- Submissions

Full Text
Cohesive Journal of Microbiology & Infectious Disease
A Review of Reproductive Number of Pandemic Covid-19: Comparative Analysis of R Value
Sheta Biswas1a*, Anip Kumar Paul2a, Md. Al-Amin Molla2 and Anuz Kumar Chakrabarty2
1Department of Biochemistry and Molecular Biology, Noakhali Science and Technology University, Noakhali- 3814, Bangladesh.
2Department of General Educational Development, Daffodil International University, Dhaka-1207, Bangladesh.
aBoth authors contributed equally to this work.
*Corresponding author: Sheta Biswas, Department of Biochemistry and Molecular Biology, Noakhali Science and Technology University, Noakhali- 3814, Bangladesh.
Submission: October 05, 2020; Published: October 23, 2020

ISSN 2578-0190 Volume4 issues3
Abstract
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is one of the most devastating outbreaks witnessed in the last 100 years causing a global health concern.At the beginning of a COVID-19 infection caused by the novel coronavirus (SARS-CoV-2), there is a period of time known as the latency period. In order to epidemic progression many scientists have concentrated on calculating the average number of secondary cases caused by a primary case in the susceptible population, which is referred as basic reproductive number, Ro. In this paper, we have studied the effect of basic reproductive number on the outbreak situation as well as comprehended the transmission pattern of COVID-19 globally. We have analyzed several data of basic reproductive numbers to discuss and finally, capable of exhibiting the prediction of this disease. Finally, comparison of reproductive numbers for several countries are represented graphically for better understanding the present outbreak situation of pandemic, COVID-19.
Keywords: COVID-19;Reproductive number;Temperature and humidity;Transmission rate
Introduction
The novel coronavirus (COVID-19), at first originated in Wuhan City, Hubei Province, China, end of the December 2019 which is subsequently spread over most of the cities (continents) of the countries in the world. On 12th December 2019, a pneumonia case of unknown etiology was reported in Wuhan and thereby World Health Organization (WHO) was briefed that this disease had been transmitted all over the world very fast due to its high infection rate. Mysteriously, the impact of the disease is different in different countries. The COVID-19 has been transmitting very fast to most of the countries over the world. Since the infected rate of this virus is very high so we have focused on its effective reproductive number. The basic reproductive number of an infectious agent is the average number of infections generated by one case over the course of the infectious period, in a naïve, uninfected population [1]. The estimation of reproductive number depends on some methodological system, assumption on parameters choice, considering time period. On the basis of the current dynamic transmission of the novel coronavirus outbreaking situation, the reproductive rate is becoming high and changing aberrantly. COVID-19 is a viral particle with single-stranded RNA belong to the order of Nidovirales, family of Coronaviridae, and subfamily of Orthocoronavirinae [2]. This virus can infect mammals including human and animals, causing infectious manifestations ranging from common cold to more extreme respiratory, hepatic, enteric as well as neurological symptoms [3].
By characterizing the severity spectrum, and how severity of symptoms relates to infectiousness, will be critical for evaluating the feasibility of control and the likely public health impact of this epidemic. The exhaustive outbreaks of SARS (Severe Acute Respiratory Syndrome) and MERS (Middle East Respiratory Syndrome) outbreaks started in 2003 in China and Saudi Arabia and South Korea in 2012, respectively [4]. Furthermore, World Health Organization reported that there were more than 8000 confirmed cases of SARS in 26 countries and more than 2200 confirmed cases of MERS in 27 countries [5]. Compared with SARS, range of the outbreak of COVID-19 is much wider, and pandemic risk and transmission rate are higher than that’s of SARS. As COVID-19’s reproductive number (R) is 2.9 which is much higher than recorded reproductive number (R) of SARS (1.77) whereas, different COVID-19 studies show the basic reproduction ranges between 2.6 to 4.71 [6]. The role of basic reproductive number is very significant because this number offers the idea about the potentiality and severity of the outbreaks which will be conductive for identifying the critical information about the type of disease interventions, contagion as well as intensity.
