- Submissions

Full Text
Approaches in Poultry, Dairy & Veterinary Sciences
Diagnosis and Treatment of Canine Babesiosis in Pakistan, A Case Report
Sami Ullah Khan Bahadur1, Razia Kausar2*, Hunain Ahmed1 and Usman Talib1
1 Department of Veterinary Medicine, University of Agriculture Faisalabad, Pakistan
2 Department of Veterinary Anatomy, University of Agriculture Faisalabad, Pakistan
*Corresponding author: Razia Kausar, Assistant Professor, Department of Veterinary Anatomy, Faculty of Veterinary Science, University of Agriculture Faisalabad, Pakistan
Submission: July 05, 2018;Published: September 12, 2018

ISSN: 2576-9162 Volume5 Issue1
Summary
A German shepherd bitch of age 2 years, weighing 20kg, was presented at Clinical Medicine and Surgery Department of University of Agriculture Faisalabad, Pakistan. Anamnesis revealed of anorexia since 12 days, 2 episodes of emesis, brown urine and excessive water intake and intermittent lethargy. Visually, bitch was emaciated with dull hair coat. Clinical examination showed increased temperature, heart rate and respiration rate of 104.2 oF, 128/min and 54/min, respectively along with pale conjunctiva and mucous membrane, increased CRT and skin tent twisting time. For diagnosis, examination of stained thin blood smear under microscope and complete blood count (CBC) was performed. The blood examination and CBC report declared the case of canine babesiosis which was treated with single shot of IMIDOCARB DIPROPIONATE, Doxycycline Monohydrate for 21 days and metronidazole for 7 days. Supportive therapy was also given until proper feed intake. Bitch recovered completely when the treatment regime of 21 days ended.
Keywords: Livestock; Crop; Integration; Benefit; Farming community
Introduction
Babesiosis is tick borne, intraerythrocytic parasitic, economically significant disease of dogs, livestock, horses, and rodents [1]. More than 100 species of Babesia are known to cause disease in different species, Babesia canis, Babesia gibsoni, and Babesia annae are species of Babesia causing disease in dogs [2]. B. canis is about 4 times more prevalent than B. gibsoni in Pakistan [3] Babesia has been placed in order Aconoidasida, family Piroplasmida, and genus babesidae [National Centre for biotechnology Information: taxonomy browser]. This disease has not only veterinary importance but also has zoonotic potential. B. microti and B. divergens species mostly infect humans [1]. Rhipicephalus species of ticks are major vector for the transmission of disease however Dermacentor reticularis transmit Babesia canis, Haemaphysalis bispinosa and Haemaphysalis longicornis transmit Babesia gibsoni. Anemia and fever are main clinical manifestations of Babesiosis in dog due to intravascular and extravascular hemolysis [4]. In Lahore-Pakistan, overall prevalence of canine Babesiosis was found to be 12.49% and 13.97% in the years of 2004 and 2005, respectively [3]. It is reported that categories of male dogs, young age < 2 years and cross-bred are more prone to babesiosis as compared to their other respective categories [5]. Disease can be controlled with the use of tick sprays, hygienic conditions and communicating dog owners about control strategies. Disease is hyper-endemic in summer as compared to other seasons [3]. This increased prevalence in summer is related with increased tick population in this season. Due to hot and humid weather of Pakistan, occurrence of babesiosis is being increased. In this report, diagnosis and treatment regime for canine babesiosis case has been described.
Case Presentation
A German shepherd bitch of 2 years age, weighing approx. 20kg was presented to Clinical Medicine and Surgery Department, University of Agriculture Faisalabad-Pakistan with the history of anorexia since 12 days, 2 episodes of emesis, brown urine and excessive water intake. On investigation, owner told about depression of the patient intermittently. Regular vaccination and deworming schedule was being followed. Dog food and boiled chicken was being fed to bitch before anorexic condition. Visually, bitch was emaciated with dull coat (Figure 1). Clinical examination revealed increased temperature, heart rate and respiration rate of 104.2 oF, 128/min and 54/min, respectively along with pale conjunctiva and mucous membrane, increased CRT and skin tent twisting time. On the basis of this examination, bitch was found to be anemic and dehydrated. Lymph nodes were normal in size. Fecal sample collected for examination of GIT parasites, showed absence of ova. Blood was collected from ear vein to form thin film smear and from cephalic vein for Complete Blood Count (CBC).
