- Submissions

Full Text
Cohesive Journal of Microbiology & Infectious Disease
The Influence of Probiotics on the Health of Patients Infected With HIV
Gisele Pantoja Costa1, Jeane Gomes da Silva1, Antonio Carlos Freitas Souza1 and Anderson Luiz Pena da Costa1,2*
1Macapa Institute of High Education-IMMES, Faculty of Pharmacy, Jovino Diona Street, Brazil
2Federal University of Amapa-UNIFAP, Post-Graduation Program in Pharmaceutical Innovation (PPGIF), Brazil
*Corresponding author: Anderson Luiz Pena da Costa, Macapa Institute of High Education- IMMES, Faculty of Pharmacy, Jovino Diona Street, Brazil
Submission: June 26, 2022; Published: August 10, 2022

ISSN 2578-0190 Volume6 issues1
Abstract
People infected by the HIV virus do not just have their immune system impaired; their gastrointestinal tract has been recognized as one of the most damaged sites by the infection, and treatment for it can enhance these patients’ quality of life. Therefore, this study aims to address the influence of probiotic supplementation on the health of HIV serum positive patients through a literature review using articles published between 2015 and 2020 that are available in the virtual libraries Scielo, PubMed, and CAPES. This research shows that using probiotics can have beneficial results for HIV serum positive patients. Improvement of dysbiosis with the restoration of the intestinal microbiota, decreases in systemic inflammation, microbial translocation, and improvement in immunological and neurocognitive functions are among the benefits reported in this review, suggesting probiotics may be a low cost and effective support therapy to delay the onset and aggravation of morbidities related to HIV infection.
Keywords:Probiotics; Acquired human immunodeficiency syndrome; Infectious diseases; Immunomodulation; Inflammation
Introduction
The Human Immunodeficiency Virus (HIV) is an infectious agent belonging to the Retroviridae family, genus Lentivirus, inserted in group VI of the Baltimore classification system because it has a genome composed of single-stranded positive sense, which produces intermediate double-stranded DNA produced by the reverse transcriptase enzyme, and then this genetic material is inserted into the host genome to produce viral particles [1]. This virus infects lymphocytes T CD4 +, which are important cells in the presentation of antigens for the subsequent production of antibodies by lymphocytes B, which generate immunity against various infectious agents; in addition, at advanced stages, HIV can also infect microglia, which are cells responsible for the central nervous system’s immune defense [2].
Thus, by reducing important cells populations of immune system, HIV infection alters immune function by causing damage in the gastrointestinal epithelium, which releases endogenous inflammatory mediators, as well as allowing the translocation of enteric microorganisms and their metabolites [such as lipopolysaccharides] for the systemic circulation, where they can activate chronic low-intensity inflammatory responses, which beside interfere in the cellular signal transduction, also act as risk/aggravating factors for metabolic and cardiovascular diseases [3].
In this sense, there is evidence that changes in the composition of enteric microbiota play an important role in regulating and maintaining homeostasis, not only in the gastrointestinal system but also in the homeostasis of other organ systems, primarily influencing immune function, in which high levels of bacterial translocation are linked to endotoxemia and lowintensity inflammation, whereas normalization of microbiota is linked to health status [4]. Thus, this study examines the impact of probiotic consumption [live bacteria that, when consumed in appropriate amounts, have favorable impacts on an individual’s health [5] on the health of HIV/ AIDS patients.
Materials and Methods
This literature study was conducted using papers available in Scielo, PubMed, and CAPES that reported the findings of clinical investigations on the effects of probiotics on the health of HIV patients. The bibliographic search was conducted using the descriptors HIV and probiotics, considering publications from 2015 to 2020, where the descriptors appeared in the title and abstract. Articles presenting clinical research in humans, published between 2015 and 2020, with full text available in electronic format, were considered for inclusion. Non-pertinence to the theme, thesis, chapters of thesis, books, book chapters, material published in annals of event, conferences, technical reports, case reports, review articles, institutional publications, and in vitro investigations were excluded.