Materials and Methods
Firstly, we have focused on the daily reproductive number (R-value) and then conducted a close comparison about the transmissibility of the disease among the different countries worldwide. The time frame was from 1st July 2020 to 14th July 2020. Further, we have accumulated available data through internet as well as popular public preprint servers (i.e., arXiv, bioRxiv, medRxiv, SSRN). We have collected data sample of R value, generated by Computer Science dept. at Beihang University, depending on their individual daily temperature and relative humidity for highly affected countries which are still in very contagious situation (source: http://covid19-report.com/#/r-value). Wang et al. [7] asserted that High temperature and humidity can be effective for reducing the transmission of COVID-19 while augmenting 1oC temperature and 1% relative humidity (RH) can reduce the R value by 0.026 (95% CI [-0.0395, -0.0125]) and 0.0076 (95% CI [-0.0108, -0.0045]), respectively [7]. Also, the same statistics of R value for U. S. counties varies as 0.020 (95% CI [-0.0311, -0.0096]) and 0.0080 (95% CI [-0.0150, -0.0010]), respectively. We collected daily reproductive number as well as represent those data values for selected countries and considering the transmitting pattern of coronavirus, we have classified our analysis into three categories: a) where new cases are increasing, b) where new cases are same, and c) where new cases are decreasing. Further, we revised the previous publication of the relevant peer reviewed study on 18th January, 2020 to 31th January, 2020 about the reproduction number in Wuhan City, Mainland China where the presented data ranges from 2.08 to 3.1 (95% credible interval, and so on). Finally, data extraction was adopted to extract information from each article to minimize the contradictory outcomes.
Result
COVID-19 has spread out so firstly through worldwide. By using the three-day average temperature and relative humidity up to and including the day the R value is measured since the World Health Organization (WHO) reports that coronavirus carriers are infectious 2 days before showing the pneumonia like symptoms. Absolute humidity of air means the mass of water vapor per cubic meter of air, relates to both temperature and relative humidity. In Figure 1 show the daily variation of R value which is measured based on temperature and relative humidity. We detect the countries where new infectious cases are increasing and R value in those country remain within the average range of 0.7-3.4 and shows that the lowest limit is in Saudi Arabia and peak point is in China. In Figure 1 have displayed the countries where new transmission cases are almost same due to their closer R value. In this category, Spain is holding the lowest transmission rate (0.48) whereas, the highest transmission rate is 1.3 in Turkey. Apart from this, another category includes in some countries where new infectious cases are decreased where R values is almost under the range from 0.62 to 2.6. In addition, R value is becoming slightly increasing in Switzerland after 10th June 2020 which is about 1.5.
Figure 1: The scenarios representing the corresponding change of the daily R value depending on temperature and humidity of the respected countries. In Figure 1(a), Figure 1(b) & Figure 1(c), we present the scenarios of the variations of R value considering “where new infectious cases are slightly increasing”, “where new infectious cases are fluctuating”, and “where new infectious cases are decreasing”, respectively.
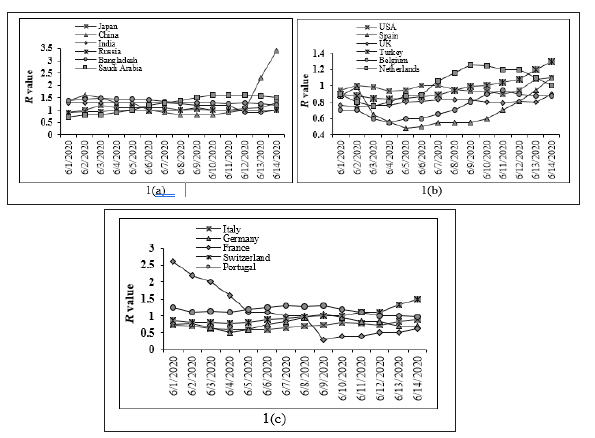
Figure 2:
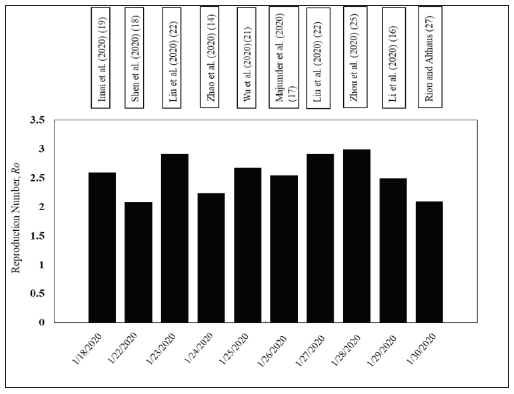
In Figure 2, illustrates the reproduction number which ranges from 2.08 to 3.0 (95% CI, and so on) which is gradually increasing from 18th January 2020 to 31st January 2020. Since high temperature and high humidity is the effective reason for reducing the transmission of COVID-19, so hopefully, in the summer season can actively play an important role to reduce slightly the transmission of the disease than in cold weather situation by diminishing the man to man contact rate which are still important for blocking the COVID-19 transmission.
