- Submissions

Full Text
Cohesive Journal of Microbiology & Infectious Disease
The Relationship of Hematological Disorders in SARS-CoV-2 Patients with Intensive Care Needs and Survival
Habip Gedik1*, Bilgehan Irmak1 and Osman Yokuş2
1Department of Infectious Diseases and Clinical Microbiology, İstanbul
2Department of Hematology, İstanbul
*Corresponding author: Habip Gedik, Department of Infectious Diseases and Clinical Microbiology, Istanbul
Submission: February 02, 2022; Published: March 28, 2022

ISSN 2578-0190 Volume5 issues5
Abstract
Objective: It was aimed to retrospectively examine the clinical and survival results of patients who were
consulted with the hematology clinic due to hematological disorders related to severe acute respiratory
syndrome coronavirus-2 (SARS-CoV-2).
Materials and methods: In this study, the data of patients who were hospitalized and consulted to the
hematology clinic due to hematological disorders related to COVID-19 infection diagnosed by radiological
findings and/or PCR results in the Ministry of Health Istanbul Training and Research Hospital between
April 1 2020 and May 21 2020, were evaluated, retrospectively.
Results: Of the 48 patients evaluated in the study, 25 (52%) were female and 29 (60%) were 60 years old
and above. Leukocytosis in 5(10%) patients, leukopenia in 19 (39%) patients, and D-Dimer ≥2ng/mL
and Ferritin ≥500ml/ng in 32(66%) patients were remarkable. D-Dimer was found to be ≥2ng/mL and
Ferritin ≥500ml/ng in 9 out of 10 patients in intensive care. A total of seven (14%) patients died.
Conclusion: Patients who are over the age of 60, and have lymphocyte count <1000μl/ml, D-Dimer value
above 2ng/mL, and ferritin over 500ml/ng are more likely to need a follow-up in the intensive care. For
this reason, vaccination of people over the age of 60, moreover, the high antibody response obtained with
the vaccine seems to be the most important precaution that can be taken against this disease.
Keywords:COVID-19; SARS-CoV-2; Gender; Hematology; Lymphopenia; Thrombocytopenia; Survival; Intensive care; D-dimer; Ferritin
Introduction
Coronavirus Disease (COVID-19) is the clinical syndrome associated with SARS-CoV-2 infection and characterized with an extent from a mild upper respiratory tract disease to severe interstitial pneumonia or an Acute-Respiratory-Distress-Syndrome (ARDS) [1]. Symptoms of COVID-19 infection can be asymptomatic depending on the immune response of the host and comorbid diseases, as well as mild, moderate, severe, or critical status of patients [2]. In the early stage of infection, mild symptoms, dry cough, diarrhea, headache, etc. may be encountered with other complaints. During this period, there is an increase in lymphopenia, increased prothrombin time, D-dimer, and Lactate Dehydrogenase (LDH) values. In the second phase, shortness of breath, hypoxia, PaO2/FiO2≤300mmHg, abnormalities in lung imaging, increased transaminases, low/normal procalcitonin levels are seen. In the third phase, the inflammatory response of the host gradually increases. ARDS, Systemic Inflammatory Response Syndrome (SIRS), shock, heart failure, and multi-organ dysfunction may be encountered. Inflammatory markers (c-reactive protein (CRP), LDH, IL-6, D-dimer, ferritin, etc.) increase during this period. Troponin and pro-BNP heights can be seen as well. Chen et al. [3] reported that the increase in the neutrophil ratio, C-reactive protein, and procalcitonin values is related to cytokine storm induced by virus invasion or accompanied by other infections in severe Covid-19 cases [3]. Gao et al. [4] revealed that the D dimer values were significantly higher in severe patients compared to mild and moderate patients [4]. In the study of Zhou et al. [5] D-dimer values were found to be approximately nine times higher in patients who died. A D-dimer value greater than 1μg/ml may help to identify patients with a poor prognosis at the early stage [5]. Studies have found that a low lymphocyte count, high D-dimer, and acute phase reactants (CRP, ferritin) levels are associated with a more severe outcome of the disease [6-8]. Therefore, it was aimed to conduct the study to retrospectively examine the clinical and survival results of patients who were consulted with the hematology clinic due to hematological disorders related to SARS-CoV-2.