Following the bibliographic search, the articles that met the inclusion criteria were manually analyzed, taking into account the clinical study design, the size of the cohorts in each study, morbidities [if present], and impacts on clinical and laboratory parameters that indicate attenuation or worsening of HIV infection, in order to provide information that can improve clinical research and the prescription of probiotic to patients with HIV infection.
Results and Discussion
Bibliographic survey
The search strategy used in the survey of articles with the descriptors HIV and Probiotics yielded 122 papers in the PubMed directory, 1754 papers in the CAPES database, and 0 papers in Scielo, for a total of 1876 papers, which were then analyzed for inclusion and exclusion and duplicate detection, yielding the selection of 12 works and the exclusion of 10. In terms of the number of publications across the period chosen, 2017 had the most (5 articles), followed by 2015 (3 articles), and 2016 (2 articles), while the years 2018, 2019, and 2020 each had only one publication in the survey. These findings imply that the scientific community is interested in the topic; nonetheless, few human clinical research have been undertaken between 2015 and 2020.
In this context, the low number of clinical studies on the effects of probiotics on the health of HIV/AIDS patients can be attributed to a variety of factors, including high costs for conducting clinical trials [6], ethical and legal aspects that regulate the conduct of human research in different countries [7], and technical difficulties in maintaining cohorts and administering treatments [8], as well as the COVID-19 pandemics that initiated as an outbreak in December 2019 at Chine and then was declared a pandemics by the world health organization on Mach 11, 2020, causing more than 350,00 death worldwide by the end of May 2020 [9]. Moreover, The COVID-19 pandemics have also caused economic, social, and political disruptions, with implications for education and research development. That may interfere in the conduction of clinical research outside the scope of COVID-19 prevention and therapeutics for the next years [10].
Methodological aspects of the selected studies
In the bulk of the articles evaluated 6 featured a randomized double-blind methodological design, 3 were longitudinal studies, 2 presented prospective approaches, and 3 were pilot studies. Table 1 shows the methodological characteristics of each selected study. In this sense, it’s worth mentioning that each type of clinical investigation has benefits and drawbacks, both in terms of logistics and the inferences and conclusions that can be drawn from the findings [11]. A randomized clinical trial is a gold standard for establishing the effectiveness of a therapy in this setting. When there is uncertainty about the effect of an exposure or treatment, and the exposure may be changed in the study, this form of study is chosen [12]. However, this type of study has possible limits in terms of generalizations about the study population and environment.
Table 1:Methodological aspects of the selected clinical works.

A pilot study is a “small version of the whole study” that allows you to test the applicability of all of the method’s instruments and methods, as well as make any necessary adjustments for definitive data collection [13]. Conducting a pilot study is important because it allows you to test, evaluate, examine, and improve research tools and techniques. This type of study is conducted to identify potential flaws and difficulties so that they can be addressed before to the research’s adoption. It is crucial for research since it might disclose minor faults in the project’s design or implementation that would otherwise go unnoticed in the research plan [14]. Moreover, the clinical research can be of the type single-center study, when they are all affiliated with the same research institution, or a multicenter study when there is an integration of different institutions while conducting the research. In this sense, when neither the patients, team members nor the personnel who deal with patient’s knowns whether they are using a placebo or the experimental drug, the research is classified as a double-blind study, only one team member is aware of who belongs to which group. This person, on the other hand, will not be dealing with patients or evaluating the results. Each group is exposed only after the conclusion of the study. To eliminate bias, the treatment and placebo controls in this sort of trial should have the same physical appearance [15].
Figure 1:Dysbiosis at the gastrointestinal tract promoted by HIV infection.
