- Submissions

Full Text
Cohesive Journal of Microbiology & Infectious Disease
Fragment Restoration (Reattachment of Anterior Tooth Fragment)
Anwar Sabti1 and Chaza Kouchaji2*
1Master pedodontics student, Syria
2Head of Syrian pedodontic associasion, Syria
*Corresponding author: Chaza Kouchaji, Head of Syrian Pedodontic Associasion, Syria
Submission: February 25, 2021; Published: March 22, 2021

ISSN 2578-0190 Volume5 issues1
Abstract
Coronal fractures of the anterior teeth are a common form of dental trauma that mainly affects children and adolescents. One of the options for managing coronal tooth fractures when the tooth fragment is available and there is no, or minimal violation of the biological width is the reattachment of the dental fragment. Reattachment of fractured tooth fragments can provide good and long-lasting esthetics (because the tooth’s original anatomic form, color, and surface texture are maintained). It also restores function, provides a positive psychological response, and is a relatively simple procedure. Patient cooperation and understanding of the limitations of the treatment is of utmost importance for good prognosis. This article reports on two coronal tooth fracture cases that were successfully treated using tooth fragment reattachment.
Clinical Significance
Reattachment of fractured tooth fragments offers a viable restorative option for the
clinician because it restores tooth function and esthetics with the use of a very conservative
and cost-effective approach. The majority of dental injuries involves the anterior teeth,
especially the maxillary incisors (because of its position in the arch), Several factors influence
the management of coronal tooth fractures, including extent of fracture (biological width
violation, endodontic involvement, alveolar bone fracture), pattern of fracture and restorability
of fractured tooth (associated root fracture), secondary trauma injuries (soft tissue status),
presence/absence of fractured tooth fragment and its condition for use (fit between fragment
and the remaining tooth structure), occlusion, esthetics, finances, and prognosis. Patient
cooperation and understanding of the limitations of the treatment is of utmost importance
for good prognosis. When there is a substantial associated periodontal injury and/or invasion
of the biological width, the restorative management of the coronal fracture should follow
the proper management of those associated issues. Coronal fractures must be approached
in a systematic way to achieve a successful restoration. Reattachment of a fragment to the
fractured tooth can provide good and long-lasting esthetics (because the tooth’s original
anatomic form, color, and surface texture are maintained),9 can restore function, can result
in a positive psychological response, and is a reasonably simple procedure. this technique
is less time-consuming and provides a more predictable long-term wear than when direct
composite is used.12 Clinical trials and long-term follow-up have reported that reattachment
using modern dentin bonding agents or adhesive luting systems may achieve functional and
esthetic success. In cases of complicated fractures, when endodontic therapy is required, the
space provided by the pulp chamber can be used as an inner reinforcement, thus avoiding
further preparation of the fractured tooth.15,16 However, in such cases, esthetics may become
an important issue as pulp less teeth lose part of their translucency and brightness.
This article reports on 0ne coronal tooth fracture case that were successfully treated
using tooth fragment reattachment (Figures 1-6).
Figure 1: Preoperative.

Figure 2:Pulp exposure.

Figure 3:Radiographe examination.
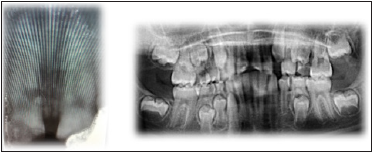
Figure 4: Radiographe examination.

Figure 5: Glass inomer plug.
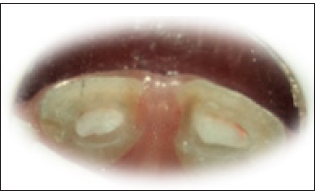
Figure 6: Glass inomer plug.

Case Report
A 11-year-old patient presented at the emergency clinic at the University of Damascus after sustaining a complicated crown fracture to his right and left central incisor during school Clinical and radiographic examination revealed a complicated oblique crown fracture with vital pulp exposure after endodontic therapy, the treatment options were presented to the patient and to her legal guardian, including (1) no treatment, (2) postand-core and crown, (3) crown buildup restoration with a resin based composite, and (4) reattachment of the tooth fragment. After some deliberation about the advantages, disadvantages, prognosis, and cost of every treatment option, the patient and the patient’s mother opted to have the tooth fragment reattached. The operating field was isolated to ensure moisture control. The endodontic temporary restorative material was removed from the pulp chamber, and the entrance of the root canal was sealed with a glass ionomer plug [1-3]. The pulp chamber, dentin, and enamel were etched with a 37% phosphoric acid gel, rinsed, and coated with an ethanol-based adhesive system and the fractured surface of the fragment was treated with 37% phosphoric acid gel for 30 seconds), followed by delicate rinsing. The adhesive system was then applied to the etched surface. Composite resin (Venus, Heraeus Kulzer, Dormagen, Germany) was applied to both fragment and tooth surfaces. The fractured segment was then accurately placed on the tooth, paying special attention to the fit between the segments. When the original position had been reestablished, excess resin was removed and the area was light cured for 40 seconds on each surface, making sure that no displacement of the fragment occurred before adhesive/resin polymerization was complete. The margins were properly finished with diamond burs and polished with a series of Sof-Lex disks and diamond polishing paste. The occlusion was carefully checked and adjusted, and the patient was dismissed after receiving instructions to avoid exerting heavy function on this tooth and to follow regular home care procedures relative to oral hygiene. The patient and the patient’s mother were informed that the reattachment line might be visible, and, if necessary, this could be managed in future visits. The patient returned for 1-, 6-, and 14-month follow-ups. Although the reattachment line can be noted in a close-up view, the patient was very satisfied with the results and opted not to have the line masked with a partial composite veneer [3-6].
References
- Reis A, Loguercio AD, Kraul A, Matson E (2004) Reattachment of fractured teeth: a review of literature regarding techniques and materials. Oper Dent 29(2): 226-233.
- Macedo GV, Diaz PI, Fernandes CA (2008) Reattachment of anterior teeth fragments: a conservative approach. J Esthet Restor Dent 20(1): 5-20.
- Mohammed K (2019) Reattachment of fractured teeth fragments in mandibular incisors. Int Med Case Rep 8: 87-91.
- Lo Giudice, Alibrandi A, Lipari F, Lizio A, Lauritano F, et al. (2017) The coronal tooth fractures: preliminary evaluation of a three-year follow-up of the anterior teeth direct fragment reattachment technique without additional preparation. Open Dent J 11: 266-275.
- Nupur Ninawe, Deoyani Doifode, Vishal Khandelwal, Prathibha Anand N (2013) Fragment reattachment of fractured anterior teeth in a young patient with a 1.5-year follow-up. BMJ Case Rep bcr2013009399.
- Georgia V, Patricia I, André V (2008) Reattachment of anterior teeth fragments: a conservative approach. J Esthet Restor Dent 20(1): 5-18.
© 2021 Chaza Kouchaji. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