Materials and Methods
In this study, the data of patients who were hospitalized and consulted to the hematology clinic due to hematological disorders related to COVID-19 infection diagnosed by radiological findings and/or PCR results in the Ministry of Health Istanbul Training and Research Hospital between April 1 2020 and May21 2020, were evaluated in terms of the relationship between hematological disorders and the need for intensive care and survival, retrospectively. The gender, age, leukocyte, lymphocyte count, eosinophil count, thrombocyte count, D-Dimer and ferritin levels, intensive care status, and survival status of the patients were recorded. In order to statistically evaluate the hematological values of the patients, reference values were categorically 3,500- 11,000μl/ml for the definition of normal leukocyte value, >1,000μl/ ml for the lympphocyte value, >40μl/ml for the normal eosinophil value, 100,000μl for the normal platelet value. Under 60 years old and above for age, female and male for gender, between 3,500 and 11,000μl/ml for the normal range of leukocyte counts, >1000μl/ ml, between 500 and 1000μl /ml, and <500μl/ml for the normal lymphocyte counts, >40μl/ml and <40μl/ml for the eosinophil counts, <100,000μl/ml and >100,000μl/ml for the thrombocyte counts, >2ng/mL and <2ng/mL for the D-dimer values, >500mL/ ng and <500mL/ng for the ferritin values were categorized for the better statistical evaluation of valuables and values that were width in the normal ranges [2,3]. While only the patients who were consulted with the hematology clinic due to disorders in their hematological parameters were included in the study, those who had incomplete data were excluded from the study. This study was approved by the Ministry of Health authorized board on 06.12.2020. Nominal data of the patients were categorized and classified as normal, low, and high. Numerical data were presented up to decimal percent. The data were categorized taking into account the width in the normal range of blood cell numbers and laboratory tests. With the categorized data, it was aimed to reveal the clustering of the patients more clearly. For the statistical evaluation of the study, Chi-square or Fischer’s exact tests were used to compare nominal data, Pearson correlation coefficient and Odd’s ratio were used to evaluate the levels of the relationship between them, while the confidence interval was taken as 95%.
Result
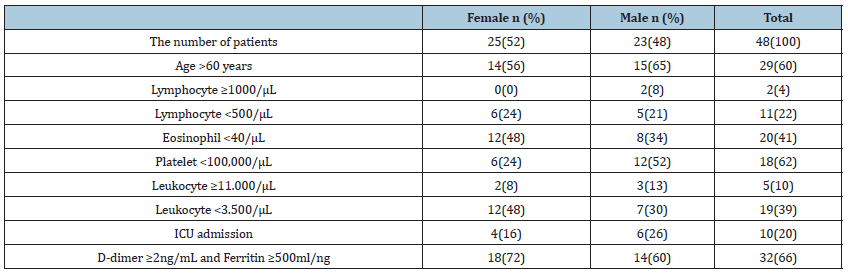
Of the 48 patients evaluated in the study, 25(52%) were female, 23(48%) were male, and 29(60%) were 60 years old and above. Leukocytosis in 5(10%) patients, leukopenia in 19(39%) patients, D-Dimer ≥2ng/mL and Ferritin ≥500ml/ng in 32(66%) patients were remarkable. D-Dimer was found to be ≥2ng/mL and Ferritin ≥500ml/ng in 9 out of 10 patients in intensive care. A total of seven (14%) patients were deceased. Of the 7 mortal patients, 4 (57%) were female, followed by thrombocytopenia in 5(71%), eosinophilopenia (<40/μL) in 20(41), lymphocyte count <1,000μl/ ml in 5(71%) and <500μl/ml in 2 (28%), leukopenia (<3.500/μL) in 3(42%), normal leukocyte count in 4 (57%), and 5 (71%) over 60 years old. Of the 16 patients with D-dimer value >2ng/mL and ferritin >500ml/ng, 13 (81%) were over 60 years old, 9(56%) were male, 9(56%) were under intensive care follow-up. As lymphocyte count was <1,000μl/ml in 11 (68%) patients, 7 (43%) died. The parameters of 48 patients evaluated by the hematology clinic are given in Table 1. In the statistical analysis of the study, no significant relationship was found between survival and gender (Fischer’s exact test p: 0,771). In terms of survival, no significant difference was found between patients under 60 years of age and above (Fischer’s exact test p: 0.687). There was no significant difference in terms of survival in terms of leukocyte count, lymphocyte count, eosinophil count, platelet count (Chi-Square test p: 0.813, p: 0.438, p: 0.429, p: 0.086, respectively). A significant difference was found in terms of survival and need for intensive care (Fischer’s exact test p: 0.0001; Pearson correlation coefficient: -0.805; Odd’s ratio: 13.66; Confidence Interval 4.59-40.62). A significant correlation was found between low survival rates and high D-Dimer and Ferritin values (Fischer exact test p: 0.0001; Pearson correlation coefficient: -0.584; Odd’s ratio: 4.55; Confidence Interval: 2.55-8, 11th). A significant correlation was found between the increased need for ICU and high D-Dimer and Ferritin values (Fischer exact test p: 0.0001; Pearson correlation coefficient: 0.617; Odd’s ratio: 39.85; Confidence Interval: 4.35-368).