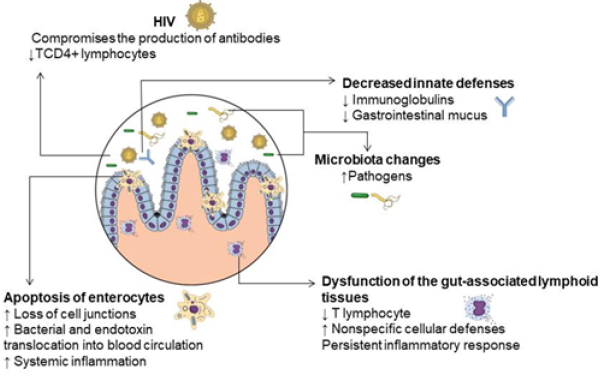
The selected clinical studies were generally concerned with the effects of dysbiosis, which is defined as an imbalance of the gastrointestinal microbiota that causes the epithelium to become permeable to microorganisms and their metabolites, resulting in changes in various physiological processes related to the endocrine, neurological, and immunological axes, as well as persistent inflammatory conditions induced by the accumulation of damage to the gastrointestinal epithelium, and changes in the transduction of signals involved in the body’s endogenous regulation [16]. In figure 1, the features of dysbiosis at the gastrointestinal tract promoted by HIV infection are illustrated to improve text comprehension.
In the longitudinal pilot clinical research with 20 HIV-infected patients and 11 healthy patients, D’ettore et al. [17] showed that probiotics had a favorable effect on HIV-infected patients during antiretroviral treatment, enhancing the microbiota and lowering mucosal and systemic inflammation. However, more research on the effects of probiotics on lymphoid tissue associated with the intestine is needed to better understand the link between immunological activation and the maintenance of plasma viremia suppression in patients with totally suppressed plasma viremia.
Villar-Garca et al. [18] conducted a randomized, double-blind, placebo-controlled study in 44 chronic HIV-infected patients with an undetectable plasma viral load to see if the beneficial effect of Saccharomyces boulardii is due to a change in the composition of these patients’ intestinal microbiota, with a decrease in some species associated with higher systemic levels of microbial translocation and inflammation. This was the first clinical investigation to use 16S rDNA sequencing to examine changes in the intestinal microbiota following therapy with Saccharomyces boulardii, as well as how these changes are linked to microbial translocation and inflammation in HIV patients.
As a result, Villar-Garca et al. [18] found alterations in the makeup of the intestinal microbiota after treatment with the probiotic [S. boulardii], with a decrease in particular species that are directly linked to systemic levels of microbial translocation and inflammation. Suggesting the introduction of probiotics as a novel therapeutic approach for HIV patients should be considered in the clinical practice.
Furthermore, Storm Larsen et al. [19] conducted a doubleblind clinical trial with 22 people (10 using probiotics and 12 as controls) to investigate if bacterial lipopolysaccharides from the gastrointestinal tract are related to the chronic inflammation seen in HIV-infected individuals by addressing with metagenome analysis the degree of acylation of lipopolysaccharides from the guts in the plasma using the PiCRUSt software to predict the overall functionality of the microbiota of HIV-infected individuals and distinguish those bacteria producing the hexaacylated polysaccharides and those producing the penta-acylated polysaccharides, and then evaluate the effect of these metabolites in pathways related to inflammation as the catabolism of tryptophan by correlating it with the inflammation biomarker neopterin, and the effect of a probiotic intervention.
In the conclusion of the study, Storm LC et al. [19] had as a result high levels of inflammation [neopterin] associated with high levels of tryptophan catabolism, suggesting a link between systemic inflammation and the catabolism of this amino acid, and it was also found a higher rate of hexa-acylated lipopolysaccharide bacteria producers over those hexa-acylated lipopolysaccharide producers in HIV-infected individuals. And concerning the treatment with probiotics, the researchers concluded that it contributed to a decrease in gram-negative bacteria associated with the overall biosynthesis of lipopolysaccharides which was primarily related to the noninflammatory penta-acylated lipopolysaccharidesproducing gram-negative bacteria.
