- Submissions

Full Text
Associative Journal of Health Sciences
Hyperbilirubinemia 73mg/Dl After Acute Suppurative Cholangitis is Not Always Fatal, a Case Report
AyaMohamed Mahros*
Gastroenterology & Infectious Diseases Department, Egypt
*Corresponding author: AyaMohamed Mahros, Hepatology, Gastroenterology & Infectious Diseases Department, Faculty of Medicine, Kafrelshiekh University, Egypt
Submission: April 23, 2021;Published: December 20, 2021

ISSN:2690-9707 Volume1 Issue5
Abstract
Background: Obstructive jaundice is a common health problem with various complications including
liver dysfunction as well as systemic complications. Proper treatment of the underlying etiology should be
the primary goal in management. However, different therapeutic approaches have been tried in lowering
the bilirubin serum levels when treatment of the underlying cause is not feasible or unsatisfactory.
These approaches include extracorporeal liver support (e.g., Molecular Adsorbent Recirculating System
(MARS), plasma exchange, and charcoal. To the best of our knowledge, this is the first case of marked
hyperbilirubinemia that was successfully managed with combined ERCP and plasma ultrafiltration.
Case presentation: We describe a case of marked hyperbilirubinemia (73mg\dl) following cholelithiasis
and acute suppurative cholangitis that was successfully treated by combined plasma ultrafiltration and
internal drainage through ERCP and biliary stenting.
Conclusion: The collaborative teamwork between gastroenterologist, endoscopist and nephrologist
thorough the combined biliary drainage with ERCP and ultrafiltration could save the life of a patient with
marked hyperbilirubinemia.
Keywords: Hyperbilirubinemia; Plasmapheresis; Cholangitis; Mortality
Abbreviations: ERCP: Endoscopic Retrograde Cholangiopancreatography; MARS: Molecular Adsorpant Recirculating System; CBD: Common Bile Duct, IHBC: Intrahepatic Biliary Channel; MRCP: Magnetic Resonance Cholangiopancreatography
Background
Obstructive jaundice is a common problem with different etiologies. It does occur due to
interference with bile flow from the liver down to the duodenal papilla [1]. The hazards of
obstructive jaundice include liver dysfunction as well as systemic complications. Disruption of
the intestinal mucosal barrier as a consequence of the decrease of bile in the gut results in an
increased absorption of endotoxins and inflammatory cytokines (TNF-α, IL-6) production. As
a result, systemic inflammatory response syndrome occurs which may lead to multiple organ
dysfunction syndrome. Fatal complications could occur such as hemodynamic instability and
acute renal failure, cardiovascular suppression, immune compromise, coagulation disorders
[2], so urgent and effective management is mandatory to avoid further organ damage,
especially permanent liver damage [3].
Proper treatment of the underlying condition should be the primary goal in the
management [4]. However, different therapeutic approaches have been tried in lowering
the bilirubin serum levels when treatment of the underlying cause is not feasible or
unsatisfactory. These approaches include extracorporeal liver support (e.g., Molecular
Adsorbent Recirculating System (MARS) [5], plasma exchange, and charcoal hemoperfusion
[1,6]. Plasma exchange is a safe and effective method for the clearance of bilirubin and has been tried in many cases with acceptable success rates [7,8]. Acute
suppurative cholangitis, conveys sepsis in the biliary system and
is associated with a wide range of morbidity and mortality mainly
in the elderly and high-risk populations. The disease clinically
is characterized by fever (and chills), jaundice, pain, and even
shock [9]. In most of the cases it follows obstructive jaundice of
any etiology, although it is one of the documented adverse events
of ERCP and seldom occurs without obstruction or interventions
[10]. We describe a case of marked hyperbilirubinemia (73mg\dl)
following cholelithiasis acute suppurative cholangtitis successfully
treated by combined plasma ultrafiltration and internal drainage
through ERCP and biliary stenting.