Table 1:The hematological parameters of patients with COVID-19 by gender.
Discussion
In our study, the female-male ratio was almost similar and more than half of them were over the age of 60. The female-male ratio was similar in the conducted studies as well [9,10]. On the other hand, the number of male cases among critical patients with COVID-19 was higher according to the data reported from China, and 82% of the patients requiring critical care were male in the ICU in Italy [8,11,12]. Leukopenia, lymphopenia, platelet (100,000μl/ ml) and D-dimer >2ng/mL and ferritin> 500ml/ng were mainly remarkable values in our cases. In a study conducted by Cömert et al. [13] the common laboratory findings at the time of diagnosis were low albumin (75%), high CRP, lymphopenia (43%), and high D-dimer, ferritin, and liver enzymes. High CRP, D-dimer, serum ferritin, prolonged prothrombin time, troponin elevation, creatinine phosphokinase elevation, and hypoxemia have been identified as poor prognostic factors as well [12,13]. In other studies, about COVID-19, neutrophil count, D-Dimer, blood urea, and creatinine levels increased, and lymphocyte count continued to decrease until death [5,12,14]. Leukocytosis, lymphopenia, thrombocytopenia, hypoalbuminemia, creatinine, D-dimer, and ferritin levels were also found to be more prominent in severe disease in a study when compared with patients without severe disease and laboratory findings [15]. In the severe cases neutrophil ratio, CRP, and procalcitonin were found high, as lymphocyte ratio and number were found to be low. In addition, leukocyte and neutrophil counts increased numerically in severe cases, but the difference was not found to be significant, statistically [16]. In a study conducted in China, there was no difference in leukocyte count between severe cases and non-severe cases [17]. It was reported that 109 Covid-19 patients who died in Wuhan city were admitted with higher leukocyte counts than 116 patients who recovered. The patients in the death group had a lower lymphocyte count and the lymphocyte/ leukocyte ratio continued to decrease, significantly [18]. In the study of Yuan et al. [19] leukocyte and neutrophil values were significantly higher in the severe and critical patients with COVID-19 compared to the normal group. Erythrocyte and hemoglobin values have been reported to decrease in critical conditions, as the platelet count was often found to be normal. While ferritin and D-dimer values were more pronounced in critically ill patients, the blood was hypercoagulable and critical levels of D-dimer and fibrinogen were higher in those cases than in normal patients [19,20]. Another study reported that 71.4% of non-survivors and 0.6% of survivors met the criteria for the disseminated intravascular coagulation during their hospital follow-up and significantly elevated D-dimer and FDP were cases who died of COVID-19 (20). Moreover, 71.4% of mortal cases and 0.6% of survivors had the diffuse intravascular coagulation (DIC) criteria and abnormal coagulation, especially with more markedly elevated D-dimer and fibrin washed-out [21]. In a meta-analysis conducted by Huang et al. [22] 11 of 25 studies revealed high D-dimer values related to the poor result. Subgroup analysis found that a higher D dimer values are associated with increased mortality rates. A higher serum ferritin level was found to be independently associated with ARDS, mortality, and severe COVID-19, as well as other biomarkers included in this study. Non-survival had higher levels of ferritin as a result of SARS-CoV-2 infection that can trigger hemostatic dysfunction and result in mortality in cases with a severe COVID-19 course. That supports the hypothesis about hypercoagulation [22]. In conclusion, patients who are over the age of 60, and have lymphocyte count <1000μl/ ml, D-dimer value >2ng/mL, and ferritin >500ml/ng are most likely to need an intensive care, moreover;... moreover, patients who have thrombocytopenia, lymphopenia, D-dimer >2ng/mL and ferritin >500ml/ng are more likely to result in mortality. Therefore, the vaccination of people over the age of 60, moreover, the high antibody response to be obtained with the vaccine seems to be the most important measure that can be taken against this disease.