Scagnolari et al. [20] conducted a longitudinal pilot study in HIV-1-serum positive male patients treated with combined antiretroviral therapy with long-term viral suppression to assess the effects of a high concentration of probiotic on the levels of neopterin in Cerebrospinal Fluid (CSF) and the expression of Indoleamine 2,3 Dioxygenase (IDO) mRNA in the intestinal Lamina Lymphocytes (LPLs). Probiotics and combined antiretroviral therapy supplementation dramatically lower IDO mRNA expression in Gut- Associated Lymphoid Tissue (GALT), and according to the findings, before probiotic administration, there was a positive connection between GALT IDO mRNA and CSF neopterin (inflammation) levels. Thus, this study shows that probiotic products can lower the activation of the IDO pathway, potentially breaking the gut-brain vicious circle and preventing the neurocognitive damage reported in HIV-1 patients.
In this regard, Ceccarelli et al. [21] conducted a pilot study and analyzed the effect of supplementation with high concentration probiotics on various neurocognitive abilities as well as the safety of this supplementation in HIV-positive patients on antiretroviral therapy with long-term viral suppression. As a result, they found that HIV-positive patients who took a probiotic formulation twice a day for six months improved significantly in some neurological cognitive functions [short and long memory, abstract reasoning], proving that changes in the intestinal microbiota can provide specific neurological benefits in HIV patients without significant side effects.
And in a pilot, double blinded study conducted by Sainz et al. [22] examined the gut microbiota of children infected vertically by HIV and assessed the possibility of modifying it through a dietary intervention utilizing pre and probiotics. This was the first study to examine the impact of a brief dietary intervention on the microbiome of HIV-infected children who were vertically infected. As a result, they observed that the microbiota of HIVinfected children presented lower alpha diversity when compared to controls, also presenting distinct beta diversity, with increase of the genus Prevotella, Akkermansia, Escherichia and abundance of Faecalibacterium, and the intervention with probiotic led the microbiota composition of HIV-infected children to parameters close to the uninfected control group. supplement twice daily for 6 months to assess the safety and efficacy of probiotic supplementation, choosing a mixture of high concentration multi-strain probiotics widely used in inflammatory bowel disease for supplementation of patients on antiretroviral therapy. Their findings suggested that supplementing antiretroviral therapy with a probiotic mixture in HIV-1 infected individuals may favor the restoration of commensal intestinal microbiota composition, triggering a series of immunological and intestinal physiology repair processes.
T cell activation was found to be significantly reduced in both peripheral blood and GALT, the probiotic improved the integrity of the intestinal epithelial barrier, and the probiotic improved mitochondrial morphology by relocating the mitochondrial chaperonin, HPS60, from the cytosol to the mitochondrial compartment. Finally, treatment with probiotics resulted in a clear and significant reduction in levels of systemic immunological activation in CD4 + or CD8 + T cell subsets, as indicated by the CD38 + and HLA-DR + markers.
In a prospective study involving 60 HIV-infected children, 31 of whom did not use antiretroviral therapy and 29 of whom received antiretroviral therapy for a median of 3.5 years, Ishizaki et al. [24] investigated the short-term effects of the probiotic strain Lactobacillus casei Shirota (LcS) on the immunological profiles and intestinal microbial translocation among children infected with the human immunodeficiency virus. The study also included 20 children with no HIV infection as control; and the findings revealed that LcS use was safe for HIV-positive children. Furthermore, infected children demonstrated considerable increases in CD4 + cells, particularly the Th17 subset, as well as significant decreases in activated CD8 + cell percentages after ingestion. Moreover, after ingesting LcS, the number of peripheral CD4 + T cells in children with HIV grew considerably. Indicating the ingestion of LcS may be a useful supportive therapy for HIV-infected youngsters.
And in different research aiming to assess the effects of a highconcentration lyophilized probiotic supplement on the Type I and II Interferon (IFN) response in HIV-1 infected patients, Pinacchio et al. [25] conducted a pilot, single-arm, non-randomized clinical study with 10 HIV-infected patients who received a high-concentration lyophilized probiotic supplement. The study found that probiotic supplementation modified the levels of IFN, IFN subtypes, and IFN transcription, as well as the expression profile of the IFN subtype. In both the GALT and the Peripheral Blood Mononuclear Cells (PBMC) of HIV-1-positive individuals, IFN 6, IFN 10, IFN 14, IFN 17, and IFN 21 increased considerably following treatment with probiotics.
