- Submissions

Full Text
Associative Journal of Health Sciences
COVID-19 Reinfection without Vaccination Vs. with Vaccine: They are not Differentiated by Biological Factors, but by Psycho-Social Variables
Jose Luis Turabian*
Specialist in Family and Community Medicine, Health Center Santa Maria de Benquerencia, Regional Health Service of Castilla la Mancha (SESCAM), Toledo, Spain
*Corresponding author: Jose Luis Turabian, Specialist in Family and Community Medicine, Health Center Santa Maria de Benquerencia Toledo, Spain
Submission: August 25, 2022;Published: September 23, 2022

ISSN:2690-9707 Volume2 Issue1
Abstract
Background: The clinical-epidemiological differences and their importance regarding public health
between cases of COVID-19 reinfection without vaccination and cases of COVID-19 reinfection with 1, 2
or 3 doses of vaccine are not known.
Objectives: To compare the clinical-epidemiological characteristics of the cases of COVID-19 reinfection
without vaccination with the cases of COVID-19 reinfection with 1, 2 or 3 doses of vaccine, to assess
whether there are differences in health utility applicable to clinical work in general medicine.
Methodology: An observational, longitudinal and prospective study of COVID-19 re-infections was
conducted from March 1, 2020, to July 1, 2022, in a general medicine office in Toledo, Spain.
Result: Eight cases of COVID-19 reinfection without vaccination and 35 with vaccine (1, 2 or 3 doses)
were included. 2 cases presented 2 reinfections: 2 women aged 17 and 19, with 2 and 1 dose of the
vaccine, respectively. The unvaccinated COVID-19 reinfection cases were younger, male, of a lower socialoccupancy
class, and with more complex problems in the family context. There were no statistically
significant differences between the cases of COVID-19 reinfection without vaccination and those
vaccinated (1, 2 or 3 doses) by presence of health care workers, low-income household, ethnic minority,
severity of primary infection symptoms, chronic diseases, days from primary infection (or first reinfection)
to reinfection (or second re-infection), or year of reinfection (2020, 2021 or 2022).
Conclusion: The cases of COVID-19 reinfection without vaccination vs. cases of COVID-19 reinfection
with vaccine (1, 2 or 3 doses) are not differentiated by biological factors, but by psychosocial variables,
which probably associate other health behaviors with not being vaccinated against COVID-19
Keywords: COVID-19; SARS-CoV-2; Reinfections; COVID-19 vaccine; General practice; Public healthBile Duct, IHBC: Intrahepatic Biliary Channel; MRCP: Magnetic Resonance Cholangiopancreatography
Introduction
Currently, it is predicted that it will be normal to be infected with the severe acute respiratory syndrome coronavirus (SARS-CoV-2) several times throughout life; In other words, the behavior of SARS-CoV-2 will resemble that of the rest of the coronaviruses that coexist with humans [1-4]. A SARS-CoV-2 reinfection occurs when a person with COVID-19 recovers and gets SARS-CoV-2 again, although after having presented COVID-19, most individuals will have some degree of protection [5].
The SARS-CoV-2 infection control strategy, and in particular its vaccination, is at a
crossroads. The following keys can be highlighted:
1. Currently high incidence of symptomatic infection, generally mild, including people
with a complete vaccination schedule and those who have had
previous infections (re-infections).
2. Vaccine effectiveness against infection and symptomatic
disease waning over time (humoral immunity). It is important
to note that the three-dose vaccine regimen maintains a very
notable protection against severe disease and death even with
circulating omicron variants (protection based on cellular
immunity).
3. Permanent and rapid evolution of the virus. Recently the
subvariants of omicron BA.4 and BA.5 are the predominant
ones (and new ones are already on the horizon), and they
seem to show a very high transmissibility and greater ability to
escape from natural immunity due to previous infections and
from the vaccine. So, the evolution of the virus is uncertain and
unpredictable [6-9].
Historically, vaccination has been one of the safest and most cost-effective public health interventions available. As of January 2022, 60.5% of the world’s population has received at least one dose of a COVID-19 vaccine. Vaccination rates continue to lag in low-income countries, where only 10% of the population have received at least one dose of a vaccine, while in high- and uppermiddle- income countries, 77% of the population have received at least one dose of a vaccine [10].
