matters, such as the ordinance of the
Minister of Health “on the procedure of a medical entity performing
stationary and 24-hour medical activities health services with the
patient’s remains in the event of death. patient “or the ordinance of
the Minister of Health” on the detailed scope of powers and duties
of the medical emergency coordinator “ orders the preparation of a
report on the 24-hour on-call duty.
The “health care system”, especially in Poland, requires changes,
as 795 hospitals, 16 60 815 health care centers, 79 337 doctors,
184 748 nurses, 6 927 medical practices, 11 297 pharmacies and
10 medical universities with 42 clinical hospitals separately pursue
their sub-goals.
In the literature, medical personnel (especially doctors) are
often treated as a homogeneous group, forgetting about 70 types of
medical specialties, 12 nurses, as many as pharmaceuticals and 23
types of medical professions. Designing a system that consists of all
the above structures (including personnel) is an extremely difficult,
if not impossible task. Moreover, the effectiveness of the system
is assessed based on the number of services provided (“health
services”: 7,344,000 hospitalizations, 290 million consultations,
42% of which in specialist clinics 7.4 advices per capita) negative
health indicators (mortality, morbidity) and financial outlays of
PLN 100 billion annually
Discussion
Research on health care systems reflects concepts that are not
necessarily consistent. Apart from the two main models of health
care (Bismarck versus Beveridge), one can distinguish the concept
of “salutogenesis” (as a development of personalized medicine
combined with preventive action) [5].
Personalized medicine (patient-oriented medicine) is based
on an individual approach to the patient, using genetic testing as
opposed to evidence-based medicine (EBM), which refers to the
results of population studies [6]. Care optimization projects based
solely on economic criteria are common [7] or the belief in the
effectiveness of computerization [8].
Successive concepts combine efficiency health system with
quality [9]. Of the 414 publications found by Rockers et al. [10] -
259 met the inclusion criteria, 50% of the analyzes were limited
to the results of controlled studies, and 68% were based on the
EPOC (Effective Practice and Organization of Care) criteria. Overall,
the authors considered it necessary to conduct further research
on the criteria used in the study of health systems, provided
that increasing the number of criteria must not compromise the
reliability of the research [10], Shah et al. [11] in a work devoted
to the effectiveness of actions for Health Impact Assessment shows
that out of 51 programs, only eight achieved improvement in QALY,
while in 18 other health benefits were identified, some programs
did not allow cost-benefit assessment. Resource allocation decisions are made differently by the Department of Health and the
National Institute for Health and Clinical Excellence (NICE), leading
to financial ineffectiveness of programs. Methodological difficulties
in assessing the quality of life underlined by Paz et al. [12].
The tools used for this purpose (SF-36, HUI, EQ-5D, QWB-SA,
HALex, MLHFQ, NEI-VFQ-25) are, to a limited extent, suitable for
assessing the quality of life of the general population. Vest and
Gamm [13] assessed the effectiveness of healthcare transformation
in the US based on 9 publications that met the inclusion criteria,
using Six Sigma, Lean / Toyota Production System, and Studer’s
Hardwiring Excellence. Authors state that due to methodological
limitations, the results of 9 studies may be questioned because
of study design errors, inappropriate analyzes and failures in
excluding alternative hypotheses.
Eccles et al. [14] state that the theoretical foundations are not
used in implementing effective clinical practice in the UK NHS.
Many politicians recognize that conducting comparative research
on the effectiveness of health protection can reduce waste in the US
health care system. For this purpose, Hoffman et al. [15] propose
the concept of “marginal medicine” (analogy to marginal costs)
consisting in the development of guidelines for the selection of the
best health options. However, the underlying problem is the scarcity
of data both in observational studies and in developing evidence of
efficacy. The question arises whether various specialists dealing with
this problem can develop sufficiently accurate measurement tools?
A possible solution is to develop assessment tools effectiveness of
individual actions for the health of the population [16].