Case Presentation
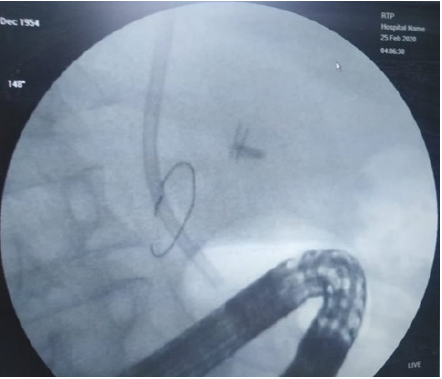
A 42-year-old heavy smoker male patient known to have liver cirrhosis for four years presented to our outpatient clinic at Kafrelsheikh University Hospital with one month right upper quadrant pain; colicky, radiate to the right shoulder, associated with fever and jaundice. The condition was associated with clay stool and dark urine. On examination, the patient was very toxic, with deep jaundice and splenomegaly but without ascites. Laboratory evaluation revealed: total bilirubin 55mg\dL, direct bilirubin: 39mg\dL, S. creatinine: 3mg\dL. Ultrasound examination revealed Intrahepatic Biliary Channel Dilatation (IHBC), dilated Common Bile Duct (CBD): 16mm with multiple stones inside. ERCP was done with pus drainage and multiple stone extraction and plastic stent insertion; cholangitis was diagnosed. The patient was discharged on demand against medical advice, refused to stay at hospital and did not receive the prescribed antibiotics. Ten days later, the patient came back with sever right hypochondrial pain, deep jaundice, fever, and toxemia. Total bilirubin was 73mg\dL and direct bilirubin: 60mg\dL. Serum creatinine was 5mg\dl. Abdominal US revealed no IHBC dilatation. MRCP revealed distal CBD stricture and residual stones. Two sessions of plasmapheresis were done as a trial to reduce the markedly elevated bilirubin. As regard plasmapheresis was done by membrane plasmapheresis using a plasma flux filter P1 with about around 2400ml plasma volume exchanged during the session. The hemodialysis machine used for plasmapheresis was Fresenius 4008s hemodialysis machine. Two days after the second session, total bilirubin was:37mg\dL, Direct bilirubin: 29mg\dL. Follow up abdominal ultrasound showed nonfunctioning stent, ERCP was done with removal of the old upward migrated occluded plastic stent (Figure 1) and insertion of a new plastic stent 10F\10cm. The patient was kept on antibiotics and follow up; and 3 days after the second ERCP, total bilirubin dropped to 15mg\dL and 10mg\dL direct bilirubin. Follow up the patient after 1 months revealed a functioning stent with total bilirubin 2mg\dL. Three months later the serum bilirubin was 1.2mg/dl.
Figure 1: Upwards migrated stent noticed in ERCP.
Discussion
Our case developed progressive post ERCP cholestasis
mostly due to inadequate antibiotic treatment of the underlying
cholangitis due to premature discharge of the patient from the
hospital without receiving the antibiotics. Renal impairment
subsequently developed, and this markedly worsened the general
condition of the patient and threatened his life. The patient was
managed with plasma ultrafiltration followed by drop of the
total bilirubin. Unfortunately, obstruction of the stent occurred
and ERCP was done with stone extraction, extraction of occluded
upward migrated stent . Follow up serum bilirubin was done for 3
months till it came to normal. The presented case here had some
interesting clinical aspects. First, the patient presented by one month history of improperly treated cholangitis. We do not have
enough data about this one-month history of illness, but we expect
that the underlying chronic liver disease, that is quiet high in our
community, directed physicians treating him to thought in hepatic
decompensation. Consequently, we alarm all physicians treating
patients with chronic liver disease to exclude other diagnoses to
avoid further delays in proper management. Second, the patient
admitted to our hospital with very high serum bilirubin (53mg\
dl) due to suppurative cholangitis and this was obvious with the
pus flowing from the CBD at time of sphinectrotomy. In fact, we
achieved internal drainage, but the patient insists on discharge
and ignored antibiotic therapy. This point of extreme importance
because suppurative cholangitis in patients with chronic liver
disease would result in high morbidity and mortality and this had
been reported in many publications and consequently clinicians
treating patients with acute suppurative cholangitis should begin
aggressive antibiotic therapy as early as possible.
Third, the exceptionally high level of bilirubin (73mg\dl)
reported in this patient in the second admission. In fact, we searched
the literature, and we did not find similarly high level. However, a
case report by Khurram et al., reported marked elevation of direct
bilirubin to the level of (17mg/dl)due to ceftriaxone use. Whereas
Guimarães and Silva described a case of marked hyperbilirubinemia
not responding to plasmapheresis due to sickle cell anemia with
reported serum bilirubin level of 53mg/dl. Fourth, it seems also
that this high bilirubin level affected the renal function with high
creatinine level. Although broad spectrum antibiotic therapy was
initiated, the general condition did not improve. At that time,
we sought adviceof our nephrology team. They performed two
sessions of plasma ultrafiltration and consequently serum bilirubin
dropped to 37mg\dl. It was reported in the literature that different
methods of dialysis may benefit patients with hyperbilirubinemia.
