- Submissions

Full Text
Cohesive Journal of Microbiology & Infectious Disease
Wrist Circumference in Relation to the Risk of Metabolic Syndrome in Middle-Aged and Elderly Chinese Patients with Type 2 Diabetes
Jingyang Gao1,2, Yan Li3, Ziwei Lin1,2, Meili Cai1,2, Cuiling Zhu1,2, Xingchun Wang1,2, Hong Li1,2, Chunjun Sheng1,2, Xiaoyun Cheng1,2, Peng Yang1,2 and Manna Zhang1,2*
1Department of Endocrinology and Metabolism, Tongji University School of Medicine, China
2National Metabolic Management Center, China
3Department of Endocrinology, Shanghai Children’s Hospital, China
*Corresponding author: Manna Zhang, Department of Endocrinology & Metabolism, Tongji University School of Medicine, China
Submission: March 29, 2021; Published: April 15, 2021

ISSN 2578-0190 Volume5 issues1
Abstract
Objective: In this study, we aimed to determine whether wrist circumference is associated with increased with of metabolic syndrome (MetS) among middle-aged and elderly Chinese type 2 diabetes (T2DM) subjects.
Method: A total of 470 type 2 diabetes hospitalized patients were included in the study. Data on demographic characteristics, anthropometry and variables were collected. Serum lipid profile, HbA1c, and beta-cell function were detected in blood samples. The diagnosis of MetS was ascertained by the International Diabetes Federation (IDF) criteria. Results: The mean of wrist circumference in male and female patients were 15.5 and 17.0cm, respectively. Weight, body mass index, waist circumference, triglycerides and incident MetS gradually increased with the increment of wrist circumferenc etertiles and HDL gradually decreased with the increment of wrist circumference tertiles (all P<0.05) even after adjustment of onset age of diabetes and duration of T2DM in both gender. When adjusted for body mass index, and waist circumference, the association between wrist circumference and MetS remained significant only among the normal group women (BMI<25kg/m2).
Conclusion: These results suggested that a higher wrist circumference was associated with higher risk for MetS in T2DM subjects, especially in the female T2DM with BMI<25kg/m2.
Keywords: Wrist circumference; Type 2 diabetes; Metabolic syndrome
Introduction
The metabolic syndrome is the clustering of abdominal obesity, hypertension, hyperglycemia, elevated triglycerides, and/or decreased high-density lipoprotein cholesterol (HDL) levels [1]. The prevalence of metabolic syndrome has grown markedly worldwide during the past decades. The syndrome not only contributes to the risk of cardiovascular diseases and type 2 diabetes, but also cardiovascular morbidity and mortality [2-4]. The core manifestation of metabolic syndrome is insulin resistance, which is associated with each individual metabolic syndrome components [5,6]. Wrist circumference, an easy to measure anthropometric index of body frame and bone size, has recently been suggested to be associated with insulin resistance in both children and adults [7,8]. Furthermore, wrist circumference proved to be a significant predictor of diabetes in both genders of adult population, but its predictability was independent of body mass index or waist circumference only in females [9]. A result of a decade follow-up in a West Asian cohort showed that wrist circumference as a novel predictor of hypertension and cardiovascular disease [10], while it was in contrast with a media follow-up of nine years study showing a higher wrist circumference was a negative predictor for incident cardiovascular disease among adult men [11]. However, limited data was available on the association between wrist circumference and metabolic syndrome. Only one study stated that wrist circumference was significant association with incident metabolic syndrome (as pre-diabetes state) in both males and females [9]. Our objective is to assess the association between wrist circumference and metabolic syndrome among middle-aged and elderly type 2 diabetes patients requiring admission to a large urban hospital in China.