In this sense, Falaska et al. [26] also evaluated the antiinflammatory features of probiotics strains in a four-week prospective trial including 30 HIV-positive men who were on continuous antiretroviral medication and were given a bottle of fermented milk Yakult Light® containing Lactobacillus Casei Shirota (LcS) twice daily. As a result, they observed significant decrease in the expression of the cytokine TGF-beta, IL-10, IL- 12 and IL-1beta, and increase in the expression of IL-23 and T lymphocytes, particularly CD56+, along with decrease on cardiovascular risk demonstrated by lowered levels of cystatin C. Thus, this study provides preliminary evidence of a modulatory effect of probiotics over the immune system that may be a low-cost and practical therapeutic approach to support the immune function of HIV-infected individuals.
With a different methodological approach, Stiksrud et al. [27] showed that probiotics had no significant effect over microbial translocation, however, they found that probiotics could lower the levels of inflammation and coagulation in HIV-infected patients who had had antiretroviral therapy with viral suppression but no normalized CD4. After 8 weeks of probiotic supplementation, the levels of D-dimer and inflammatory markers including IL-6 and C-reactive protein in HIV-infected people on stable antiretroviral therapy decreased. These results are relevant because despite the persistent state of inflammation in HIV-infected individuals, their clotting systems remain more active than HIV serum negative people, becoming these individuals prone to pathological clotting.
Concerning the effects of probiotics as a neuroprotective approach for late-stage HIV infection, Ceccarelli et al. [28] investigated the effects of high-dose multiple strain probiotic supplementation on CSF immunological activation and neurocognitive performance in HIV-1-infected people taking combination antiretroviral therapy over a 6-month period. The study comprised 35 HIV serum positive people who were enrolled in the HIV clinic at the University of Rome Sapienza’s Department of Public Health and Infectious Diseases, and as a result, the intervention group presented a decrease in CNS immune activation and an improvement in cognitive performance, suggesting that probiotics could be used to treat intrathecal immune activation and cognitive impairment in HIV-infected people.
Moreover, the study also found that giving probiotics to correct dysbiosis reduces microbial translocation, systemic inflammation, and, possibly, blood-brain barrier permeability. Thus, probiotic supplementation could be a novel therapeutic option for improving the direct and indirect effects of the intestinal environment on the CNS by rebalancing the microbiota composition, and consequently the neurocognitive functions of individuals in the late stage of HIV infection. In general, the findings of the articles analyzed present consensus concerning beneficial effect on lowering inflammation and improving immunological markers in HIV serum positive individuals. The effects of probiotics on microbial translocation, on the other hand, are inconclusive, and more research is needed to enhance the state of the art of this phenomenon and how to approach it therapeutically to improve the quality of life and longevity of people living with HIV.
Conclusion
This review combines clinical evidence that supports the use of probiotics in HIV/AIDS patients due to better immune system function and decreased inflammation, which is a determinant factor in a variety of morbidities linked to HIV infection’s chronic inflammatory state. Furthermore, none of the studies included in this review reported any adverse effects from probiotics alone or in combination with antiretroviral therapy, demonstrating that probiotics are safe and antiretroviral drug interactions possibly are extremely rare events.
However, the findings on microbial translocation are unclear and may represent a major research axis for a better understanding of this phenomenon and how to address it therapeutically.
Authors and Contributors
A.L.P.C conceptualized and supervised and approved the final version, G.P.C and J.G.S. performed the literary survey, wrote the initial manuscript draft, A.C.F.S. revie
References
- Sigalov AB (2010) The School of nature IV Learning from viruses. Self Nonself 1(4): 282-298.
- Christo PP (2010) Cognitive changes in HIV infection and AIDS. Rev Assoc Med Bras 56(2):242-247.