On the other hand, it is worrying that numerous reports suggest that people’s willingness to be vaccinated against COVID-19 is far from universal. There is significant variation in vaccine acceptance, due to a variety of individual and vaccine-related factors. Varying rates of vaccine hesitancy have been reported in different countries: 26% in Europe, 11% in Japan, 35% in the United States, 8-35% in China, and 20% in low- and middle-income countries from Asia, Africa and South America [11]. Consequently, the factors associated with vaccination against covid-19 continue to be the subject of a variety of investigations around the world [10].
In this context, reinfections are increasingly common and will continue with the emergence of new variants that escape previous vaccination. Data are lacking to identify how these reinfections occur, who is most at risk, and the severity of reinfection episodes [5]. In this way, numerous questions are raised; one of them is what the differences between the clinical-epidemiological characteristics of the cases of COVID-19 reinfection without vaccination versus the cases of COVID-19 reinfection with are 1, 2 or 3 doses of vaccine, to assess whether there are differences which could be applicable to clinical work in general medicine.
Material and Methods
Design and emplacement
An observational, longitudinal and prospective study of COVID-19 re-infections was conducted from March 1, 2020 to July 1, 2022 in a general medicine office in the Santa Maria de Benquerencia Health Center, Toledo, Spain, which has a list of 2,000 patients >14 years of age (in Spain, the general practitioners [GPs] care for people > 14 years of age, except for exceptions requested by the child’s family and accepted by the GP). The dependent neighbourhood of the health centre has a population of 20,000 inhabitants. The GPs in Spain work within the National Health System, which is public in nature, and are the gateway for all patients to the system, and each person is assigned a GP [12]. The descriptive results of the COVID-19 reinfections case series which are presented here, as well as the incidence and risk factors from the same case series, have already been published [13,14].
Outcome of interest
To compare the clinical-epidemiological characteristics of the cases of COVID-19 reinfection without vaccination with the cases of COVID-19 reinfection with 1, 2 or 3 doses of vaccine, to assess whether there are differences of utility applicable to clinical work in general medicine.
Definition of reinfection
SARS-CoV-2 reinfection was conventionally defined as a documented infection occurring at least 90 days after a previous infection, to avoid misclassification of prolonged PCR positivity as reinfection if a shorter time interval is used [15-17].
Diagnosis of COVID-19 and definition of doses of vaccine
The diagnostic criteria for COVID-19, the definitions of vaccination with 1, 2 or 3 doses (booster) have been previously published for this study [13,14].
Collected variables
A. Age and sex
B. Symptoms of COVID-19 in reinfection
C. Chronic diseases (defined as “any alteration or
deviation from normal that has one or more of the following
characteristics: is permanent, leaves residual impairment, is
caused by a non-reversible pathological alteration, requires
special training of the patient for rehabilitation, and / or can
be expected to require a long period of control, observation
or treatment” [18], classified according to the International
Statistical Classification of Diseases and Health-Related
Problems, ICD-10 Version: 2019 [19]
D. Patients with the presence of at least one chronic disease
E. Dates of COVID-19 infections and days from COVID-19
primary infection to COVID-19 reinfection
F. Social-occupancy class (according to the Registrar
General’s classification of occupations and social status code:
professional occupations, intermediate occupations, nonmanual
skilled occupations, manual skilled occupations, partly
skilled occupations, unskilled occupations, other -students,
armed forces, and people whose occupation is inadequately
described) [20,21].
G. If they were Health Care Workers
H. Problems in the family context and low-income household
based on the genogram and in the experience of the GP for their
continuity of care and knowledge of the family (genogram is a
schematic model of the structure and processes of a family, which
included the family structure, life cycle and family relational
patterns). It was understood that “complex” genograms present
families with psychosocial problems. In this way, “problems
in the family context” was defined as families with “complex
genogram”. The definition of “low-income household” was
based on the opinion of the family doctor who performed the
genogram at the past time, and who has remained in the same
practice for over 30 years [22-25].
I. Ethnic minority, defined as a “human group with cultural,
linguistic, racial values and geographical origin, numerically
inferior compared to the majority group” [26].