Discussion
The third zoonotic human coronavirus of the century emerged in December 2019, with a cluster of pneumonia like syndrome originated in Wuhan city has not yet been effectively blocked. The basic reproductive number of the disease transmission (R) depends on several factors including climate conditions such as, temperature and humidity [7], population density, medical service [8,9]. Anyway, R have proportional relation with human to human contact rate and their body defense system while varying their local situation. As COVID-19 can be transmitted from person to person through direct contact or by droplets released by an infected person [6]. So, social distancing is very important and strictly maintain for blocking the COVID-19 transmission [7]. The Estimation of changes in transmission of disease over time, the epidemiologist can provide new perceptions into the existing situation [10] while identifying outbreak control have quantifiable effect [11,12]. Such exploration can inform the predictions about the potentiality of growth rate in future as well as to estimate the risk to other countries [13]. There are several researchers [1,7,14,15] found the basic reproduction number using different models. Susceptible- Exposed-Infectious-Recovered (SEIR) compartmental model is developed based on the clinical progression of the disease and estimated reproduction number was 6.47 (95% CI 5.71-7.23) [1]. Li et al. [16] have determined the value of the reproduction number ranging from 2.90 (95% CI 2.32-3.63) to 2.92 (95% CI 2.28-3.67) [16]. Zhao et al. [14] given a mode of transmission of COVID-19 through the exponential growth of the epidemic in mainland China from 10th to 24th January 2020 [14].
They estimated intrinsic growth rate by using the serial intervals (SI) of two other coronavirus diseases like MERS and SARS and obtained the basic reproduction number of COVID-19 ranging from 2.24 (95%CI: 1.96-2.55) to 3.58 (95% CI: 2.89-4.39). Another absolute reproductive number, Ro, estimation is varied from 2.0 to 3.1 (average 2.55) by Majumder MS [17] when data are collected from December 8, 2019 through January 26, 2020. Wang et al. [7] investigated the high temperature and relative humidity for reducing the transmission of COVID-19 [7]. Boldog et al. [15] investigated that the risk of COVID-19 as the number of cases in China is growing with increasing time and, estimated that the risks of outbreaks outside of China for imported cases such as international mobility patterns, control efforts, and secondary case distributions [15]. The Ro value of 2019-nCov is an indication of the initial transmissibility of the virus which is estimated as 4.71 is declined to 2.08 (1.99-2.18) on 22nd January 2020. If the declining trend continues with the assumption, Ro will drop below one within three months [18]. Estimating corresponds to the smallest level of zoonotic exposure, Ro is 2.6 in the level of giving a range of 1.5-3.5, assuming a total of 4000 cases by 18th January [19]. Yu [20] estimated that only a quarantine rate of infectious population higher than 90% would enable to effectively restrict the outbreak of coronavirus and estimated reproductive number is 3.5 [20]. On the basis of nowcasting and forecasting approach, the estimated basic reproductive number in China is 2.68 (95% CI 2.47-2.86) represented by Wu et al. [21] whereas, this number (Ro) is between 2.76-3.25 in Italy [21]. Around 12 modelling studies have recently reviewed that the mean value of Ro is 3.28, with a median of 2.79 in which two studies are stochastic methods and six studies are mathematical methods, the estimated Ro ranges from 2.2-2.68 and 1.5-6, respectively [22]. Ahmed J et al. [23] collected the data from Covid-19 affected 70 cities/provinces as well as analyzed the environmental data such as, temperatures, humidity and population density in each of these cities/provinces [23]. Thereby, they showed that average high temperature was the essential factor to diminish the augmentation of Covid-19 whereas, higher population density was an important factor for the prompt spreading of Covid-19. Since it was absolutely impossible to maintain the social distance, the virus can spread easily amongst the population. Hasan et al. [24] estimated daily reproductive number by using the exponential growth model for Bangladesh from March 8 to May 11, 2020 considering time-varying disease reporting rate and found the Ro to be 1.82 [95% CI: 1.81–1.84] without adjusting reporting rate [24]. Zhou et al. represent the basic reproduction number which fall between 2.8 and 3.3 using the real‐time reports on the number of 2019‐nCoV‐infected cases in China [25]. Liu et al. [26] considered exponential growth (EG) and maximum likelihood estimation model and found the Ro values as 2.90 (95%CI: 2.32- 3.63) and 2.92 (95%CI: 2.28-3.67), respectively [26]. Riou J [27] and Althaus CL estimated the Ro is 2.2 (90% high density interval: 1.4-3.8), indicating the potential for sustained human-to-human transmission [27].