- Pedigoni PM, Olegário EGG, Rossi CMS, Vassimon HS (2019) Effect of four-week probiotic supplementation on the immune response of HIV-infected patients. Connect Science 14(3): 66-74.
- Felipe BA, Roriz V (2020) Use of probiotics in HIV positive individuals. HU Rev 46(1): 1-7.
- Kechagia M, Basoulis D, Konstantopoulou S, Dimitriadi D, Gyftopoulou K, et al. (2013) Health benefits of probiotics: A Review. Isrn Nutr, pp. 1-7.
- Zucchetti C, Morrone FB (2012) Clinical research profile in Brazil. Clin Biomed Res 32(3): 340-347.
- Adami ER, Chemin MC, France BS, (2014) Ethical and bioethical aspects of clinical research in Brazil. Study Biol 68(2): 202-205.
- Fontanella BJB, Luchesi BM, Saidel MGB, Ricas J, Turato ER (2011) Sampling in qualitative research: Proposal of procedures to verify theoretical saturation. Cad Saude Publica 27(2): 389-394.
- Acuti MC, Flacco ME, Cappadona R, Bravi F, Mantovani L, et al. (2020) SARS-CoV-2 pandemic: An overview. Adv Biol Regul 77: 100739.
- Shang Y, Li H, Zhang R (2021) Effects of pandemic outbreak on economies: Evidence from business history context. Front Public Heal 9: 632043.
- Aragão J (2013) Introduction to quantitative studies used in scientific research. Rev Praxis 3(6): 59-62.
- Aurélio M, Oliveira P, Câmara R, Parente M (2010) Understanding randomized clinical. Bras J Video Sur Bras 4(3): 176-180.
- Zaccaron R, Ely RC, Xhafaj DC (2018) Pilot study: an important process of adaptation and refinement for quasi-experimental research in l2 acquisition. Rev do Gelne 20(1): 30-41.
- Carolina R, Ferraz S (2011) Planning as a dynamic process: the importance of the pilot study for experimental research in applied linguistics. Exchange Rev do Programa Estud Postgraduates in Linguistics Apl and Estud da Lingua 24(0): 129-146.
- Hochman B, Nahas X, Filho O, Ferreira M (2005) Research designs. Acta cirúrgica Bras 20(Supl 2): 1-9.
- Levy M, Kolodziejczyk AA, Thaiss CA, Elinav E (2017) Dysbiosis and the immune system. Nat Rev Immunol 17(4): 219-232.
- Ettorre DG, Ceccarelli G, Giustini N, Serafino S, et al. (2015) Probiotics reduce inflammation in antiretroviral treated, hiv-infected individuals: Results of the probio-HIV clinical trial. PLoS One 10(9): e0137200.
- Villar GJ, Güerri FR, Moya A, González A, Hernández JJ, et al. (2017) Impact of probiotic Saccharomyces boulardii on the gut microbiome composition in HIV-treated patients: A double-blind, randomized, placebo-controlled trial. PLoS One 12(4): e0173802.
- Storm LC, Stiksrud B, Eriksen C, Nowak P, Holm K, et al. (2019) Microbial translocation revisited. AIDS 33(4): 645-653.
- Scagnolari C, Corano SG, Selvaggi C, Schietroma I, Najafi FS, et al. (2016) Probiotics differently affect gut-associated lymphoid tissue indolamine-2,3-dioxygenase mRNA and cerebrospinal fluid neopterin levels in antiretroviral-treated HIV-1 Infected Patients: A Pilot Study. Int J Mol Sci 17(10): 1639.
- Ceccarelli G, Fratino M, Selvaggi C, Giustini N, Serafino S, et al. (2017) A pilot study on the effects of probiotic supplementation on neuropsychological performance and microRNA-29a-c levels in antiretroviral-treated HIV-1-infected patients. Brain Behav 7(8): e00756.
- Sainz T, Gosalbes MJ, Talavera A, Jimenez HN, Prieto L, et al. (2020) Effect of a nutritional intervention on the intestinal microbiota of vertically hiv-infected children: The pediabiota study. Nutrients 12(7): 2112.