J. Severity of the disease -primary infection and reinfection
(mild cases: clinical symptoms are mild and no manifestation
of pneumonia can be found on images; moderate cases: with
symptoms such as fever and respiratory tract symptoms, and
the manifestation of pneumonia can be seen on the imaging
tests; and severe cases: respiratory distress, respiratory
rate ≥30 breaths/min; pulse oxygen saturation ≤93% with
room air at rest; arterial partial pressure of oxygen/oxygen
concentration ≤300mmHg) [27]. To simplify comparison,
moderate and severe cases were counted together.
K. Vaccinated with 1 dose, with 2 doses, with booster, and
not vaccinated against COVID-19
Statistic analysis
The bivariate comparisons were performed using the Chi Square test (X2), X2 with Yates correction or Fisher Exact Test, and the student test for the mean.
Ethical aspects
Individual patient data is not used, but only aggregated statistical data.
Result
Table 1: Variables in COVID-19 reinfection without vaccination versus with vaccine (1, 2 or 3 doses).( ): Denotes percentages; NS: Not significant.
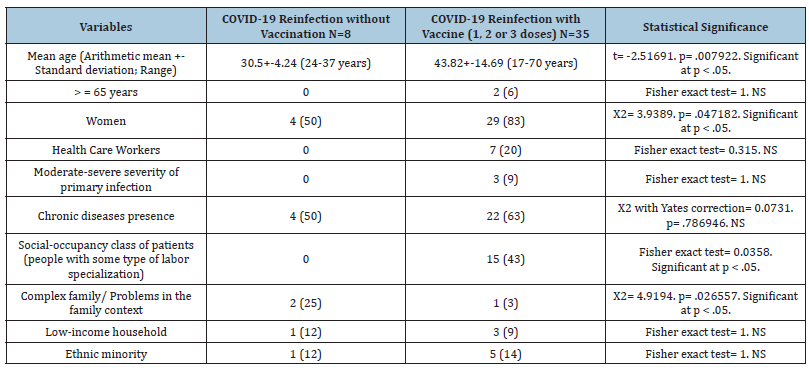
Table 2:Variables in COVID-19 reinfection without vaccination versus with vaccine (1, 2 or 3 doses). ( ): Denotes percentages; NS: Not significant; *COVID-19 reinfection with vaccine (1, 2, or 3 doses) N=35 people; 2 cases presented 2 reinfections: 2 women aged 17 and 19, with 2 and 1 dose of the vaccine, respectively. The number of infections is used as denominator: N=37.
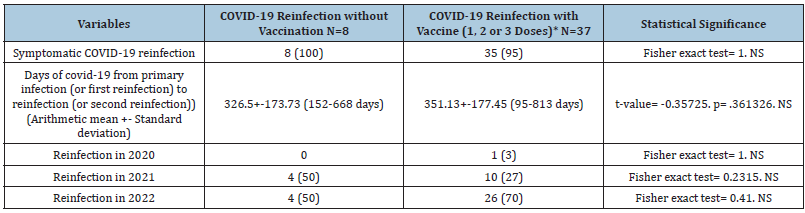
Table 3:Chronic diseases in COVID-19 reinfection without vaccination versus with vaccine (1, 2 or 3 doses). ( ): Denotes percentages; NS: Not significant; *Patients could have more than one chronic disease. The percentages of chronic diseases are over the total of chronic diseases of symptomatic and asymptomatic patients.
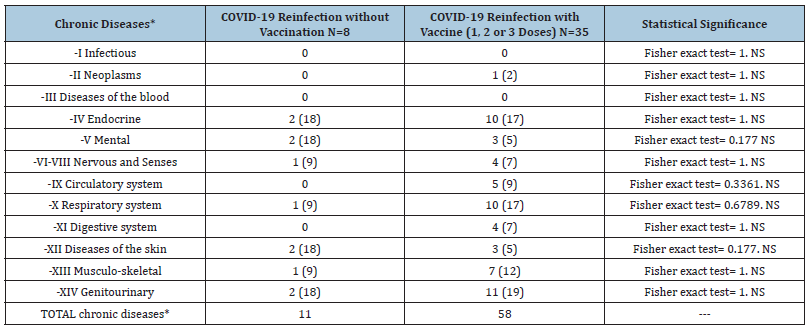
Table 4:Symptoms COVID-19 reinfection cases without vaccination versus with vaccine (1, 2 or 3 doses). ( ): Denotes percentages; NS: Not significant; *Patients could have more than one symptom. The percentages are over the total of symptoms; ***COVID-19 reinfection with vaccine (1, 2, or 3 doses) N=35 people; 2 cases presented 2 reinfections: 2 women aged 17 and 19, with 2 and 1 dose of the vaccine, respectively. The number of infections is used as denominator: N=37.
