- Submissions

Full Text
COJ Biomedical Science & Research
Areflux Nutritious Junostoma
Martynov VL*, Kolchin DG, Kurilov VA and Trukhalev VA
GBUZ NO, Russia
*Corresponding author: Martynov VL, GBUZ NO, Russia
Submission: July 01, 2020; Published: August 28, 2020

Volume1 Issue2July 2020
Abstract
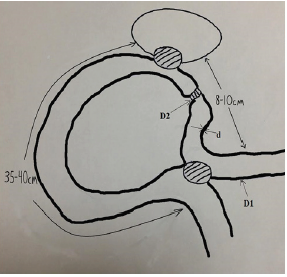
In case of internal drainage of abdominal cavity and retroperitoneal cavity formations, a “plug” was developed for the leading loop of the small intestine, which eliminates compression, ischemia and necrosis of the intestinal wall with subsequent migration of the created structure into the gastrointestinal tract and leveling the planned effect. We form a “stub” on the small intestine according to the developed technique, in which compression and necrosis of its wall with subsequent migration of the structure into the intestinal lumen are excluded (Figure 1).
Figure 1: Scheme of drainage of the cavity formation of the abdominal cavity or retroperitoneal space using a “plug”.
During the operation, the diameter of the small intestine section (D1), the wall thickness of the small intestine (d), where it is planned to perform a “stub”, are determined. Upon receipt of the desired parameters by the formula D2 = 2√D1d - the required diameter of the corrugated portion of the small intestine (D2) is calculated, after which the intended stage of the operation is performed (Figure 2).
Figure 2: Scheme and formula for applying an areflux “plug” to the adductor loop during drainage of the cavity formation.
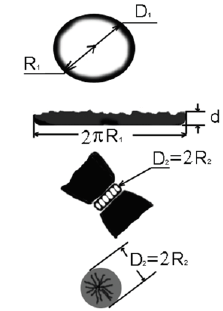
d-wall thickness of the small intestine; R1 is the radius of the small intestine; R2 is the radius of the corrugated portion of the small intestine; D1 is the diameter of the small intestine; D2 - diameter of the corrugated portion of the small intestine with a “plug”; 2P R1 is the cross-sectional area of the small intestine stacks; S1 is the cross-sectional area of the wall of the small intestine; S1 = 2ΠR1d = D1Пd; S2 is the cross-sectional area of the corrugated wall of the small intestine; S2 = Π R22 = Π (D2/2) 2; S1 = S2 - a condition for the absence of compression and necrosis of the wall of the small intestine in the area of the stub; D1Pd = Π (D2/2) 2; D2/2 = D1d; D2 = 2√D1d - the desired diameter of the corrugated portion of the small intestine with a “stub” - (Patent No. RF 2253379. Registered in the State Register of Inventions of the Russian Federation 10.06.2005). “Method for creating a “stub” on the adducting loop of the small intestine during internal drainage of abdominal cavity formations”.
Creating Nutritious Areflux Junostoma
Eating disorders in the postoperative period significantly reduce the effectiveness of treatment, increase the risk of developing septic and infectious complications, increase the length of hospital stay, and worsen mortality rates [1,2].
Tumor stenosis and cicatricial strictures of the esophagus lead to obstruction of the proximal digestive tract with the development of nutritional deficiency, exhaustion and extinction of the compensatory capabilities of the body, which leads to the rejection of the simultaneous formation of an artificial esophagus in patients of this category. For this category of patients, the use of long-term enteral nutrition through the areflux stoma [3], as the most physiological, causing fewer complications and economically viable method [4], is receiving increasing attention. The frequency of development of purulent mediastinitis with esophageal perforation reaches 80%, and mortality - 40-45%. The main task is to stop the flow of the esophagus lumen into the mediastinum, which determines the relevance of the nutritional stoma in these patients.
The use of nonintentional sounding entails formidable complications-the formation of acute stomach ulcers and 12-PK, including those complicated by bleeding. The leading method for preventing such complications is the use of proton pump blockers, which leads to a decrease in hydrochloric acid production. The negative side of this therapeutic effect is a significant increase in the degree of bacterial contamination of the upper gastrointestinal tract in combination with a change in the microbiological landscape. Under these conditions, the presence of a foreign body (probe) in the esophagus and oropharynx, as well as the inability to seal the esophagus sphincter tightly, create favorable conditions for translocation of pathogenic microorganisms into the trachea and bronchi. The result of the above pathological processes is an increase in the frequency of nosocomial pneumonia.
A jejunostomy can be performed as a stage of an operation and as an independent operation from a small laparotomy incision. Schematically, the essence of the developed jejunostomy is as follows (Figure 3):
- Choose a loop of the small intestine for jujunostomy.
- Form an anastomosis between the adducting and abducting parts of the intestine 15-20cm from the area of the jejunostoma.
- In 4-5cm from the inter-intestinal anastomosis on the adducting loop of the intestine we impose a “plug” according to the developed method.
- Through the center of the purse string suture, we introduce a drainage tube or probe 15-20cm behind the anastomosis into the outlet loop of the intestine.
- We fix the loop of the intestine with the stoma in the front wall of the abdomen (Figure 4).
- Through the drainage tube or probe on the first day we introduce nutrient mixtures.
Figure 3: The scheme for creating areflux nutritional jujunostomy according to the developed method.
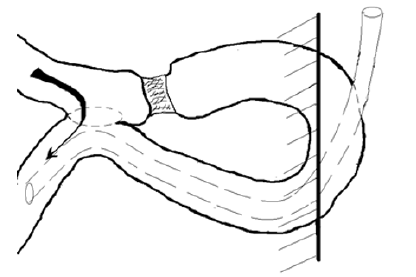
Figure 4: Areflux nutrient jujunctoma formed.

References
- Zybin KD (2017) An individual approach to providing nutritional support for patients with acute pancreatitis. Bulletin of Surgical Gastroenterology 2: 28-30.
- Rodoman GV (2017) Optimization of early enteral nutritional support after gastrectomy. Surgeon 1: 9-16.
- Marco B (2001) Early postoperative enteral nutrition improves gut oxygenation and reduces costs compared with total parenteral nutrition. Crit Care Med 29: 242-248.
- Nicola W (2003) Nutrition support to patients undergoing gastrointestinal surgery. Nutr J 2: 1-5.
© 2020 Martynov VL. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