- Ettorre G, Rossi G, Scagnolari C, Andreotti M, Giustini N, et al. (2017) Probiotic supplementation promotes a reduction in T-cell activation, an increase in Th17 frequencies, and a recovery of intestinal epithelium integrity and mitochondrial morphology in ART-treated HIV-1-positive patients. Immunity, Inflamm Dis 5(3): 244-260.
- Ishizaki A, Bi X, Nguyen L, Matsuda K, Pham H, et al. (2017) Effects of short-term probiotic ingestion on immune profiles and microbial translocation among hiv-1-infected Vietnamese children. Int J Mol Sci 18(10): 2185.
- Pinacchio C, Scheri GC, Statzu M, Santinelli L, Ceccarelli G, et al. (2018) Type I/II Interferon in HIV-1-infected patients: expression in gut mucosa and in peripheral blood mononuclear cells and its modification upon probiotic supplementation. J Immunol Res 1-7.
- Falasca K, Vecchiet J, Ucciferri C, Nicola M, Angelo C, et al. (2015) Effect of probiotic supplement on cytokine levels in HIV-infected individuals: A preliminary study. Nutrients 7(10): 8335-8847.
- Stiksrud B, Nowak P, Nwosu FC, Kvale D, Thalme A, et al. (2015) Reduced levels of d-dimer and changes in gut microbiota composition after probiotic intervention in hiv-infected individuals on stable ART. JAIDS J Acquir Immune Defic Syndr 70(4): 329-337.
- Ceccarelli G, Brenchley J, Cavallari E, Corano SG, Fratino M, et al. (2017) Impact of high-dose multi-strain probiotic supplementation on neurocognitive performance and central nervous system immune activation of HIV-1 Infected Individuals. Nutrients 9(11): 1269.
- Sigalov AB (2010) The School of nature IV Learning from viruses. Self Nonself 1(4): 282-298.
- Christo PP (2010) Cognitive changes in HIV infection and AIDS. Rev Assoc Med Bras 56(2):242-247.
- Pedigoni PM, Olegário EGG, Rossi CMS, Vassimon HS (2019) Effect of four-week probiotic supplementation on the immune response of HIV-infected patients. Connect Science 14(3): 66-74.
- Felipe BA, Roriz V (2020) Use of probiotics in HIV positive individuals. HU Rev 46(1): 1-7.
- Kechagia M, Basoulis D, Konstantopoulou S, Dimitriadi D, Gyftopoulou K, et al. (2013) Health benefits of probiotics: A Review. Isrn Nutr, pp. 1-7.
- Zucchetti C, Morrone FB (2012) Clinical research profile in Brazil. Clin Biomed Res 32(3): 340-347.
- Adami ER, Chemin MC, France BS, (2014) Ethical and bioethical aspects of clinical research in Brazil. Study Biol 68(2): 202-205.
- Fontanella BJB, Luchesi BM, Saidel MGB, Ricas J, Turato ER (2011) Sampling in qualitative research: Proposal of procedures to verify theoretical saturation. Cad Saude Publica 27(2): 389-394.
- Acuti MC, Flacco ME, Cappadona R, Bravi F, Mantovani L, et al. (2020) SARS-CoV-2 pandemic: An overview. Adv Biol Regul 77: 100739.
- Shang Y, Li H, Zhang R (2021) Effects of pandemic outbreak on economies: Evidence from business history context. Front Public Heal 9: 632043.
- Aragão J (2013) Introduction to quantitative studies used in scientific research. Rev Praxis 3(6): 59-62.
- Aurélio M, Oliveira P, Câmara R, Parente M (2010) Understanding randomized clinical. Bras J Video Sur Bras 4(3): 176-180.
- Zaccaron R, Ely RC, Xhafaj DC (2018) Pilot study: an important process of adaptation and refinement for quasi-experimental research in l2 acquisition. Rev do Gelne 20(1): 30-41.