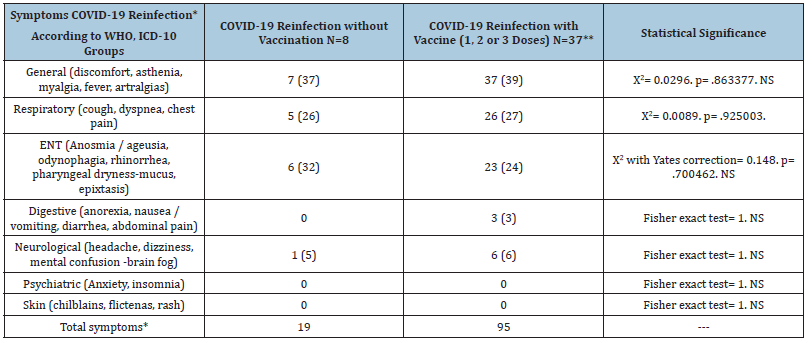
Eight cases of COVID-19 reinfection without vaccination and 35 with vaccine (1, 2 or 3 doses) were included. 2 cases presented 2 reinfections: 2 women aged 17 and 19 with 2 and 1 dose of the vaccine, respectively. The unvaccinated COVID-19 reinfection cases were younger, male, of a lower social-occupancy class and with more complex problems in the family context. There were no statistically significant differences between the cases of COVID-19 reinfection without vaccination and those vaccinated (1, 2 or 3 doses) due to the presence of health care workers, low-income household, ethnic minority, severity of primary infection symptoms, chronic diseases, days from primary infection (or first re-infection) to reinfection (or second re-infection), or year of reinfection (2020, 2021 or 2022) (Table 1-4).
Discussion
Main findings
The main results of our study are that the cases of COVID-19 reinfection without vaccination were younger, male, of a lower social-occupancy class, and with more complex problems in the family context. On the other hand, there were no statistically significant differences between the cases of COVID-19 reinfection without vaccination and those vaccinated (1, 2 or 3 doses) due to the presence of low-income household, ethnic minority, severity of primary infection symptoms or chronic diseases. Taking into account that the three-dose vaccine regimen maintains a very remarkable protection against severe disease and death even with circulating omicron variants, these data may allow planning strategies to improve the vaccination rate [1-4].
Comparison with other studies
Immunity: SARS-CoV-2 infection offer a high level of sustained protection against reinfection, comparable to that offered by vaccines, but decrease with the introduction of new major variants of the virus; dramatically when Omicron appear. Decreases in protection against reinfection appeared to be primarily driven by viral evolution [28]. Vaccine-induced immunity after a primary vaccination series is modest against Omicron infection in the months following vaccination and declines significantly over time. Most studies have found that the protection conferred by hybrid immunity against infection and mild symptomatic disease is similar to or slightly better than immunity induced by infection or vaccine alone [29]. Therefore, previous infection or vaccination guarantees a certain degree of protection against SARS-CoV-2 reinfections. However, emerging variants could reinfect naturally to infected or vaccinated individuals [30].
Vaccine hesitancy: Vaccine hesitancy is not a clear issue, but rather represents a spectrum of beliefs and concerns [31]. Existing research reports that factors influencing COVID-19 vaccine acceptance may include gender, background knowledge, perceived risk of COVID-19, vaccine knowledge, vaccine confidence, etc., and vary between different populations [11]. The following factors were significantly associated with the decision to accept the COVID-19 vaccination (and to vaccinate their children): level of education, employment status, presence of chronic diseases, and consultation with a health professional from the beginning of the pandemic [10].