Hu et al. [28] studied over 12 selected countries focusing on new confirmed cases as well as showing clear peak of the epidemic curve which is downfallen gradually, and also added that most of the estimated Ro monotonically were declined to be close to or less than 1.0 in April 30, 2020 except Singapore, South Korea, Japan, Iran, and South Africa [28]. Gunzler D [29] demonstrated that the reproduction number was declined from 4.02 to 1.51 between March 17 and April 1, 2020 in USA and consequently, the reproduction number for COVID-19 has been declined in most states over the past two weeks [29]. Depending on the different scenarios and levels of zoonotic exposure, the reproduction number was found to vary from 1.7 to 2.6 to 1.9 to 4.2. For instance, the WHO has estimated a reproduction number of 1.4 to 2.5. Thereby, Li and colleagues have computed a slightly higher value of 2.2 (95% CI 1.4 to 3.9), whereas other mathematical models published as pre-prints or undergone peer-review show the reproduction number varies from 1.3 to 4.7 [16]. These different findings vary because of applying different methodological issues, including different assumptions and choice of parameters, comparing updated versions, utilizing another model, using various datasets and also the period of estimation. More effective and timely precautions are required in order to control the further extension of 2019‐nCoV very quickly. By analyzing the current fluctuating characteristics of R value, the decision maker can implement the ongoing and upcoming accomplishments which will be effective for the respective mankind’s against the outbreaking potentiality of pandemic COVID-19. Further research is needed to estimate a more accurate Ro for this pandemic in the outbreak situation. We demonstrate here the R value of COVID-19 and try to represent the tendency of spreading situation based on some epidemiological data.
Conclusion
Coronavirus is spreading out worldwide drastically with highly reproduction numbers (0.5-4.9). Presently, a fourth large-scale outbreak is occurring and spreading out in almost every country in the world. The high reproduction number of this disease indicates that the outbreak of COVID-19 become more complicated than what has been reported so far, given the particular season of increasing social contacts, warranting effective, strict public health measures aimed to lessen the burden generated by the spreading of this virus. Since the infected rate of this virus is very high and second time infected chance are also increasing that is why we have focused on its reproductive number to prevent the outbreaking situation.
Acknowledgement
The authors would like to acknowledge anonymous colleagues for helpful comments.
References
- Tang B, Nicola LB, Qian Li, Sanyi T, Yanni X, et al. (2020) An updated estimation of the risk of transmission of the novel coronavirus (2019-nCov). Infect Dis Model 5: 248-255.
- Carlos WG, Charles S DC, Bin C, Shazia P, Shazia J, et al. (2020) Novel wuhan (2019-nCoV) coronavirus. Am J Respir Crit Care Med 201(4): P7-P8.
- Zhu N, Dingyu Z, Wenling W, Xingwang Li, Bo Y, et al. (2020) A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med 382(8): 727-733.
- Gralinski LE, Vineet DM (2020) Return of the Coronavirus: 2019-nCoV. Viruses 12(2): 135.
- http://www.emro.who.int/pandemic-epidemic-diseases/mers-cov/mers-situation-update-july-2018.html
- Hamid S, Mohammad YM, Gulab KR (2020) Noval coronavirus disease (COVID-19): a pandemic (epidemiology, pathogenesis and potential therapeutics). New Microbes New Infect 35: 100679.
- Wang J, Ke T, Kai F, Weifeng Lv (2020) High temperature and high humidity reduce the transmission of COVID-19. SSRN pp. 458-489.