Figure 1:

Figure 2:
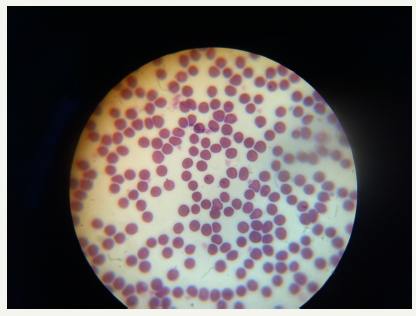
Thin blood smear was stained with field stain and examined under 100X of compound microscope which revealed erythrocytic parasite (Figure 2). Complete Blood Count (CBC) report showed anemia with decreased erythrocytic count, Hematocrit and Hemoglobin level of 3.7x1012/L, 23.4% and 8.2g/dL, respectively. Thrombocytopenia (which occur due to destruction and sequestration in spleen) with platelet count of 53x109 and lymphocytosis with 88.4% lymphocytes was present.
[Normal reference values of CBC for dog are RBC’s count= 4.95-7.87x1012/L, PCV/Hematocrit=35-57%, Hb=11.9-18.9g/dL, platelets=211-621x109/L and lymphocytes=8-21% of total White blood cells. (https://www.msdvetmanual.com/appendixes/reference- guides/hematologic-reference-ranges)]. On the basis of history, clinical examination, CBC report and blood smear examination, disease was diagnosed as Canine babesiosis. Babesiosis should be differentially diagnosed from conditions which cause haemolysis, anemia, icterus and fever. Ehrlichiosis, Acute anemia, Lyme disease, Q-fever and typhoid fever can confuse while diagnosing babesiosis but examination of stained blood smear and ELISA are confirmatory for canine babesiosis.
This case of bitch infected with Babesiosis was treated with single shot of IMIDOCARB DIPROPIONATE @ 5mg/kg subcutaneous route, Doxycycline Monohydrate 100mg/day P.O for 21 days and metronidazole 200mg/day for 7 days to minimize the damage produced by Babesia because no drug can eliminate it completely. To resuscitate dehydration and maintain energy level, infusion of 5% Dextrose and Lactated Ringer (Ringolact-d, Otsuka Pakistan Ltd.) 400ml/day for 4 days was administered through IV route. Infusions are advantageous in this case if administered accurately. To overcome the adverse reactions of Imidocarb, 1ml (1mg) atropine sulphate and 1ml (4mg) dexamethasone sodium phosphate was given 10min before, intramuscularly.
Result
The bitch showed very good response against treatment prescribed and recovered completely. After 21 days of medication, bitch became healthy with normal haematological values. In Pakistan diagnosis of canine babesiosis can be made on the basis of examination of stained blood smear, haematological values as mentioned in this case. In such instances of Canine babesiosis, drugs mentioned above are very good choice.
Discussion
World-wide distributed protozoal disease of Babesiosis is caused by Babesia, victimize multiple species of animals. This disease is most economically important for cattle industry [6] but Canine babesiosis is becoming more prevalent and major problem in dogs. Disease is transmitted by ticks. In Pakistan, most prevalent vector for transmission of the disease is Rhipicephalus [5]. Disease burden is related with density of ticks in an area, so disease is more prevalent in summer season, due to hot and humid environment that is favourable for ticks. Other modes of transmission for Babesiosis include blood transfusion and dog bite [7]. Transplacental transmission from dam to offspring has also been reported [8]. In such cases, disease is seen in very young age.
Pathogenesis of Canine Babesiosis in different regions differs [9]. In general Babesia is transmitted by ticks after 3 days of bite and enter into blood. In blood, attach with RBCs and enter RBCs through endocytosis. Intravascular and extravascular haemolysis lead to haemolytic anemia and hypotensive shock. Clinically Babesiosis is manifested with anorexia fever, tachycardia, tachypnoea haemoglobinurea, pale mucous membrane and splenomegaly. Paraplegia is also a rarely reported sign of Canine Babesiosis [10]. Proteinuria with concentrated urine are also seen in canine babesiosis [11]. Disease is not fatal if diagnosed and treated in early stage of disease, prognosis become poor if case become complicated. Blood parasitism is considered when fever persist even after giving anti- pyretic. The more replication of babesia and RBCs lysis is, the more severe disease is. Immunosuppression and splenectomy are also conditions which can be risk factors for Canine Babesiosis.
Diagnosis of Babesiosis in dog is based on symptoms observed, examination of diff quick stained blood smear under 100X lens of compound microscope when the case is no more complicated while PCR and serological detection are tools to diagnose complicated/ chronic cases. Clinical signs have been described earlier, for smear formation blood is collected from peripheral vein e.g. ear or tail veins. The percentage of affected RBCs examined varies and can reach up to 10% [12]. Acute phase protein level in serum increases whenever there is inflammation or body damage. Level of acute phase proteins including C-reactive protein CRP and ceruloplasmin is intensified while that of haptoglobin is reduced in Babesia canis [13]. This is another way to diagnose and to check the severity of disease but for that there is need to develop simple tests for the detection of acute phase protein’s level in serum. Serological testing with ELISA can differentiate between B. canis and B. gibsoni [14]. Prevalence of ticks and disease in an area and season are contributory factors for diagnosis of Babesia specifically in countries like Pakistan where advanced testing is not affordable.