Socioeconomic level and family psychosocial problems: Most educated patients and those with high income levels are willing to be vaccinated [32-34]. The fact that a lower socio-economic level is associated with a lower COVID-19 vaccination rate highlights the problem of inequalities in the pandemic. Different possible pathways may include unhealthy lifestyles associated with lower socioeconomic position, such as smoking, physical inactivity, alcohol use, and cannabis use. Some of these behavioural factors have been associated with an increased risk of susceptibility to COVID-19. Low socioeconomic status can be a barrier to access health care services for COVID-19, but it does not occur in our context, where health care is universal and free, and each person is assigned a GP that is the door to the health system [12]. Family support and a herd mentality can help improve vaccination among the undecided [11]. Other family characteristics, such as living alone, without a partner or children, and being single, were negatively associated with the desire to be vaccinated [34-36]. People living alone with limited care may have less access, irregular preventive health visits, and less support from family members [37].
Sex and age: In general, greater acceptance is found among women [10]. In a study among college students who were hesitant to get vaccinated, 56% were men [11]. Patients older than 65 years are more willing to be vaccinated than younger patients [10,34], and these usually mention that “the situation is not serious enough” or that they are not at risk” [38] in order not to accept the vaccine. By against, those with chronic health conditions who perceive their health to be less than good and people who are considered at risk of contracting the disease are willing to be vaccinated [34]. Older adults, particularly those with chronic conditions, are in the most vulnerable categories for all phases of COVID-19, from contracting the virus to being at risk of severe illness or death. In addition, their vulnerability to COVID-19 is It is exacerbated in many cases by dependency on a caregiver who moves in and out of the home, thereby increasing the risk of contracting COVID-19 from the community. In short, vaccination reluctance is less or almost nil in older adults [39].
Comorbidities:No strong evidence has been found, and studies showing conflicting results, whether certain diseases (including diseases of the circulatory, digestive, nervous, respiratory, genitourinary, musculoskeletal, and connective tissue systems, metabolic diseases, and mental disorders) increase the risk of COVID-19 [36]. Like all infectious processes, the clinical severity depends on the virulence of the microorganism and the susceptibility of the host. Some people with comorbidities may be out of control or have associated complications; for example, in patients with underlying lung disease, having a new episode of COVID-19 can become a severe episode, and patients with immunocompromise can excrete the virus for weeks or months, having a persistent active infection [5].
Symptoms and severity in reinfection:Vaccines against COVID-19 help protect against severe illness, hospitalizations, and death. Additionally, COVID-19 vaccines help protect against infection. However, vaccinated people can still get COVID-19. When a vaccinated person contracts COVID-19, they are much less likely to have severe symptoms compared to people who are not vaccinated [40]. Among patients who became reinfected, hospitalization rates were similar for both vaccinated and unvaccinated patients, with approximately one in five reinfected patients admitted to hospital [41]. In a rapid systematic review of 17 cases of genetically confirmed COVID-19 reinfection, it was found that 69% of people had symptoms similar to those of their first episode, 19% had a more severe condition and 12% a milder one. The virus inoculum received the possible differences between SARS-CoV-2 variants and changes in a person’s health status can modify the symptoms of reinfection. The key point to know, and also for future vaccines, would be to resolve the role of immunological memory and whether it affects symptoms during the second infection [42,43].
Role of the GP:COVID-19 vaccines induce better long-term immunity than infection [44,45]. Regarding the action signals, one of the significant predictors that increase the intention to be vaccinated is the recommendation of the GP [10,34]. The situation is not calm enough for the vaccine boosters to be reduced. There are still vulnerable people who can develop serious forms and die from them. It should not be forgotten that current vaccines prevent hospitalization, but the duration of protection is conditioned by the level of transmission. The more infections there are, the more the virus will replicate, and the more replication there is, the more opportunities there are for mutations and, therefore, for the appearance of new variants” [46].
Study limitations:
a) Infections were not genetically sequenced; thus,
reactivations of the strain involved in the first episode cannot
be completely ruled out.
b) The number of cases was small.
c) The study may have missed asymptomatic cases who did
not attend GP consultation, as no systematic surveillance or
screening was performed.
d) Preventive behaviours associated with transmission were
not analyzed.
Conclusion
The cases of COVID-19 reinfection without vaccination vs. cases of COVID-19 reinfection with vaccine (1, 2 or 3 doses) are not differentiated by biological factors, but by psychosocial variables, which probably associate other health behaviours with not being vaccinated against COVID-19. GPs should recognize these psychosocial variables in their patients and recommend vaccination.
