- Submissions

Full Text
Associative Journal of Health Sciences
COVID-19 and Cardiovascular Disease: A Worksite Intervention
Tina M Penhollow* and Brittany Kimmons
Department of Exercise Science and Health Promotion, College of Science, Florida Atlantic University, USA
*Corresponding author: Tina M Penhollow, Associate Professor, Florida Atlantic University, College of Science, Department of Exercise Science and Health Promotion, 777 Glades Road, FH11-25B, Boca Raton, Florida, USA
Submission: February 24, 2021;Published: March 11, 2021

ISSN:2690-9707 Volume1 Issue4
Abstract
The Coronavirus Disease 2019 (COVID-19) pandemic has resulted in social and working environments that have significantly changed. This has included mandatory international lockdowns, quarantine regulations, social distancing policies, suspention of productive work activity, loss of income, anxiety, and the fear of future employment. This lockdown has also exacerbated a number of health aliments, including weight gain and high blood presuure, which can lead to Cardiovascular Disease (CVD). A number of workplace interventions can help to allieviate the stress and uncertainty of this pandemic. This includes policies of anti-contagion measures, requiring and providing health care workers with personal protective equipment, and the implemenation of health promotion programs to enhance quality of life for employees. The Health Belief Model (HBM) and the Transtheoretical Model (TTM) are theortetical frameworks that can assist to deliver work-related health promotion programs. This mini review is an intervention proposal in order to provide approaches to better understand and provide assistance relative to the health and well-being of worksite employees.
Keywords: COVID-19; Cardiovascular disease; Worksite health promotion programs
Introduction
The COVID-19 pandemic has significantly transformed both social and working
environments. This has ranged from social distancing polies, restricted lockdowns, isolation
periods, quarantine, loss of income, interruption of productive activity, and an overall fear of
future employment. Characteristics of any workplace can play a vital role in an employee’s
metal and physical health status [1]. A high percentage of workplace employees are overweight
or obese and are treated for type 2 diabetes, hypertension, anxiety, stress, and depression
[2,3]. These issues increase the chance of developing Cardiovascular Disease (CVD). Recent
studies support an above-average annual weight gain due to COVID-19 restrictions [4].
Individuals who work for companies are often lacking a healthy culture which may directly
impact employee health and mental well-being [5,6]. Administrative and executive employees
are often unaware of how an unhealthy work environment affects overall productivity and
employee satisfaction. Little seems to be done in many work-place facilities to address the
unhealthy social norms this environment can create. Often onsite cafes cater to unhealthy food
options, employee recognition rewards include candy and junk food, there is limited focus on
stress management, and most employees have a sedimentary job with few opportunities to
move around.
A workplace initiative aimed to target at-risk employees for COVID-19 and Cardiovascular
Disease (CVD) is an important initiative. Current recommendations from the Centers of
Disease Control and Prevention (CDC) for both COVID-19 and CVD focus on controllable risk
factors. Recommendations include wearing a mask in public and while at work, practicing
healthy hygiene, 30 minutes of physical activity five days a week, a healthy diet consisting
of lean proteins, fruits, and vegetables, limiting high fat and sugar intake, not smoking,
initiative alcohol consumption, and managing levels of stress [3]. This can lead to employees
living a healthier life, lower the risk of COVID-19 and CVD, and increase longevity to live a
healthier life. This evolution will directly influence the culture, change current social norms,
and increase employee engagement in health initiatives. This can decrease insurance costs
for both employees and the company. This paper is a proposed intervention that applies
the Health Behavior Model (HBM) and the Transtheoretical Model (TTM) to address how
a worksite intervention can help minimize the severity of COVID-19 symptoms and reduce Cardiovascular Disease (CVD) while creating a healthy work
environment.
Intervention Theories
Health Belief Model (HBM)
The HBM focuses on the likelihood of an individual participating in preventative screenings or actions for healthier behaviors. Employees’ attitudes toward the program’s effectiveness and the disease/illness’s threat will determine participation probability. This theory allows focus on an employee’s attitudes toward the implications of COVID-19 and CVD and how it influences their motivation to adopt healthier behaviors. This model accounts for an individual’s expectation of the initiative’s benefits and barriers to determine their desire to participate. The HBM consists of six constructs that support people’s desire to act or not in preventative or maintenance health initiatives. Please see Table 1.
Table 1:
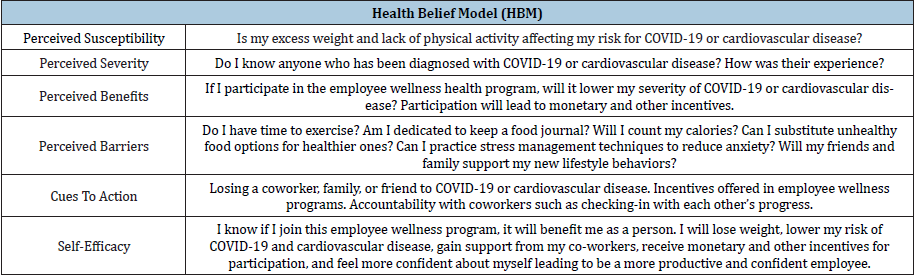
Perceived susceptibility: This construct is an individual’s
belief that they may contract a disease or illness. Focusing on
COVID-19 and CV disease will allow us to reach more employees
with one initiative. For example, suffering a recent heart attack
experienced by a current employee will increase the awareness of
the detriments of type 2 diabetes, high blood pressure, and obesity
in a workplace.