Different types of drugs are available used as treatment of babesiosis. Imidocarb dipropionate, diminazine aceturate (antiprotozoal drugs) are mostly prescribed with antibiotics Doxycycline or Enrofloxacin. Metronidazole is another choice. Atovaquone and azithromycin combination has also been proved effective against Babesia gibsoni, but Asian genotypes of B. gibsoni are thought to be resistant for this combination of atovaquone and azithromycin. There is no drug available which can eliminate the disease pathogen completely [2]. Supportive therapy with blood or electrolytes is also crucial in case of Babesiosis. In Pakistan, single shot imidocarb dipropionate 3.5-5mg/kg injectable along with oral doxycycline is prescribed. Supportive therapy with Ringer lactate and vitamin B complex (Neurobion®) are also prescribed. No drug can eliminate the parasite completely from an infected patient and even if recovered, relapse is also seen.
For the control of every disease, to know the paths of transmission of pathogens is very crucial. The main culprit for transmission of babesiosis is ticks. Controlling ticks is controlling Babesiosis. Dipping, spraying and tick collars are ways to control ticks. Owner should be advised to check their pets for ticks daily and provide them hygienic condition. Fipronil spray (Frontline ®) is easily available in Pakistan for the control of ticks on dogs. Dog bite and blood transfusion are also source of spread so dog fight should be strictly prohibited and blood of donor should be tested for haemo-parasites before transfusion.
References
- Vial HJ, Gorenflot A (2006) Chemotherapy against babesiosis. Vet Parasitol 138(1-2): 147-160.
- Birkenheuer AJ, Levy MG, Breitschwerdt EB (2004) Efficacy of combined atovaquone and azithromycin for therapy of chronic Babesia gibsoni (Asian genotype) infections in dogs. J Vet Intern Med 18(4): 494-498.
- Ahmad SS, Khan MS, Khan MA (2007) Prevalence of canine babesiosis in Lahore. The Journal of Animal and Plant Sciences (Pakistan) 17: 11-13.
- Schoeman JP (2009) Canine babesiosis. Onderstepoort J Vet Res 76(1): 59-66.
- Bashir IN, Chaudhry ZI, Ahmed S, Saeed MA (2009) Epidemiological and vector identification studies on canine babesiosis. Pakistan Vet J 29(2): 51-54.
- Mosqueda J, Olvera Ramirez A, Aguilar Tipacamu G, Canto GJ (2012) Current advances in detection and treatment of babesiosis. Curr Med Chem 19(10): 1504-1518.
- Birkenheuer AJ, Correa MT, Levy MG, Breitschwerdt EB (2005) Geographic distribution of babesiosis among dogs in the United States and association with dog bites: 150 cases (2000-2003). J Am Vet Med Assoc 227(6): 942-947.
- Fukumoto S, Suzuki H, Igarashi I, Xuan X (2005) Fatal experimental transplacental Babesia gibsoni infections in dogs. Int J Parasitol 35(9): 1031-1035.
- Saud N, Hazarik GC (2000) Studies on incidence and biochemical changes of babesia infection in dogs. Indian Veterinary Journal J 77(11): 944- 947.
- Jacobson LS (2006) The South African form of severe and complicated canine babesiosis. Clinical advances 199-2004. Vet Parasitol 138(1-2): 126-139.
- Lobetti RG, Jacobson LS (2001) Renal involvement in dogs with babesiosis. J S Afr Vet Assoc 72(1): 23-28.
- Van Heerden J, Reyers F, Stewart CG (1983) Treatment and thrombocyte levels in experimentally induced canine ehrlichiosis and canine babesiosis. Onderstepoort Journal of Veterinary Research 50: 267-270.
- Ulutas B, Bayramli G, Ulutas PA, Karagenc T (2005) Serum concentration of some acute phase proteins in naturally occurring canine babesiosis: a preliminary study. Vet Clin Pathol 34(2): 144-147.
- Verdida RA, Hara OA, Xuan X, Fukumoto S, Igarashi I, et al. (2004) Serodiagnosis of Babesia gibsoni infection in dogs by an improved enzyme- linked immunosorbent assay with recombinant truncated P50. J Vet Med Sci 66(12): 1517-1521.
© 2018 D Udhaya Nandhini. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