Method
Patients
A total of 193 female and 277 male patients with type 2 diabetes who were admitted to the Shanghai Tenth People’s Hospital between January 2014 and December 2015 were recruited in our study. Exclusion criteria included 1) clinical symptoms with generalized edema; 2) hyperthyroidism; 3) hypothyroidism; 4) the presence or history of cancer; 5) moderate or severe liver and renal dysfunction. The diagnosed of type 2 diabetes was based on the American Diabetes Association definition. Metabolic syndrome was defined according to the International Diabetes Federation (IDF) definition (1). According to the IDF definition, a person was defined as having metabolic syndrome if he or she had central obesity (defined as waist circumference ≥90cm for men and ≥80cm for women) plus any two of the following four factors: 1) Raised triglyceride level: ≥150mg/dL (1.7mmol/L), or specific treatment for this lipid abnormality, 2) Reduced high-density lipoprotein cholesterol: <40mg/dL (1.03mmol/L) in males and<50 mg/dL (1.29mmol/L) in females, or specific treatment for this lipid abnormality, 3) Raised blood pressure: systolic blood pressure ≥130 or diastolic blood pressure≥85mm Hg, or treatment of previously diagnosed hypertension, 4) Raised fasting plasma glucose≥100mg/dL (5.6mmol/L), or previously diagnosed type 2 diabetes. The study protocol was approved by the Institutional Human Subjects Review Board of Shanghai Tenth People’s Hospital, and all participants gave their informed consent.
Measurements
Age, age of onset, and duration of diabetes, family history, blood pressure, height, body weight and body mass index (BMI) were obtained. Wrist circumference was measured to the nearest 0.1cm using a tape measure. Subjects were asked to hold their wrist anterior surface up; the superior border of the tape measure was placed just distal to the prominences of radial and ulnar bones. Waist Circumference was measured against the skin at the natural waist (midpoint between the top of the iliac crest and the lower ribs) with a non-elastic flexible tape measure. After 12 hours of overnight fasting, laboratory test parameters were collected in the morning during the patients’ admission, including Total Cholesterol (TC), Triglyceride (TG), High-Density Lipoprotein (HDL), Low-Density Lipoprotein (LDL), Free Fatty Acid (FFA), Uric Acid (UA), glycosylated hemoglobin A1c (HbA1c), fasting plasma glucose, and fasting C-peptide. The standard meal-load test (70g of instant noodles equivalent to an energy intake of 500 kilocalories) was performed [12], followed in 120 minutes by examination of plasma glucose, insulin, and C-peptide. AUC (Area Under the Curve) was calculated with the following equations (AUC for glucose, for example): AUC for glucose= (glucose 0min + glucose30min)×30/2+(glucose 30min+glucose120min) × 90/2+(glucose120 min + glucose180min) × 60/2 [13]; glucose 0 min denotes the glucose concentration tested just before the patient started the standard meal, and glucose 30 min the concentration tested 30 min after starting the meal, and so on.
Statistical Analysis
Data were expressed as mean ± standard deviation (SD) for normal distribution and expressed as median (upper and lower quartiles) for skewed distribution. Standard T test was used to compare the baseline morphometric measurements. Data of skewed deviations were compared by nonparametric test. Pearson’s correlation analysis was used to investigate the relationship of two indices. Binary logistic analysis was performed to analyze the association between variables and incident MetS. Statistical Product and Service Solutions version 20 (SPSS 20) software were used for statistical analysis. A value of P<0.05 was considered statistically significant.
Result
General characteristics of patients with T2DM
Clinical characteristics of the patients (193 females and 277 males) are summarized in Table 1. Mean age of the baseline population was 63.4±12.9 years for females and 58.9±12.8 years for males; and the mean wrist circumference was 15.6±1.2 cm in females and 16.9±0.9 cm in males. Duration of diabetes in female group was longer than that of male group. Onset age of diabetes, family history of diabetes, BMI, hip circumference, TG, FFA, HbA1c, fasting glucose and postprandial glucose were not different between the female and male groups. Blood pressure, AUC for glucose, AUC for c-peptide, TC, LDL in female group were higher than that of male group, whereas uric acid and HDL in female group were lower than in male group. The prevalence of MetS was much higher in female that in male group.
Table 1: Baseline Characteristics of the Study Population.

Data are presented as mean ± SD or median (inter quartile range). P<0.05 (female vs male).
