- Submissions

Full Text
Cohesive Journal of Microbiology & Infectious Disease
A Rare Case of Wunderlich Syndrome Secondary to Bleeding Renal Angiomyolipoma (AML)
Mohamed Shafi MA*, Wan Zainira WZ, Mohamad Nizam H, Rosnelifaizur Ramely, Wan Mokhzani and Syed Hassan
Physician, Epidemiologist, Colombia
*Corresponding author: Physician, Epidemiologist, Colombia
Submission: September 03, 2021; Published: October 13, 2021

ISSN 2578-0190 Volume5 issues4
Abstract
Wunderlich syndrome is a rare fatal condition characterized by spontaneous atraumatic renal hemorrhage that confined to peri-renal and sub capsular space. It may present as an acute or insidious onset. Female has more predilection for the syndrome compared to males. Diagnosis is usually incidental. A constellation of symptoms known as Lenk’s triad described by the German physician Carl Reinhold August Wunderlich in diagnosing the condition that are acute flank pain, flank mass and hypovolemic shock. Etiologies related to the syndrome can be broadly classified into neoplastic and non-neoplastic. Commonest benign neoplastic cause of Wunderlich syndrome is renal angiomyolipoma while malignant causes such as Renal Cell Carcinoma (RCC) and liposarcoma. Non neoplastic causes such as vasculitis, aneurysm, arteriovenous malformation and cystic rupture. Wunderlich syndrome has a high mortality rate associated with the rupture of the hematoma. Early accurate diagnosis is crucial in patient’s intervention and management. Multimodality treatment is available in Wunderlich syndrome such as highly specific embolization, surgeries as well as conservative. Treatments are tailored according to the hematoma size, availability specialty services and patient’s hemodynamic status.
Keywords:Wunderlich syndrome; Angiomyolipoma; Hematoma
Introduction
Angiomyolipoma are mostly asymptomatic and are diagnosed incidentally through imaging usually from an unrelated clinical presentation. The bleeding risk is directly proportional to its size. Angiomyolipoma that are less than 4cm has a bleeding risk of about 13% compared to those that are more than 4cm which is about 51% [1]. Although clinical presentations may vary, most patients present with acute flank pain, flank mass, hematuria and hemodynamic instability [2]. Lenk’s triad is used in clinical diagnosis of Wunderlich syndrome: acute flank pain, flank mass and hypovolemic shock. In this case report we would like to highlight about a young patient with a giant renal angiomyolipoma that manifested as Wunderlich syndrome.
Case Report
A 35-years-old man presented to the Emergency Department (ED) with the complaint of one day history of severe right flank pain associated with nausea and vomiting. The pain radiated to the right iliac fossa region with the pain score of 10/10.Intravenous morphine was given in order to control the pain. His vital signs were abnormal with the systolic blood pressure ranging 80-90mmhg and heart rate of 110-120 beats per-minute. Biochemically the white cell count was raised 13.54x109, hemoglobin is 10.4g/dl while the coagulation and renal profile were within normal range. Clinically the abdomen was guarded with cardboard rigidity and no mass were palpable. Initial fluid resuscitation was commenced by the ED team and upon surgical review we had the initial diagnosis of ruptured appendicitis with septic shock and posted the case for an emergency laparoscopic appendicectomy. No prior ultrasound was performed as the patient demonstrated clear-cut features of a ruptured appendicitis and ordering an ultrasound will further delay the management of the patient. Upon breaching the peritoneum, they were hemorrhagic fluids surrounding the bowels and pelvic cavity with a normal looking appendix. Upon mobilizing the small bowel and ascending colon we noticed a large, contained hematoma arising from zone 2 with an intact Gerota’s fascia. We decided to perform laparoscopic appendicectomy with peritoneal lavage and left alone the contained hematoma. Pre-emptive appendicectomy was done as to avoid future risk of appendicitis and in the hope of finding other pathology in the appendix during histology review. An urgent contrasted Computed Tomography (CT) of the patient obtained on the very same day. Packed red blood cells were also transfused to maintain a normal range of hemoglobin and blood pressure. Otherwise, patient was nurse in the Surgical High Dependency Unit (SHDU) (Figures 1-4).
Figure 1:Axial cut of the CT scan showing (white arrow) a large right sided well defined exophytic heterogeneous mass measuring (9.7x11.7x10.0) cm. Presence of intralesional fat, soft tissue and abnormal vascular component with no internal calcification seen.
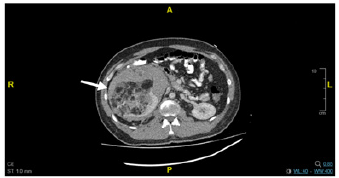
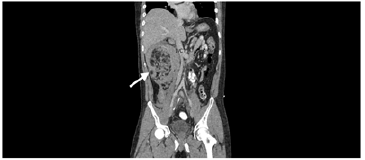
Figure 2: Coronal cut of the CT scan showing the exophytic mass arising from the lower pole the right kidney and compressing the inferior vena cava.
CT scan reported the mass as a right renal angiomyolipoma complicated with hemorrhage. In view of the evidence of ongoing bleed from the angiomyolipoma, we decided to get the assistance of the interventional radiologist. Patient was then subjected for a highly selective embolization the next day. The right renal artery was cannulated with 5F catheter and embolization was performed using gel foam into the arterial feeders via inferior polar artery. No complications encountered during and after the procedure. Patient was discharged home well after few days in the general ward. We then repeated the CT scan after 1 month to look for any changes of the Agiomyolipoma (AML) post embolization. Repeated scan showed a significant reduction of the angiomyolipoma (AML) size with relieved compression of the Inferior Vena Cava (IVC). He was also referred to the urology department for further work-up and investigation as Renal Cell Carcinoma (RCC) was one of our differential diagnosis.
Figure 3: Angiogram of the right renal vessel showing (black arrow) contrast flow with no extravasation to the surrounding structures post embolization.
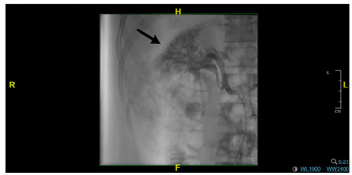
Figure 4: Coronal view of the CT scan showing angiomyolipoma (white arrow) pre and post embolization with reduced compression effect on the Inferior Vena Cava (IVC).