- Carolina R, Ferraz S (2011) Planning as a dynamic process: the importance of the pilot study for experimental research in applied linguistics. Exchange Rev do Programa Estud Postgraduates in Linguistics Apl and Estud da Lingua 24(0): 129-146.
- Hochman B, Nahas X, Filho O, Ferreira M (2005) Research designs. Acta cirúrgica Bras 20(Supl 2): 1-9.
- Levy M, Kolodziejczyk AA, Thaiss CA, Elinav E (2017) Dysbiosis and the immune system. Nat Rev Immunol 17(4): 219-232.
- Ettorre DG, Ceccarelli G, Giustini N, Serafino S, et al. (2015) Probiotics reduce inflammation in antiretroviral treated, hiv-infected individuals: Results of the probio-HIV clinical trial. PLoS One 10(9): e0137200.
- Villar GJ, Güerri FR, Moya A, González A, Hernández JJ, et al. (2017) Impact of probiotic Saccharomyces boulardii on the gut microbiome composition in HIV-treated patients: A double-blind, randomized, placebo-controlled trial. PLoS One 12(4): e0173802.
- Storm LC, Stiksrud B, Eriksen C, Nowak P, Holm K, et al. (2019) Microbial translocation revisited. AIDS 33(4): 645-653.
- Scagnolari C, Corano SG, Selvaggi C, Schietroma I, Najafi FS, et al. (2016) Probiotics differently affect gut-associated lymphoid tissue indolamine-2,3-dioxygenase mRNA and cerebrospinal fluid neopterin levels in antiretroviral-treated HIV-1 Infected Patients: A Pilot Study. Int J Mol Sci 17(10): 1639.
- Ceccarelli G, Fratino M, Selvaggi C, Giustini N, Serafino S, et al. (2017) A pilot study on the effects of probiotic supplementation on neuropsychological performance and microRNA-29a-c levels in antiretroviral-treated HIV-1-infected patients. Brain Behav 7(8): e00756.
- Sainz T, Gosalbes MJ, Talavera A, Jimenez HN, Prieto L, et al. (2020) Effect of a nutritional intervention on the intestinal microbiota of vertically hiv-infected children: The pediabiota study. Nutrients 12(7): 2112.
- Ettorre G, Rossi G, Scagnolari C, Andreotti M, Giustini N, et al. (2017) Probiotic supplementation promotes a reduction in T-cell activation, an increase in Th17 frequencies, and a recovery of intestinal epithelium integrity and mitochondrial morphology in ART-treated HIV-1-positive patients. Immunity, Inflamm Dis 5(3): 244-260.
- Ishizaki A, Bi X, Nguyen L, Matsuda K, Pham H, et al. (2017) Effects of short-term probiotic ingestion on immune profiles and microbial translocation among hiv-1-infected Vietnamese children. Int J Mol Sci 18(10): 2185.
- Pinacchio C, Scheri GC, Statzu M, Santinelli L, Ceccarelli G, et al. (2018) Type I/II Interferon in HIV-1-infected patients: expression in gut mucosa and in peripheral blood mononuclear cells and its modification upon probiotic supplementation. J Immunol Res 1-7.
- Falasca K, Vecchiet J, Ucciferri C, Nicola M, Angelo C, et al. (2015) Effect of probiotic supplement on cytokine levels in HIV-infected individuals: A preliminary study. Nutrients 7(10): 8335-8847.
- Stiksrud B, Nowak P, Nwosu FC, Kvale D, Thalme A, et al. (2015) Reduced levels of d-dimer and changes in gut microbiota composition after probiotic intervention in hiv-infected individuals on stable ART. JAIDS J Acquir Immune Defic Syndr 70(4): 329-337.
- Ceccarelli G, Brenchley J, Cavallari E, Corano SG, Fratino M, et al. (2017) Impact of high-dose multi-strain probiotic supplementation on neurocognitive performance and central nervous system immune activation of HIV-1 Infected Individuals. Nutrients 9(11): 1269.
© 2022,Anderson Luiz Pena da Costa. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