References
- Kojima N, Klausner JD (2021) Protective immunity after recovery from SARS-CoV-2 infection. Lancet Infect Dis 22(1):12-14.
- Goldberg Y, Mandel M, Bar On YM, Bodenheimer O, Freedman LS, et al (2022) Protection and waning of natural and hybrid immunity to SARS-CoV-2. N Engl J Med 86:2201-2212.
- Williams S (2020) Cold-causing coronaviruses don’t seem to confer lasting immunity. The Scientist.
- Johnston C, Hughes H, Lingard S, Hailey S, Healy B (2022) Immunity and infectivity in covid-19. BMJ 378: e061402.
- Pérez Cortés Villalobos A (2022) The true meaning of SARS-CoV-2 reinfections.
- Asociación Española de Pediatría (2022) Covid vaccination at a crossroads: new vaccines adapted to Ó
- Callaway E (2022) Fast-evolving COVID variants complicate vaccine updates. COVID-19 vaccines are due for an upgrade, scientists say, but emerging variants and fickle immune reactions mean it’s not clear what new jabs should look like. Nature 607: 18-19.
- Wise J (2022) Covid-19: Omicron infection is poor booster to immunity, study finds. BMJ 377: o1474.
- Wise J (2022) Covid-19: Omicron sub variants driving new wave of infections in UK. BMJ 377: o1506.
- Drouin O, Fontaine P, Arnaud Y, Montmarquette C, Prudhomme A, et al. (2022) Parental decision and intent towards COVID-19 vaccination in children with asthma: an econometric analysis. BMC Public Health 22(1): 1547.
- Xiong Y, Zhao Y, Zhang T, Wang Q, Liu JA (2022) Factors associated with the vaccination behavior among COVID-19 vaccine hesitant college students in Wuhan, China: A survey based on social psychological dimension. Front Public Health 10: 865571.
- Turabian JL (1995) Notebooks of family and community medicine. An introduction to the principles of Family Medicine. Díaz de Santos, Madrid, Spain.
- Turabian JL (2022) Characteristics of a case-series of COVID-19 reinfection and its trend from 2020 to June 2022 in a general medicine office in Toledo (Spain). Int J Epidemiol Health Sci 3: e39.
- Turabian JL (2022) Incidence rates and risk factors of covid-19 reinfections from March 1, 2020 to July 1, 2022 in a general medicine office in Toledo, Spain. Annals of Community Medicine and Primary Health Care. 1(1): 1006.
- Slezak J, Bruxvoort K, Fischer H, Broder B, Ackerson B, et al. (2021) Rate and severity of suspected SARS-Cov-2 reinfection in a cohort of PCR-positive COVID-19 patients. Clin Microbiol Infect 27(12): 1860.e7-1860.e10.
- Altarawneh HN, Chemaitelly H, Ayoub Hh, Tang P, Hasan MR, et al. (2022) Effects of previous infection and vaccination on symptomatic omicron infections. N Engl J Med 87(1): 21-34.
- Ayoub HH, Tomy M, Chemaitelly H, Altarawneh HN, Coyle P, et al. (2022) Estimating protection afforded by prior infection in preventing reinfection: applying the test-negative study. MedRxiv.
- Strauss AL (1984) Chronic illness and the quality of life. The C.V. Mosby Company, St Louis, Missouri, USA.
- WHO (2019) International statistical classification of diseases and health-related problems. ICD-10 Version: 2019, Geneva, Switzerland.
- Royal Collage of General Practitioners (1986) The classification and analysis of general practice data. Occasional Paper 26.
- Donaldson RJ, Donaldson LJ (1983) Essential community medicine. MTP Press, Lancaster, Pennsylvania, USA.
- Turabian JL (2017) Family genogram in general medicine: A soft technology that can be strong. An Update. Res Med Eng Sci 3(1). 186-191.
- Russell LT (2020) Capturing family complexity in family nursing research and practice. J Fam Nurs 26(4): 287-293.
- Watts C, Shrader E (1998) How to do (or not to do) The genogram: a new research tool to document patterns of decision-making, conflict and vulnerability within households. Health Policy Plan 13(4): 459-464.
- McIlvain H, Crabtree B, Medder J, Stange KC, Miller WL (1998) Using practice genograms to understand and describe practice configurations. Fam Med 30(7): 490-496.