- Hemmes JH, Kcf W, Kool SM (1960) Virus survival as a seasonal factor in influenza and poliomyelitis. Nature 188: 430-431.
- Dalziel BD, Stephen K, Julia RG, Cecile V, Ottar NB, et al. (2018) Urbanization and humidity shape the intensity of influenza epidemics in US cities. Science 362(6410): 75-79.
- Camacho A, Adam K, Yvonne AS, Mark AW, Stefan F, et al. (2015) Temporal changes in ebola transmission in sierra leone and implications for control requirements: a real-time modelling study. PLoS Curr 7: 25-56.
- Funk S, Iza C, Amanda T, Etienne G, Anton C, et al. (2017) The impact of control strategies and behavioural changes on the elimination of Ebola from Lofa County, Liberia. Philos Trans R Soc Lond B Biol Sci 372(1721): 20160302.
- Riley S, Christophe F, Christl AD, Azra CG, Laith J AR, et al. (2003) Transmission dynamics of the etiological agent of SARS in Hong Kong: impact of public health interventions. Science 300(5627): 1961-1966.
- Cooper BS, Richard JP, John EW, Nigel JG (2006) Delaying the international spread of pandemic influenza. PLoS Med 3(6): e212.
- Zhao S, Qianyin L, Jinjun R, Salihu SM, Guangpu Y, et al. (2020) Preliminary estimation of the basic reproduction number of novel coronavirus (2019-nCoV) in China, from 2019 to 2020: A data-driven analysis in the early phase of the outbreak. Int J Infect Dis 92: 214-217.
- Boldog P, Tamás T, Zsolt V, Attila D, Ferenc AB, et al. (2020) Risk assessment of novel coronavirus COVID-19 outbreaks outside China. J Clin Med 9(2): 571.
- Li Q, Xuhua G, Peng W, Xiaoye W, Lei Z, et al. (2020) Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N Engl J Med 382(13): 1199-1207.
- Kenneth DM (2020) Early transmissibility assessment of a novel coronavirus in Wuhan, China. SSRN 3524675.
- Shen M, Zhihang P, Yanni X, Lei Z (2020) Modelling the epidemic trend of the 2019 novel coronavirus outbreak in China. Bio Rxiv 2020.
- Imai N, Anne C, Ilaria D, Marc B, Christl A, et al. (2020) Report 3: Transmissibility of 2019-nCoV. Imperial College London. UK.
- Yu X (2020) Updated estimating infected population of Wuhan coronavirus in different policy scenarios by SIR model. Infectious Diseases: Comments.
- Wu JT, Kathy L, Gabriel ML (2020) Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: a modelling study. Lancet 395(10225): 689-697.
- Liu Y, Albert AG, Annelies WS, Joacim R (2020) The reproductive number of COVID-19 is higher compared to SARS coronavirus. J Travel Med 27(2): 21.
- Ahmed J, Hasna JM, Goutam S, Pratyya G (2020) Effect of temperatures, humidity and population density on the spreading of covid-19 at 70 cities/provinces. Preprints, pp. 158-198.
- Hasan M, Akhtar H, Wasimul B, Syed SI (2020) Estimation of the basic reproduction number of novel coronavirus (COVID-19) in Bangladesh: A 65-day outbreak data-driven analysis. Bangladesh.
- Zhou T, Quanhui L, Zimo Y, Jingyi L, Kexin Y, et al. (2020) Preliminary prediction of the basic reproduction number of the Wuhan novel coronavirus 2019‐nCoV. J Evid Based Med 13(1): 3-7.
- Liu T, Jianxiong H, Min K, Lifeng L, Haojie Z, et al. (2020) Transmission dynamics of 2019 novel coronavirus (2019-nCoV). USA.
- Riou J, Christian LA (2020) Pattern of early human-to-human transmission of Wuhan 2019 novel coronavirus (2019-nCoV), December 2019 to January 2020. Euro Surveill 25(4): 2000058.
- Fu CH (2020) The estimated time-varying reproduction numbers during the ongoing pandemic of the coronavirus disease 2019 (covid-19) in 12 selected countries outside China. Med Rxiv.
- Gunzler D, Ashwini RS (2020) Time-varying COVID-19 reproduction number in the United States. Med Rxiv 4(10): 20060863.
© 2020 Sheta Biswas. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






