- Submissions

Full Text
Associative Journal of Health Sciences
Incision to Delivery Times in Preterm Cesarean Deliveries and Outcomes: An analysis in Neonates
Aksal Vashi BS1*#, Peggy Palsgaard BS1#, Aashka Shah BS1#, Joseph O Connell DO1,2# and Joseph M Maurice MD, MS3#
1Carle Illinois College of Medicine, University of Illinois at Urbana-Champaign, Urbana, Illinois
2Department of Neonatology, Carle Foundation Hospital, Urbana, Illinois
3Department of Obstetrics and Gynecology, Creighton University School of Medicine
#These authors contributed equally to this work
*Corresponding author:Aksal Vashi, Carle Illinois College of Medicine, University of Illinois at Urbana- Champaign, Urbana, Illinois, USA
Submission: March 11, 2024;Published: March 26, 2024

ISSN:2690-9707 Volume3 Issue2
Abstract
Certain aspects of a cesarean delivery, such as skin incision to delivery time and uterine incision to delivery time, have been studied in term deliveries and have not yet yielded relationships with negative neonatal outcomes. However preterm cesarean deliveries have not been studied in the same capacity. Through a retrospective chart review of 706 preterm cesarean deliveries, this study aims to assess the relationship between skin incision to delivery, uterine incision to delivery and neonatal hypoxia. Overall, skin incision to delivery time had no significant statistical relation to hypoxic outcomes in preterm neonates. While uterine incision to delivery time did have an significant association with hypoxic outcomes and factors that make surgical procedures more difficult (increased BMI, maternal age), this relationship did not exist when controlling for gestational age. With further studies, these findings could inform and influence the strategies obstetricians utilize during preterm cesarean deliveries.
Keywords:Neonate; Hypoxia; Preterm; Incision time
Introduction
Cesarean Deliveries (CD) made up 31.7 percent of births in 2019 [1]. A cesarean delivery is one of the most commonly practiced surgical procedures in the United States [2,3]. One challenging aspect of a cesarean delivery is the time between uterine incision and delivery. Studies demonstrated no clear relationship between uterine incision and delivery [4-7]. The largest study these authors could identify was a prospective cohort of 812 patients, which identified no relationship between uterine incision to delivery time and hypoxic neonatal outcomes [4] Notably, most studies excluded preterm cesarean deliveries [4-7]. Preterm deliveries are associated with worse neonatal outcomes including hypoxia [8]. A physiological challenge for a newborn is transitioning from lungs filled with fluid to lungs filled with air. Preterm cesarean delivery is well known to make this a more challenging transition [9]. Thus, any small intervention done during a cesarean procedure has the potential to impact neonatal outcomes. This study seeks to examine if time from skin incision to delivery and uterine incision to delivery significantly contributes to preterm neonatal hypoxia.
Methods
Data collection
This retrospective cohort study was performed by chart review for all preterm cesarean deliveries at Carle Foundation Hospital between January 1, 2017, through December 31, 2020. This study was conducted at a single academic institution and deemed exempt by the Carle Foundation Hospital Human Subject Protection Office. Inclusion criteria included all preterm neonates born by cesarean delivery at less than 37 weeks gestation. Multifetal gestations and mal-presented fetuses were excluded in this study. No preexisting conditions were excluded.
Data was retrieved from maternal and neonatal medical records including demographic characteristics, gestational age, procedure timing records, cesarean indication, and blood gases. Surgical times were extracted from the nursing record. Data was exported to a REDCap database.
Hypoxic outcomes were defined based on pH, lactate, base excess, and respiratory support as previously described [4]. The criteria were as follows: umbilical arterial pH less than 7, base excess greater than negative 16, five-minute apgar less than 5, and need for respiratory support in the first 10 minutes of life [4]. Neonate was considered to have a hypoxic outcome if any of these criteria were met.
Statistical analysis
Demographic and maternal/neonatal risk factor (i.e., age, race, BMI, GDM, indication for cesarean etc.) comparisons were conducted between the patients within the upper quartile of skin and uterine incision to delivery times (>8 min and >60 seconds, respectively) and the lower three quartiles of patients. Significance was determined using a two-tailed t-test with F-test two-sample for variances.