Perceived severity: This construct consists of how serious
one feels about contracting an illness and its effects. According to
recent research by Brocq et al. [7], obese individuals exhibit fear
and anxiety of obesity-related COVID-19 complications, and they
were worried about limited access to medical assistance.
Perceived benefits: Benefits of participation in an employee
wellness program are multifold. Employees can save money on
medical costs, be able to use paid time off for vacation versus sick
time and will feel better both mentally and physically. Incentives
provided throughout a program can enhance participation.
Perceived barriers: Barriers to any program can cause a
program to fail. If employees view the program to be physically or
emotionally inconvenient, participation lacks. Some barriers can be
resolved before the program exists. Barriers include time, money,
social support, and lack of self-efficacy.
Cues to action: An example of cues to action is having a
coworker suffer a heart attack in a tight-knit organization. This
could be a wake-up call to employees as a catalyst for change. Atrisk
employees are concerned for their well-being. Those not at risk
often know other employees who are at risk.
Self-efficacy: Self-efficacy is the belief that one is confident
enough to accomplish tasks provided to be successful. Participants
will see the effects of their efforts. Typically, people want to avoid
illness and are confident that a specific health behavior will prevent
disease.
Transtheoretical Model (TTM)
The TTM addresses change as a process that happens over time, based on a person’s decision-making. People can start at any stage, depending on their attitudes and beliefs at the program’s introduction. Each stage is unique in its intervention strategies to motivate people to change and move to the next step. The goal is to adopt to change and reach a level of maintenance. The TTM consists of six stages of change [8]; Table 2.
Table 2:
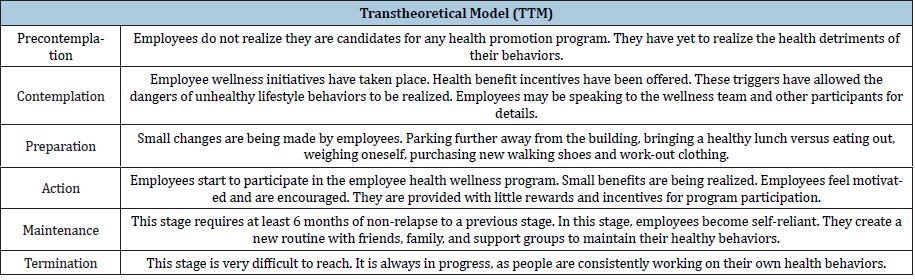
Precontemplation: This stage pertains to those who are six months or more out from making behavioral changes. These individuals do not recognize the benefits of change and focus more on the inconveniences of changing.
Contemplation: Once individuals realize the danger of their unhealthy behaviors, they consider the pros to change. These people tend to make changes in the next six months.
Preparation: This is when a person starts making small steps to change. For example, purchasing new workout clothing or buying a comfortable pair of walking shoes.
Action: People who continue to make changes for six months have reached the action stage. They experience the benefits of healthy behaviors both mentally and physically. They continue moving forward with healthy behavior changes.
Maintenance: This stage applies to those who have managed to stay on track and not relapse to a previous stage for at least six months. They feel confident in their ability to change and may remain in this stage for up to five years.
Termination: Those who have achieved self-efficacy and will not relapse have entered into the termination stage. Reaching the termination stage is not common, as individuals are always working on their own health behaviors.
Proposed Program Implementation
Combining the HBM with the TTM provides a framework
for a company to develop a wellness team using a multilevel
approach. It will include employees who are at a variety of risk
levels. This wellness committee will generate motivation on the
floor and provide word-of-mouth advertising before the start of
the intervention. Mailers will be sent out to all employees a month
before the program. These will encourage employees to take baby
steps toward the program, including parking further away from
the building, bringing lunch versus ordering out, and being active
during scheduled breaks. The company Wellness Coordinator will
partner with the onsite cafe to update the menu from high sodium
and carbohydrate options to healthier food choices. The wellness
team will use Microsoft Teams to send random alerts, such as Drink
Water and Get Up and Move. A Registered Dietitian will be available
onsite once a month for participants who would like a nutritional
consult.
This employee program will target high-risk employees who
volunteer to participate. A company health survey concentrating on
risk factors for CVD and mental wellness caused during COVID-19
will be sent out to employees introducing the Health Belief Model
(HBM) and the Transtheoretical Model (TTM). This will help
the wellness team identify the stage of change employees fall
under and rank participants according to willingness to change.