Tenbensel et al. [17], based on data from the Health Policy
Monitor in 11 developed countries, showed that better health
outcomes (outcomes) are obtained:
a. in tax-financed health systems,
b. when the center-left dominates the government,
c. when social security-based systems are more concerned
with cost reduction and economic efficiency. On the other hand,
the political composition of the government is not the main factor
shaping the health policy of the state. It is only from 2019 that the
role of initiatives targeting societies, assessing accessibility and
equality, and health effects on the population due to the COVID -19
pandemic, increases [17].
Thus, unlike research on the effectiveness of healthcare on
selected groups of patients, research on the effectiveness of
healthcare systems is few. This is mainly due to from methodological
difficulties, the complexity of the problem, and political conditions.
Only in recent years, and especially in 2020, has there been a greater
interest in the effectiveness of health care systems at the national
and international level, although some of the concepts presented
are a return to the ideas from the 19th and 20th centuries [18-23].
1. Determining the effectiveness of the health care system
requires overcoming numerous methodological problems, the solutions of which require further research with the
participation of multidisciplinary teams.
2. The problem of the effectiveness of health care applies to both
developed and developing countries. It does not only result
from the limited financial resources allocated to health care.
3. For many years, in the Polish health care system, there has
been a tendency to solve all problems by means of excessively
detailed and frequently amended legal acts, with insufficient
funding and underestimating the role of partners from various
professional groups [24-28].
4. In transforming healthcare, the specificities of the sector
must not be underestimated. These specific features include
the relationship between the doctor, nurse and patient, the
right to professional change of care and information about
it. It is also about health needs and the right of equal access
to medical services, possibly with limitations, but this is an
undisputed principle. For health is a private good as well as a
public good. It is very difficult to establish boundaries between
them. However, even serious difficulties cannot justify
unprofessionalism in carrying out changes. The advantages of
party interests over the public interest and the advantages of
certain groups of medical professions over others, and even
more so of the medical community over the interests of the
patient [29-33].
5. Managing efficiency in healthcare requires knowledge,
substantive preparation and prudence. The current changes
consisting in centralizing decisions in a situation of great
difficulties caused by the COVID-19 pandemic can be treated
as a kind of system rationalization attempt [34-37].
Centralization in a COVID -19 crisis situation is sometimes
necessary. However, as a permanent solution, it is irrational and
socially dangerous. It is a solution of the type of “enlightened
absolutism” based on discretion, based on the assumption that
one authority is better than independent units operating in a
coordinated system.
References
- Lalonde M (1974) A new perspective on the health of Canadians.
- Romanow R (2016) Building on values. The future of health care in Canada.
- Dart RC (2011) Can lean thinking transform American health care? Ann Emerg Med 57(3): 279-281.
- Ryś A (2017) Crisis, or time for changes. Health Manager 6.
- Alivia M, Guadagni PP, di Sarsina PR (2017) Towards salutogenesis in the development of personalized and preventive healthcare. EPMA Journal 2(4): 381-384.
- Clark DA (2015) The end of evidence-based medicine? Inflammopharmacol 20(4):187-193.
- Baranowski J, Windak A (2017) Optimization of the Polish primary healthcare financing system. Efficient State. Program Erenst & Young, Warsaw, Poland.
- Chaudhry B, Wang J, Wu S, Maglione M, Mojica W, et al. (2016) Systematic review: Impact of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med 144(10): 742-752.
- Arah OA, Klazinga NS, Delnoij DMJ, Asbroek AHAT, Custers T (2013) Conceptual frameworks for health systems performance: A quest for effectiveness, quality, and improvement. International Journal for Quality in Health Care 15(5): 377-398.
- Rockers PC, Feigl AB, Røttingen JA, Fretheim A, de Ferranti D, et al. (2015) Study-design selection criteria in systematic reviews of effectiveness of health systems interventions and reforms: A meta-review. Health Policy 104(3): 206-214.