Relative risk was calculated comparing rates of hypoxic outcomes in increasing skin incision to delivery and uterine incision to delivery times. Uterine incision to delivery time was divided into 60 second increments (0-60, 61-120, 121-180, >180) as previously described [4]. Skin incision to delivery time was divided into <120 seconds, 121-300 seconds, 301-480 seconds, and >480 seconds. Both were compared to rates of neonatal hypoxic outcomes. Preterm deliveries were divided into extremely preterm (<28 weeks), very preterm (<32 weeks), moderately preterm (32 to <34 weeks), and late preterm (34 to <37 weeks) and respective rates of hypoxic outcomes were compared to skin and uterine incision to delivery times [10]. Significance for all statistical analysis was set to p<0.05.
Result
Our initial dataset included 706 deliveries; 520 deliveries had a documented uterine incision to delivery time and 694 deliveries had a documented skin incision to delivery time. The median time from uterine incision to delivery was 0.93 minutes, while the median skin incision to delivery time was 6.47 minutes. As seen in Table 1, longer skin incision to delivery times were positively correlated with advanced maternal age (p < .0001), higher BMIs (even while stratified by BMI >30, p<0.0001), rates of gestational diabetes mellitus (p=0.001), prior CD (p<0.0001), and heavier birth weights (p=0.007). Patients with advanced maternal age (p=0.023), and lower gestational age (p=0.004) were more likely to have a longer uterine incision to delivery time. Non reassuring fetal status (p=0.018) and placental abruption (p = 0.01) were indications for cesarean delivery that were associated with a shorter skin incision to delivery time, meanwhile prior cesarean (p<0.0001) and abnormal placentation (p=0.006) were associated with increased skin incision to delivery time. No indications for CD were associated with variations in uterine incision to delivery time. As outlined in Table 1, no indications for CD were associated with the upper quartile for both skin and uterine incision to delivery times.
Table 1:Numerical description of samples and phenotype.

In the analysis of hypoxic morbidity, outcomes were compared based on 60 second intervals for uterine incision to delivery times (Table 2). For all gestational ages, hypoxic outcomes were seen in 66.04% for less than 60 seconds [n=427], 68.33% for 61- 120 seconds [n=60], 95.24% for 121-180 seconds [n=21], and 64.29 for greater than 180 seconds [n=14] (p=0.049). Acidemia (p =0.000028), pH<7.2 (p<0.00001), lactate >8 (p=0.015), and neonatal death (p=0.045) were each associated with elevated uterine incision to delivery times. Changes in rates of base excess <-8 were not significant as seen in Table 2.
Table 2:Uterine incision time Vs Neonatal hypoxic outcomes.

The prevalence of neonatal hypoxic outcomes was not associated with changes in skin incision to delivery time (Table 3). For changes in skin incision to delivery time, lactate >8 (p=0.0115) was the only factors found to vary significantly.
Table 3:Skin incision time Vs Neonatal hypoxic outcomes.

Finally, hypoxic outcomes amongst preterm neonates were associated with a significantly elevated uterine incision to delivery time (p=0.034) but not any variation in skin incision to delivery time (Tables 4&5). When controlled for gestational age, neither uterine nor skin incision to delivery times were associated with individual hypoxic outcomes.
Table 4:Average uterine incision to delivery time stratified by hypoxic outcomes and gestational age.
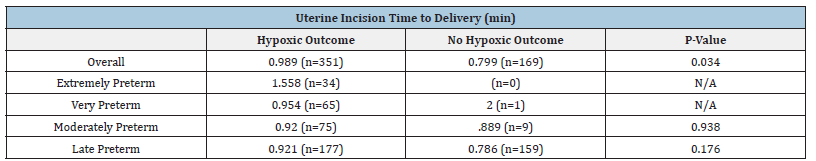
Table 5:Average skin incision to delivery time stratified by hypoxic outcomes and gestational age.