BMI: Body Mass Index; SBP: Systolic Blood Pressure; DBP: Diastolic Blood Pressure; HbA1c: Glycosylated Hemoglobin A1c; AUC: Area Under the Curve; TC: Total Cholesterol; TG: Triglyceride; HDL: High-Density Lipoprotein; LDL: Low- Density Lipoprotein; FFA: Free Fatty Acid; UA: Uric Acid; MetS: Metabolic Syndrome
Univariate correlations between wrist circumference and component of MetS
The results of all correlation analyses are reported in Table 2. Univariate correlations analysis in the entire cohort showed that wrist circumference was positively associated with weight, BMI, WC, SBP, TG, MetS, and negatively associated with HDL, AUC-glucose. In female, wrist circumference was correlated with weight, BMI, WC, TG, HDL, DBP, AUC for glucose and MetS. In male, wrist circumference was correlated with weight, BMI, WC, TG, HDL, and MetS. There was no significant association between wrist circumference and DBP among three groups. All data were adjusted for age, onset age of diabetes and duration of T2DM.
Table 2: Univariate correlations between wrist circumference and component of MetS.
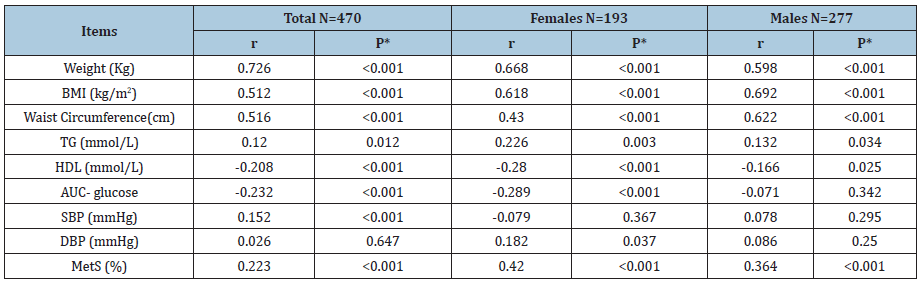
*All data were adjusted for age, onset age of diabetes and duration of T2DM.
BMI: Body Mass Index; SBP: Systolic Blood Pressure; DBP: Diastolic Blood Pressure; AUC: Area Under the Curve; TG: Triglyceride; HDL: High-Density Lipoprotein; MetS: Metabolic Syndrome
Association of wrist circumference tertiles with MetS
The patients were divided into three groups according to the cut-off points of the wrist circumference tertiles. From the lowest tertiles to the highest tertiles, the range of wrist circumference was<15.0, 15.0–15.9, and >15.9 cm for females; <16.6, 16.6–17.3, and >17.3 cm for male. Weight, BMI, WC, TG and incident MetS gradually increased with the increment of wrist circumference tertiles and HDL gradually decreased with the increment of wrist circumference tertiles (all P<0.05) even after adjustment of onset age of diabetes and duration of T2DM in both genders. Overall, as well as in both the genders, there was no significant association between wrist circumference and DBP (Table 3). In multivariable model, a significant association was shown between the increase of wrist circumference tertiles and MetS. Furthermore, compared with the participants in the first wrist circumference, those in the other two tertiles had successively a 7.61- and 22.71-fold risk of MetS in females and a 2.18- and 9.60-fold in males after adjustment for various risk factors (Table 4). In the normal women group (BMI<25kg/m2), after adjusting for variable various characteristics plus BMI and waist circumference, increase in wrist circumference was independently associated with MetS (OR8.45 (1.12-43.61)). However, wrist circumference increase could not predict MetS among the overweight/obese women (BMI≥25 kg/m2), the normal male or the overweight/obese male groups (Table 5).
Table 3: Component of MetS in patients according to wrist circumference tertiles.
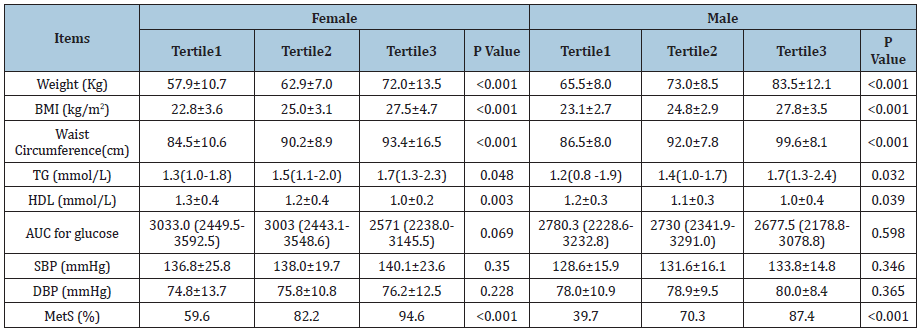
*All data were adjusted for age, onset age of diabetes and duration of T2DM.