- Shah K, Praet C, Devlin N, Sussex J, Appleby J, et al. (2018) Is the aim of the English health care system to maximize QALYs? Journal of Health Services Research & Policy 17(3): 157-163.
- Paz SH, Liu H, Fongwa MN, Morales LS, Hays RD (2019) Readability estimates for commonly used health-related quality of life surveys. Qual Life Res 18(7): 889-900.
- Vest JR, Gamm LD (2019) A critical review of the research literature on six sigma, lean and studergroup's hardwiring excellence in the United States: The need to demonstrate and communicate the effectiveness of transformation strategies in healthcare. Implementation Science 4: 35.
- Eccles MP, Armstrong D, Baker R, Cleary K, Davies H, et al. (2019) An implementation research agenda. Implementation Science 4.
- Hoffman A, Pearson SD (2019) ‘Marginal medicine’: Targeting comparative effectiveness research to reduce waste. Health Affairs 28(4): 710-718.
- Kansagra SM, Farley TA (2016) Public health research: Lost in translation or speaking the wrong language? Am J Public Health 101(12): 2203-2206.
- Tenbensel T, Eagle S, Ashton T (2017) Comparing health policy agendas across eleven high income countries: Islands of difference in a sea of similarity. Health Policy 106(1): 29-36.
- Borg MA (2010) Are healthcare economics a factor behind European MRSA rates? Eur J Clin Microbiol Infect Dis 29(4): 477-479.
- Box GEP, Draper NR (2017) Empirical model-building and response surfaces. John Wiley & Sons, New Jersey, USA.
- Brown PM (2014) Personalized medicine and comparative effectiveness research in an era of fixed budgets. EPMA Journal 1(4): 633-640.
- Coffman JM, Hong MK, Aubry WM, Luft HS, Yelin E (2019) Translating medical effectiveness research into policy: Lessons from the California health benefits review program. The Milbank Quarterly 87(4): 863-902.
- Costigliola V (2018) Healthcare overview: Global process of personalization in medicine. EPMA Journal 1(4):525-528.
- Cvetanović S (2017) On economic evaluation of health care. Scientific Journal of the Faculty of Medicine in Niš 28(3).
- D’Amore JD, Sittig DF, Ness RB (2016) How the continuity of care document can advance medical research and public health. American Journal of Public Health 102(5): e1-4.
- Döring A, Friedemann P (2010) The German healthcare system. EPMA Journal 1(4): 535-547.
- Suchecka J (2017) Healthcare financing. Selected Issues. ABC Wolters Kluwer, Warszawa, Poland.
- Frączkiewicz-Wronka A, Jasłowski J, Owcarz-Cydzik B, Sobusik D (2018) Local government health policy. Katowice, Poland.
- Grosios K, Gahan PB, Burbidge J (2017) Overview of healthcare in the UK. EPMA Journal 1(4):529-34.
- GUS (2018) Polska w liczbach.
- http://isap.sejm.gov.pl/
- Kornai J (2017) Niedobór w gospodarce. Polish Economic Publishing House, Warszawa, Poland.
- Li SC (2017) Pharmacoeconomic evaluation in rheumatology an introduction to pharmacoeconomic evaluation in rheumatology. APLAR Journal of Rheumatology 6(2): 192-200.
- Matuszak-Flejszman A (2011) Effectiveness and efficiency of environmental management systems.
- Mazur M (1987) The concept of the system and the rigors of its application. Advances in Cybernetics 2.
- Miller M, Zieliński A (2017) Public health-mission and science. Epidemiological Review 56(4): 547-557.
- http://www.cbc.ca/healthcare/final_report.pdf.
- Ruszkowski J (2018) Polish health system - socialism in a market environment. In: Health protection and economy. Market mechanisms and public regulations. Warszawa, Poland.
© 2020 Jasińska J. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