The majority of cases were presented with acute liver cell failure
treated with MARS. In fact, plasmapheresis or ultrafiltration was
tried in treatment of severe hyperbilirubinemia in the centers
lacking the facility of artificial and bioartificial liver support. Tried
plasma ultrafiltration to treat patients with high serum bilirubin
awaiting liver transplantation and also it was tried in patients
with cholestasis with variable rates of success. To the best of our
knowledge, this is the first case of ultrafiltration in managing acute
suppurative cholangitis with this exceptionally high level of serum
bilirubin.
We believe that plasmapheresis is not the ideal treatment for
this patient with jaundice due to cholangitis. However, jaundice
was progressively increasing with impending renal failure. Also,
sufficient biliary drainage was not achieved due to the presence of
biliary stricture and stent migration. We were worrisome about a
multi-organ failure cascade with renal shutdown, so we thought out
of box to control the condition by reducing bilirubin load through
plasmapheresis that could strives for the opportunity to cure and
this was supported by evidence from literature. Plasmapheresis is
a safe effective treatment that may improve the survival in cases
with hyperbilirubinemia due to different disorders. Another study
from china demonstrated that plasma exchange is an effective
method in lowering high levels of bilirubin with fewer side effects.
Fifth, the collaborative teamwork. We assume that this patient
would have been lost if not managed by the teamwork between
gastroenterologist, endoscopist and nephrologist. Unfortunately,
in communities lacking this collaborative health care system,
patients like our patient would be lost. Our hospital support this
team activity, and this reflected on the good outcome we obtained.
This case reflect that marked hyperbilirubinemia is not always fatal
with proper management. Sixth, the importance of follow up. Over
a 3 months period this critically ill patient was recovered. However,
we encourage not only our juniors but also our patients not to be
depressed and insist on good outcome provided that proper team
management is applied. Conclusion: The collaborative teamwork
between gastroenterologist, endoscopist and nephrologist thorough
the combined biliary drainage with ERCP and ultrafiltration could
save the life of a patient with marked hyperbilirubinemia.
Declarations
A. Ethics approval and consent to participatewas done
B. Consent for publication written informed consent was
taken from the patient
C. Availability of all data and material of the patient: Data
sharing is not applicable to this article as no datasets were
generated or analysed during the current study.
D. Competing interest: the authors declare that they have no
competing interest.
References
- Modha K (2015) Clinical approach to patients with obstructive jaundice. Tech VascIntervRadiol 18(4): 197-200.
- Pavlidis ET, Pavlidis TE (2018) Pathophysiological consequences of obstructive jaundice and perioperative management. Hepatobiliary Pancreat Dis Int 17(1): 17‐21.
- Guicciardi ME, Gores GJ (2002) Bile acid-mediated hepatocyte apoptosis and cholestatic liver disease. Dig Liver Dis. 2002;34(6):387‐392.
- Nesseler N, Launey Y, Aninat C, Morel F, Mallédant Y, et al. (2012) Clinical review: The liver in sepsis. Crit Care 16(5): 235.
- Doria C, Mandalá L, Smith J, Claudio H, Augusto L, et al. (2003) Effect of molecular adsorbent recirculating system in hepatitis C virus-related intractable pruritus. Liver Transpl 9(4): 437‐443.
- Kaaja RJ, Kontula KK, Räihä A, Laatikainen T (1994) Treatment of cholestasis of pregnancy with peroral activated charcoal. A preliminary study. Scand J Gastroenterol 29(2): 178‐181.
- Hatice T, SerdalKorkmaz, Mehmet S, Ozlem Y, Abdulkerim Y, et al. (2019) The role of plasma exchange in hyperbilirubinemia from a different perspective. Cumhuriyet Medical Journal 41(1): 82-87.
- Yao J, Li S, Zhou L, Lei L, Lili Y, et al. (2019) Therapeutic effect of double plasma molecular adsorption system and sequential half-dose plasma exchange in patients with HBV-related acute-on-chronic liver failure. J ClinApher 34(4): 392–398.
- Qureshi WA (2006) Approach to the patient who has suspected acute bacterial cholangitis. GastroenterolClin North Am 35(2): 409‐423
- Chen M, Wang L, Wang Y (2018) Risk factor analysis of post-ERCP cholangitis: A single-center experience. Hepatobiliary Pancreat Dis Int 17(1): 55‐58.
© 2021 AyaMohamed Mahros. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