References
- Petrosillo N, Viceconte G, Ergonul O, Ippolito G, Petersen E (2020) COVID-19, SARS, and MERS: are they closely related? Clin Microbiol Infect 26(6): 729-734.
- Shang Y, Pan C, Yang X (2020) Management of critically ill patients with COVID-19 in ICU: a statement from front-line intensive care experts in Wuhan, China. Ann Intensive Care 10(1): 73.
- Chen N, Zhou M, Dong X (2020) Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. The Lancet 395(10223): 507-513.
- Gao Y, Li T, Han M (2020) Diagnostic utility of clinical laboratory data determinations for patients with the severe COVID-19. J Med Virol 92(7): 791-796.
- Zhou F, Yu T, Du R (2020) Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 395(10229): 1054-1062.
- Wu Z, McGoogan JM (323) Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese center for disease control and prevention. JAMA 323(13): 1239-1242.
- Shang Y, Pan C, Yang X (2020) Management of critically ill patients with COVID-19 in ICU: a statement from front-line intensive care experts in Wuhan, China. Ann Intensive Care 10(1): 73.
- Wang D, Hu B, Hu C (2020) Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 323(11): 1061-1069.
- Arentz M, Yim E, Klaff L (2020) Characteristics and outcomes of 21 critically Ill patients with COVID-19 in Washington State. JAMA 323(16): 1612-1614.
- Zhang JJ, Dong X, Cao YY (2020) Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy 75(7): 1730-1740.
- Grasselli G, Zangrillo A, Zanella A (2020) COVID-19 Lombardy ICU network baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy. JAMA 323(16): 1574-1581.
- Guan WJ, Ni ZY, Hu Y (2020) China medical treatment expert group for Covid-19 clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 382(18): 1708-1720.
- Cömert (2020) COVID-19 Olgusunun klinik ozellikleri ve yaklaşı Southern Clinics of Istanbul Eurasia 31: 13-15.
- Çelik D, Kose Ş (2020) COVID-19 in adults: clinical findings. The Journal of Tepecik Education and Research Hospital 30(2): 43-48.
- Karakoç ZÇ, Pınarbaşı ŞB, Asil R, Dodurgali R, Çalışkaner F, et al. (2020) COVID-19 pandemisinde birinci dalga deneyimi: tek merkez deneyimi. Klimik Dergisi 33(3): 223-229.
- Li K, Wu J, Wu F (2020) The clinical and chest CT features associated with severe and critical covid-19 pneumonia. Invest Radiol 55(6): 327-331.
- Zhou Y, Zhang Z, Tian J (2020) Risk factors associated with disease progression in a cohort of patients infected with the 2019 novel coronavirus. Ann Palliat Med 9(2): 428-436.
- Deng Y, Liu W, Liu K (2020) Clinical characteristics of fatal and recovered cases of coronavirus disease 2019 (COVID-19) in Wuhan, China: a retrospective study. Chin Med J(Engl) 133(11): 1261-1267.
- Yuan X, Huang W, Ye B (2020) Changes of hematological and immunological parameters in COVID-19 patients. Int J Hematol 112(4): 553-559.
- Sümer Ş, Ural O, Aktuğ Demir N (2020) Clinical and laboratory characteristics of COVID-19 cases followed in Selçuk University Faculty of Medicine. Klimik Derg 33(2): 122-127.
- Tang N, Li D, Wang X, Sun Z (2020) Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost 18(4): 844-847.
- Huang I, Pranata R, Lim MA (2020) C-reactive protein, procalcitonin, D-dimer, and ferritin in severe coronavirus disease-2019: a meta-analysis. Ther Adv Respir Dis 14: 1753466620937175.
© 2022, Habip Gedik. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