BMI: Body Mass Index; SBP: Systolic Blood Pressure; DBP: Diastolic Blood Pressure; AUC: Area Under the Curve; TG: Triglyceride; HDL: High-Density Lipoprotein; MetS: Metabolic Syndrome
Table 4: Association of wrist circumference tertiles with metabolic syndrome.
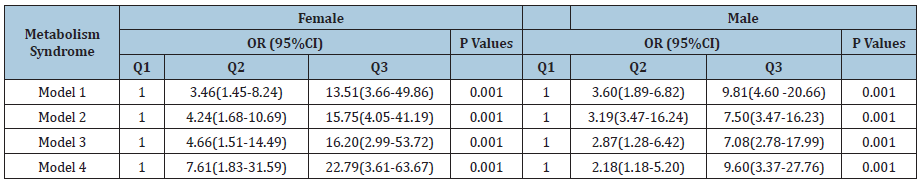
Analyzed by binary logistic regression analysis; CI: Confidence Interval; OR: Odds Ratio; Model 1, adjusted for age. Model 2, adjusted for age, duration of diabetes and family history of diabetes. Model 3, adjusted for age, duration of diabetes, family history of diabetes, glycated hemoglobin, fasting C-peptide, Postprandial C-peptide. Model 4, adjusted for adjusted for age, duration of diabetes, family history of diabetes, glycated hemoglobin, fasting C-peptide, Postprandial C-peptide, total cholesterol, LDL: Low-Density Lipoprotein, free fatty acid, uric acid
Table 5: Odds Ratios of developing metabolic syndrome for 1 cm increase in wrist circumference beyond other fat distribution.
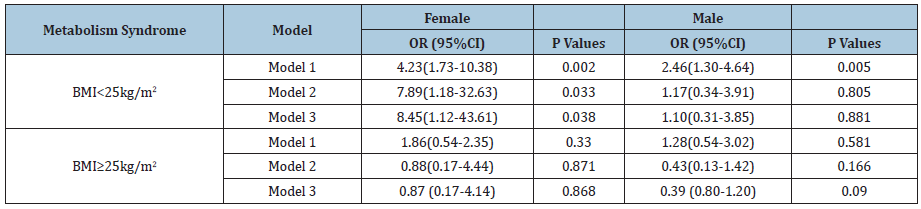
Analyzed using binary logistic regression analysis; OR: odds ratio; CI: confidence interval; Model 1, adjusted for adjusted for age, duration of diabetes, family history of diabetes, glycated hemoglobin, fasting C-peptide, total cholesterol, LDL: Low-Density Lipoprotein; free fatty acid, uric acid; Model 2, Model1+Waist circumference; Model 3, Model 2+BMI
Discussion
The wrist circumference parameter is easily accessible and measurable by the doctor, which has been recently demonstrated that it was associated with insulin resistance, diabetes, cardiovascular risk [7-10]. However, limited data was available on the association between wrist circumference and metabolic syndrome. The present study provided the first evidence that wrist circumference was significantly associated with MetS in the middle-aged and elderly T2DM requiring admission requiring admission to a large urban hospital in China. Wrist circumference is considered as a measure of peripheral fat distribution, and it could be a good surrogate to assess bone metabolism in relation to hyperinsulinemia and diabetes [14,15]. Showed that this peripheral girth was related with insulin resistance and claimed that wrist circumference opens a new perspective in the prediction of cardiovascular risk [7]. Amini et al. [16] in a study of 3000 first-degree relatives of diabetic patients found a positive association between wrist circumference and cardio metabolic risk factors [16]. In addition, a recent prospective study demonstrated that wrist circumference was a significant predictor of development of diabetes and MetS as pre-diabetes state [9]. In the light of these findings, we wonder that whether wrist circumference was associated with MetS in patients with T2DM. In our study, after adjusting for age, onset age of diabetes and duration of T2DM, wrist circumference was positively associated with weight, BMI, WC, TG, and negatively associated with HDL, AUC-glucose in both genders. Our results were in generally in line with previous studies that wrist circumference was associated with components of MetS [9,10,16]. However, the results were not significant for SBP and DBP in both genders. This was supported by some studies [11,16], while it was in contradiction to those reached by others which demonstrated with wrist circumference as a novel predictor of hypertension [10].