Enlisting employees prepared to engage in lifestyle changes will
allow them to utilize their resources efficiently. Introducing a
lifestyle management program that supports and encourages
employee participation will help them make better lifestyle choices.
Employees will have easy access to practice in a number of lifestyle
modifications at work.
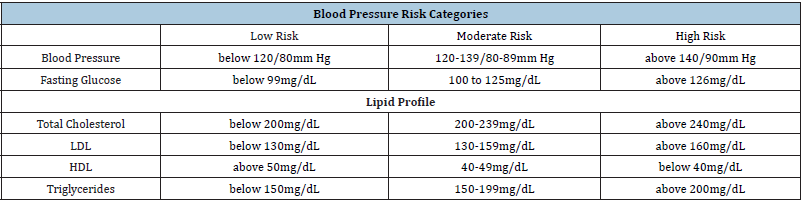
This program will begin with a biometric screening to measure
employee’s blood pressure, blood sugar, cholesterol, triglycerides,
and BMI. According to the TTM, moderate or high-risk employees
will be classified into the preparation phase; and low-risk employees
can be categorized into the maintenance phase. The Wellness
Coordinator will design an infographic to email all participants.
This infographic will include reference ranges for BMI and blood
levels along with CDC risk levels. Biometric screening numbers
will measure program success, with the goals being a decrease in
COVID-19 and CVD occurrences among company employees (Table
3).
Table 3:
A Registered Dietitian will instruct high-risk participants to decrease their caloric intake and maintain a nutrition journal for accountability. The wellness team will promote Trot the Lot to encourage participants to walk five times a week, for 15 minutes a day at work. Participants will be provided with the same metrics from the biometric screening measured quarterly to see their results. The wellness committee team will support focused initiatives and show continued enthusiasm throughout the program. They will be able to provide feedback from the floor to share employees’ ideas and critiques. There will be a physical and virtual Health Champion wall to recognize employee participation and provide incentives to employees who have achieved success. Support and encouragement are vital to the program. Employees at risk for COVID-19 or CVD can experience the benefits of a proper nutrition program, stress management, and an exercise regime through a workplace initiative [9,10]. Those who have adopted healthier behaviors and see the benefits will likely share their positive experiences with other employees, allowing them to become health advocates.
Conclusion
The global pandemic of COVID-19 has impacted social and workplace environments. The workplace presents an important environment to focus efforts on both mental and physical health issues. Major employee health concerns include increased stress, anxiety, and lack of physical activity – all of which contribute to CVD. Improvement of workplace conditions, including the adoption of anti-contagion measures and requirements of personal protective equipment such as masks can create a more safe and healthy work environment. The goals of employee health promotion programs should be to create an environment that encourages employees to make healthy choices voluntarily. Participants in employee health promotion programs can adapt lifestyle changes. Healthier employees will lead to an increase productivity, satisfaction, and overall quality of life.
References
- Giorgi G, Lecca L, Alessio F, Finstad G, Bondanini G, et al. (2020) Review COVID-19-related mental health effects in the workplace: A narrative review. International Journal of Environmental Research and Public Health 17(21): 1-22.
- Gans KM, Salkeld J, Risica PM, Lenz E, Burton D, et al. (2015) Occupation is related to weight and lifestyle factors among employees at worksites involved in a weight gain prevention study. Journal of Occupational and Environmental Medicine 57(10): 114-120.
- Oh H, Park H, Boo S (2017) Mental health status and its predictors among call center employees: A cross-sectional study. Nursing & Health Sciences 19(2): 228-236.
- Bhutani, S, Cooper JA (2020) COVID‐19-related home confinement in adults: Weight gain risks and opportunities. Obesity Research Journal 28(9): 1576-1577.
- Lockhart SM, ORahilly S (2020) When two pandemics meet: Why is obesity associated with increased COVID-19 mortality? Medical Journal: Cell Press 18(1): 33-42.
- Siqueira JV, Almeida LG, Zica BO, Brum IB, Barceló A (2020) Impact of obesity on hospitalizations and mortality, due to COVID-19: A systematic review. Obesity Research & Clinical Practice 14(5): 398-403.
- Brocq SL, Clare K, Bryant M, Roberts K, Tahrani A (2020) Obesity and COVID-19: A call for action from people living with obesity. The Lancet Diabetes & Endocrinology 8(8): 652-654.
- Freitas PP, Menezes MC, Santos LC, Pimenta AM, Ferreira AV, et al. (2020) The transtheoretical model is an effective weight management intervention: A randomized controlled trial. BMC Public Health 20(1): 246-262.
- Rippe JM (2018) Lifestyle strategies for risk factor reduction, prevention, and treatment of cardiovascular disease. American Journal of Lifestyle Medicine 13(2): 204-212.
- Siqueira JV, Almeida LG, Zica BO, Brum IB, Barceló A (2020) Impact of obesity on hospitalizations and mortality, due to COVID-19: A systematic review. Obesity Research & Clinical Practice 14(5): 398-403.
© 2021 Tina M Penhollow. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