- Diccionario panhispánico del español jurídico (2022) Ethnic minority.
- Mao S, Huang T, Yuan H, Li M, Huang X, et al. (2020) Epidemiological analysis of 67 local COVID-19 clusters in Sichuan Province, China. BMC Public Health 20(1): 1525.
- Michlmayr D, Hansen CH, Gubbels SM, Branth PV, Bager P, et al. (2022) Observed protection against SARS-CoV-2 reinfection following a primary infection: A Danish cohort study among unvaccinated using two years of nationwide PCR-test data. Lancet Regional Health 20: 100452.
- WHO (2022) Interim statement on hybrid immunity and increasing population seroprevalence rates.
- Rahman S, Rahman MM, Miah M, Begum MN, Sarmin M, et al. (2022) COVID-19 reinfections among naturally infected and vaccinated individuals. Sci Rep 12(1): 1438.
- Li L, Wood CE, Kostkova P (2022) Vaccine hesitancy and behavior change theory-based social media interventions: a systematic review. Transl Behav Med 12(2): 243-272.
- Fabry P, Gagneur A, Pasquier JC (2011) Determinants of a (H1N1) vaccination: cross-sectional study in a population of pregnant women in Quebec. Vaccine 29(9): 1824-1829.
- Schwarzinger M, Flicoteaux R, Cortarenoda S, Obadia Y, Moatti JP (2010) Low acceptability of a/H1N1 pandemic vaccination in French adult population: did public health policy fuel public dissonance? PLoS One 5(4): e10199.
- Shmueli L (2021) Predicting intention to receive COVID-19 vaccine among the general population using the health belief model and the theory of planned behavior model. BMC Public Health 21: 804.
- Rosoff DB, Yoo J, Lohoff FW (2021) Smoking is significantly associated with increased risk of COVID-19 and other respiratory infections. Commun Biol 4(1): 1230.
- Luo S, Liang Y, Wong THT, Schooling CM, Yeung SLA (2022) Identifying factors contributing to increased susceptibility to COVID-19 risk: a systematic review of Mendelian randomization studies. Int J Epidemiol 51(4): 1088-1105.
- Nagata JM, Hernández Ramos I, Kurup AS, Albrecht D, Vivas Torrealba C, et al. (2013) Social determinants of health and seasonal influenza vaccination in adults ≥65 years: a systematic review of qualitative and quantitative data. BMC Public Health 13: 388.
- Seale H, Heywood AE, McLaws ML, Ward KF, Lowbridge CP, et al. (2010) Why do I need it? I am not at risk! Public perceptions towards the pandemic (H1N1) 2009 vaccine. BMC Infect Dis 10: 99.
- Wyte Lake T, Levy C, Hovsepian S, Mudoh Y, Schmitz C, et al. (2022) COVID-19 vaccine adoption and hesitancy among older Veterans. BMC Public Health 22: 1532.
- CDC (2022) COVID-19 after vaccination: Possible breakthrough infection. Content source: National Center for Immunization and Respiratory Diseases (NCIRD), Division of Viral Diseases.
- Rohrer Meck K, Barkley E, Lin L, Fox B, McNitt J (2021) Getting COVID-19 twice: Reinfections 44% more likely among the unvaccinated. Abstract: Unvaccinated patients are more likely than vaccinated patients to get COVID-19 twice. Cosmos Study. Epic Research.
- Ledford H (2020) Coronavirus reinfections: three questions scientists are asking Second infections raise questions about long-term immunity to COVID-19 and the prospects for a vaccine. Nature 585(7824): 168-169.
- Wang J, Kaperak C, Sato T, Sakuraba A (2021) COVID-19 reinfection: a rapid systematic review of case reports and case series. J Investig Med 69(6): 1253-1255.
- Zieba J (2022) COVID-19 vaccines induce better long-term immunity than infection. The Scientist.
- Zhang Z, Mateus J, Coelho CH, Dan JM, Rydyznski C, et al. (2022) Humoral and cellular immune memory to four COVID-19 vaccines. Cell 185(14): 2434-2451.
- Loewy MA (2022) COVID-19: the week summary. Medscape.
© 2022 Jose Luis Turabian. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