In this cross-section analysis, wrist circumference was significant related with MetS in both genders as well. Most of hazard ratios for MetS could be explained by confounding effects of BMI and WC in both genders, respectively. However, after controlling for BMI or WC, the association remained significant only among females. Differences between the two genders regarding the association between wrist girth and metabolic risk factors have been reported by the other study, which demonstrated that wrist circumference could be a predictor of diabetes and MetS after controlling for BMI or waist circumference only among females [9]. The higher prevalence of MetS in female group than in male might contribute to find the association of wrist girth and MetS. These observations are generally in accordance with many other studies which reported that, female genders had higher hypertension, hyperglycemia and hyperlipidemia as compared to male counterparts, especially among the elder patients with diabetes [17-19]. The phenomena might be explained by estrogen deficiency, severe low-degree chronic inflammation in female patients [17,20]. Besides, it was reported that wrist circumference could be a good surrogate to assess bone metabolism in relation to hyperinsulinemia and diabetes [14,15]. Bones may also be involved as an endocrine organ in the regulation of whole-body glucose and energy metabolism [21,22]. Thus, the gender difference on bone metabolism might also attribute to the association of wrist girth and MetS in female patients [23,24]. However, when adjusted for BMI and WC, the association between wrist circumference and MetS remained significant only among the normal group women (BMI<25kg/m2). The similar observation has been reported by Mohebi R et al, which demonstrate that wrist circumference was an independent predictor for incident hypertension and cardiovascular disease events among non-centrally obese women [10]. As we known, both of bone tissue and adipose could regulate energy hemostasis and impact metabolism [21,25-27]. Thus, compared with obesity or overweight patients, the association between wrist circumference and metabolism might be more prominent in patients with normal weight, which might attribute to reduce the effect of adipose on metabolism. Further studies are required to confirm our findings. Limitations of this cross-sectional study were listed as following: first, there was no age matched normal control in the study, and because of all patients from hospitals but not from out-patient, a selection bias might exist in our study that. Those factors will limit the using of wrist circumference as a marker of metabolic syndrome; Second, assessment of wrist circumference levels was based on single measurements, which might underestimate the true strength of the association; Third, the number of samples is relatively small, large number of samples should be recruited to confirm our findings.
Conclusion
According to our results, in the middle-aged and elderly type 2 diabetic patients requiring admission to a large urban hospital in China, wrist circumference was significantly associated with MetS among even after adjustment for various characteristics in both genders as well. However, after considering other fat measures, the association remained significant only among the normal group women (BMI<25kg/m2).
Acknowledgment
The present study would not have been possible without the participation of these patients. This study was approved by the ethics committee of Shanghai Tenth People’s Hospital. This study is supported by grants from the Scientific Research Fund of Shanghai Shenkang (No. SHDC12012303).
References
- Alberti KG, Zimmet P, Shaw J (2005) The metabolic syndrome a new worldwide definition. Lancet 366(9491): 1059-1062.
- Cornier MA, Dabelea D, Hernandez TL (2008) The metabolic syndrome. Endocr Rev 29(7): 777-822.
- Cabre JJ, Martin F, Costa B (2008) Metabolic syndrome as a cardiovascular disease risk factor: patients evaluated in primary care. BMC Public Health 8: 251.
- Prasad DS, Kabir Z, Dash AK, Das BC (2012) Prevalence and risk factors for metabolic syndrome in Asian Indians: a community study from urban eastern India. J Cardiovasc Dis Res 3(3): 204-211.
- Salazar MR, Carbajal HA, Espeche WG (2011) Relationships among insulin resistance, obesity, diagnosis of the metabolic syndrome and cardio-metabolic risk. Diab Vasc Dis Res 8(2): 109-116.