Discussion
Data from this study will be the first insight into skin and uterine incision to delivery times impact in preterm Cesarean deliveries and could help drive decision making for obstetric physicians across the country. Overall, skin incision to delivery time had no significant statistical relation to hypoxic outcomes in preterm neonates. This was true both for when stratified by gestational age as well as by time intervals of skin incision to delivery. There was an association between lower pH and a faster skin incision to delivery time, however considering that no other hypoxic factors were significant, this is likely not a clinically significant finding. This further supports other findings for term pregnancies that indicate skin incision to delivery does not affect outcomes [6,7].
Skin incision to delivery time has a direct relationship to maternal factors such as age, BMI, and prior cesarean; these findings may be due to increased difficulty of surgical procedures with increased scar tissue from a prior cesarean and increased BMI. No indications for Cesarean delivery were significantly associated with increased skin or uterine incision to delivery time, except for chorioamnionitis. This finding is consistent with expectations that surgical procedure is similar regardless of indication.
Unlike skin incision, uterine incision to delivery time did have a significant association with hypoxic outcomes in the overall preterm sample. Longer uterine incision to delivery times were associated with factors that make surgical procedures more difficult, such as increased BMI and maternal age. It is important to note that the extent to which a neonate is born preterm can serve as a significant confounding factor: a 36-week-old delivery will have vastly different outcomes than a 24-week-old delivery. Thus, our study controlled for gestational age. When assessing the relationship in each preterm cohort (extremely preterm, very preterm, moderate preterm, and late preterm), uterine incision to delivery time was no longer a significant predictor of hypoxic outcomes. When controlling for gestational age, the sample size was much smaller for extremely preterm (less than 28 weeks) and very preterm (28 to 32 weeks) births. There were only 55 extremely preterm neonates in this study (vs 99 late preterm) and all of these neonates met our hypoxic outcome criteria. This is important to note because given our t-test analysis, comparing to the “no hypoxic outcome” group with an n=0 or 1 was impossible. Given all extremely preterm neonates required supplemental oxygen due to lack of fetal lung maturity, our study design is limited in its ability to differentiate how uterine incision to delivery time affects hypoxic outcomes within this subgroup of preterm neonates. Further investigation using more specific criteria to designate the severity of hypoxic outcomes amongst this population would likely be required.
There may exist a relationship of progressive importance as gestational age decreases; we must weigh three findings of our data against one another to interpret this. First, there is no statistically significant relationship between uterine incision to delivery time and hypoxic outcomes in moderate and late preterm neonates; second, the youngest gestational age subgroup was unable to be calculated due to no patients with non-hypoxic outcomes. Finally, the overall sample of preterm births did have a significant relationship between uterine incision to delivery time and rates of hypoxic outcomes. If a true relationship did exist, we would expect that the “older” preterm groups would remain significant, however they did not. It is possible that the relationship identified is the confounding variable of the younger neonates having more difficult deliveries and always having a hypoxic outcome. In future studies, stratifying hypoxic outcomes by severity would allow for differentiation.
As uterine incision to delivery time increased, there was an increase in factors of hypoxic outcomes with notable exceptions of hypoxic morbidity, neonatal demise, and elevated base excess. Given the high sample size of neonates with hypoxic morbidity, we believe this further supports no significant relationship between uterine incision time and hypoxic outcomes.
Conclusion
Our findings are thus in agreement with previous studies performed on term neonates. A 2015 study found no relationship between uterine incision to delivery time and hypoxic outcomes with an average gestational age at delivery of 39.3 weeks [4]. Another study found transient tachypnea was not related with procedure time, anesthesia induction to delivery time, or uterine incision to delivery time in 100 subjects. This study was limited in its exclusion of pre-existing maternal conditions, emergency C-sections, maternal drug intake prior to CDs, as well as other factors [5]. A retrospective study in Israel demonstrated no impact of anesthesia induction to delivery time, skin incision to delivery time, or uterine incision to delivery time on neonatal outcomes. This study looked at gestational ages 37-42 weeks (mean of 38.3 weeks) and considered many postnatal complications. These included respiratory distress, hypoglycemia, need for phototherapy, among others [6]. Uterine incision to delivery time has also been studied in the context of vertical versus transverse incisions and found to have no significant difference in preterm delivery outcomes [11].