Discussion
Wunderlich syndrome (WS) is a surgical emergency and could be fatal if not detected early. Classical presentations of WS are acute flank pain, flank mass and hypovolemic shock which is collectively known as the Lenk’s triad [3]. Renal Angiomyolipoma (AML) is the commonest cause of WS [4]. Renal Angiomyolipoma (AML) is a solid benign renal lesion and consist of poorly organized blood vessels, smooth muscle and varying levels of mature adipose tissue. Diagnosis of AML is usually incidental through imaging or from some unrelated clinical presentations. Early detection of AML may avoid patients from undergoing unnecessary high-risk surgeries. As in this case, we managed to detect Wunderlich Syndrome (WS) early and subjected the patient for highly selective embolization which saved his life and reduced the morbidity. Although patient did not present with the classical Lenk’s triad, he developed hypovolemic shock due to the expansion of Angiomyolipoma (AML) which compressed the Inferior Vena Cava (IVC) and thus reducing the venous return to the heart. Risk of bleeding in angiomyolipoma is classified according to its size. Less than 4cm lesion having 13%risk of bleeding compared to lesion that is larger than 4cm which is 50% [5]. Various imaging modalities may be used in diagnosing AML and by far CT scan is the best. CT scan may differentiate AML with other lesions, such as tuberous sclerosis and renal cell carcinoma by the presence of fat and absence of internal calcification. MRI is excellent in evaluating fat containing lesion as well as fat-poor AML. Digital Subtracting Angiography (DSA) may be use for the AML diagnosis with certain specific characteristic such as ‘sunburst appearance’ of the tortuous vessels, whorled peripheral vessel with ‘onion peel’ appearance, micro and macro aneurysm as well as absent of arteriovenous shunting. Management of AML is based on the size of the lesion and patient’s symptoms. Oesterling et al. [5] proposes that lesion that is less than 4cm diameter may be treated conservatively with yearly CT while those that are more than 4cm may be done CT every 6 monthly to assess the growth. Symptomatic AML patient with evidence of lesion growth should be considered for prophylactic embolization as it is the most successful nephron sparing procedure. Nephrectomy is preserved for hemodynamically unstable patients and in case of failed embolization.
Conclusion
Diagnosing Wunderlich Syndrome (WS) is very challenging especially when patient presented with a vague clinical feature. Early detection of AML causing Wunderlich Syndrome is crucial as therapeutic embolization is proven to lower the mortality and morbidity of the patient. Clinicians should be vigilant and have a high index of suspicion when a retroperitoreal hematoma is detected as Wunderlich Syndrome (WS) may be fatal if treatment is delayed.
References
- Simmons JL, Hussain SA, Riley P, Wallace DM (2003) Management of renal angiomyolipoma in patients with tuberous sclerosis complex. Oncol Rep 10(1): 237-241.
- Seyam RM, Bissada NK, Kattan SA (2008) Changing trends in presentation, diagnosis and management of renal angiomyolipoma: Comparison of sporadic and tuberous sclerosis complex associated forms. Urology 72(5): 1077-1082.
- Phillips, Lepor H (2006) Spontaneous retroperitoneal hemorrhage caused by segmental arterial mediolysis. Rev Urol 8(1): 36-40.
- Molina ER, Castillo OA (2013) Spontaneous retroperitoneal haemorrhage of renal origin (Wunderlich Syndrome): Analysis of 8 cases. Arch Esp Urol 66(10): 925-929.
- Oesterling JE, Fishman EK, Goldman SM, Marshall FF (1986) The management of renal angiomyolipoma. J Urol 135(6): 1121-1124.
© 2021,Mohamed Shafi MA. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