- Reaven GM (2009) Is diagnosing metabolic syndrome a uniquely simple way to predict incident type 2 diabetes mellitus? CMAJ 180(6): 601-602.
- Capizzi M, Leto G, Petrone A (2011) Wrist circumference is a clinical marker of insulin resistance in overweight and obese children and adolescents. Circulation 123(16): 1757-1762.
- Mitrea A, Soare A, Popa SG (2013) Wrist circumference: an independent predictor of both insulin resistance and chronic kidney disease in an elderly population. Rom J Diabetes Nutr Metab Dis 20: 6.
- Noudeh YJ, Hadaegh F, Vatankhah N (2013) Wrist circumference as a novel predictor of diabetes and prediabetes: results of cross-sectional and 8.8-year follow-up studies. J Clin Endocrinol Metab 98(2): 777-784.
- Mohebi R, Mohebi A, Sheikholeslami F, Azizi F, Hadaegh F (2014) Wrist circumference as a novel predictor of hypertension and cardiovascular disease: results of a decade follow up in a West Asian cohort. J Amer Soc Hypertens 8(11): 800-807.
- Derakhshan A, Eslami A, Bozorgmanesh M, Sheikholeslami F, Azizi F, et al. (2016) Wrist circumference as a novel negative risk factor for cardiovascular disease among adult men: a median follow-up of 9 years. J Endocrinol Invest 39(7): 763-768.
- Li F, Cao H, Sheng C, Sun H, Song K (2016) Upregulated Pdx1 and MAFA contribute to beta-cell function improvement by sleeve gastrectomy. Obes Surg 26: 904-909.
- Yang W, Liu J, Shan Z, Tian H (2014) Acarbose compared with metformin as initial therapy in patients with newly diagnosed type 2 diabetes: an open-label, non-inferiority randomised trial. Lancet Diabetes Endocrinol 2(1): 46-55.
- Mora S, Pitukcheewanont P, Nelson JC, Gilsanz V (1999) Serum levels of insulin-like growth factor I and the density, volume, and cross-sectional area of cortical bone in children. J Clin Endocrinol Metab 84(8): 2780-2783.
- Freedman DS, Rimm AA (1989) The relation of body fat distribution, as assessed by six girth measurements, to diabetes mellitus in women. Am J Public Health 79(6): 715-720.
- Amini A, Soltanian N, Iraj B (2012) Association of wrist circumference with cardio metabolic risk factors. J Pak Med Assoc 62(3): S34-S36.
- Blaak E (2008) Sex differences in the control of glucose homeostasis. Curr Opin Clin Nutr Metab Care 11(4): 500-504.
- Callewaert F, Sinnesael M, Gielen E, Boonen S, Vanderschueren D (2010) Vanderschueren D. Skeletal sexual dimorphism: relative contribution of sex steroids, GH-IGF1, and mechanical loading. J Endocrinol 207(2): 127-134.
- Fukumoto S, Martin TJ (2009) Bone as an endocrine organ. Trends Endocrinol Metab 20(5): 230-236.
- Lee NK, Sowa H, Hinoi E (2007) Endocrine regulation of energy metabolism by the skeleton. Cell 130(3): 456-469.
- Paula FJ, Horowitz MC, Rosen CJ (2010) Novel insights into the relationship between diabetes and osteoporosis. Diabetes Metab Res Rev 26(6): 622-630.
- Leonard MB, Shults J, Wilson BA, Tershakovec AM, Zemel BS (2004) Obesity during childhood and adolescence augments bone mass and bone dimensions. Am J Clin Nutr 80(2): 514-523.
- Pollock NK, Laing EM, Baile CA, Hamrick MW, Hall D (2007) Is adiposity advantageous for bone strength? A peripheral quantitative computed tomography study in late adolescent females. Am J Clin Nutr 86(5): 1530-1538.
- Pollock NK, Laing EM, Hamrick MW, Baile CA (2011) Bone and fat relationships in postadolescent black females: a pQCT study. Osteoporos Int 22(2): 655-665.
© 2021, Manna Zhang. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