Our study was not without limitations, some of which have been defined above. The relationship between uterine incision to delivery time and hypoxic outcomes is difficult to interpret due to our smaller sample sizes amongst lower gestational ages. We believe that with larger sample sizes amongst extremely and very preterm neonatal groups, as well as a method of differentiating the severity of hypoxic outcomes, there would be a more distinct, observable relationship between uterine incision time and hypoxic outcomes amongst preterm neonates if one exists. Thus, future studies could include larger sample sizes across gestational age and determine a wider range of defining hypoxic outcomes to further elucidate if uterine incision to delivery time affects neonatal outcomes. If expanded appropriately, we believe these findings could be used in further educating surgical approaches to preterm neonatal CD’s across the world.
Additional Information
Conflict of interest
No authors have competing financial interests in relation to the work described.
This study was approved and deemed exempt by the Carle Foundation Hospital Human Subject Protection Office. The study was performed in accordance with the Declaration of Helsinki.
.Availability of data and materials
Dataset can be made available to readers promptly on request. No funding was received for this study.
Author statement and contributions
A. AV: Conceptualization, Methodology, Investigation, Data
Retrieval, Data Analysis, Data Interpretation, Writing - Original
draft, Writing - Review and Editing.
B. PP: Conceptualization, Methodology, Investigation, Data
Retrieval, Data Analysis, Data Interpretation, Writing - Original
draft, Writing - Review and Editing.
C. AS: Methodology, Investigation, Data Retrieval, Writing-
Original draft, Writing-Review and Editing.
D. JO: Methodology, Investigation, Data Interpretation,
Writing-Review and Editing, Project administration.
E. JM: Conceptualization, Methodology, Investigation, Data
Interpretation, Writing-Review and Editing, Project administration.
Acknowledgement
This project would not have been possible without the assistance of the Carle Foundation Hospital Outcomes Research team including Debby Vannoy, and Dr. Linda Owens.
References
- Martin JA, Hamilton BE, Osterman MJK, Driscoll AK (2021) Births: Final data for 2019. Natl Vital Stat Rep 70(2):1-51.
- Pfuntner A, Wier LM, Stocks C (2006) Most frequent procedures performed in U.S. Hospitals, 2010. In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US).
- Caughey AB, Wood SL, Macones GA, Wrench IJ, Huang J, et al. (2018) Guidelines for intraoperative care in cesarean delivery: Enhanced recovery after surgery society recommendations (Part 2). Am J Obstet Gynecol 219(6): 533-544.
- Spain J, Tuuli M, Stout M, Roehl K, Odibo A, et al. (2014) Time from uterine incision to delivery and hypoxic neonatal outcomes. Am J Perinatol 32(5): 497-502.
- Mohamad MI El-Bokl, Doaa Sh Abo Zaher, Abd El-Rahman A Abd El-Razek, Mona M Sediek Khalil, Heba M Marie (2018) The correlation between the duration of fetal extraction during cesarean section and development of transient tachypnea of the newborn. Med J Cairo Univ 86: 611-615.
- Maayan Metzger A, Schushan Eisen I, Todris L, Etchin A, Kuint J (2010) The effect of time intervals on neonatal outcome in elective cesarean delivery at term under regional anesthesia. Int J Gynecol Obstet 111(3): 224-228.
- Andersen H, Auster G, Marx G, Merkatz I (1987) Neonatal status in relation to incision intervals, obstetric factors, and anesthesia at cesarean delivery. Am J Perinatol 4(4): 279-283.
- Peacock JL, Marston L, Marlow N, Calvert SA, Greenough A (2012) Neonatal and infant outcome in boys and girls born very prematurely. Pediatr Res 71(3): 305-310.
- Ramachandrappa A, Jain L (2008) Elective cesarean section: Its impact on neonatal respiratory outcome. Clin Perinatol 35(2): 373-393.
- World Health Organization (2012) Born too soon: The global action report on preterm birth, p. 112.
- Luthra G, Gawade P, Starikov R, Markenson G (2013) Uterine incision-to-delivery interval and perinatal outcomes in transverse versus vertical incisions in preterm cesarean deliveries. J Matern Fetal Neonatal Med 26(18): 1788-1791.
© 2024 Aksal Vashi BS. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






