- Submissions

Full Text
Associative Journal of Health Sciences
Predictors of Receiving the HPVVaccination Among University Students
Tina M Penhollow1*, Michael Hall1 and Michael Young2
1Department of Exercise Science and Health Promotion, Florida
2 CEO Center for Evidence Based Programming, Florida
*Corresponding author:Tina M Penhollow, Associate Professor, Department of Exercise Science & Health Promotion, Florida Atlantic University, USA
Submission: October 09, 2019;Published: October 17, 2019

ISSN:2690-9707 Volume1 Issue2
Abstract
Introduction: The Human papillomavirus (HPV) is the most common sexually transmitted infection (STI) in the United States. The HPV vaccine is a common and popular way to effectively reduce the chances of being infected. The purpose of the study was to identify variables which distinguished between college students who received the HPV vaccine and those who did not receive the vaccine.
Methods: Students from one university in the southeastern United States was employed as the study sample. Participants completed a questionnaire that included items designed to elicit information concerning demographics, sexuality, religiosity, as well as knowledge and behaviors about the HPV vaccine. Data were analyzed using SPSS programs.
Results: Frequency counts, confirmatory factor analysis, and multivariate logistic regression analyses were conducted on the data. Total participants in the research were N=257 (females n=194; males n=63). Nearly half of the sample had received the HPV vaccine (n=110, 43%), more than a quarter reported not receiving the vaccine (n=87, 34%), and less than a quarter reported they did not recall whether or not they received the HPV vaccination (n=56, 23%). The top five reasons provided for choosing not to receive the HPV vaccine were: the vaccine was unnecessary, not sexually active, parent/guardian, did not want another vaccination, and belief the vaccine was dangerous. The top five reasons given for choosing to receive the vaccination were: understood the purpose, parent/guardian, thought it was safe, sexually active, and thought it was necessary. Male gender, extreme religious involvement, and Black race were the identified statistically significant variables to predict lack of receiving the HPV vaccine.
Conclusion: Our findings add to the existing body of literature in health science. Health professionals should work to develop interventions that provide education about sexual health among college students which include the benefits and risks of receiving the HPV vaccination.
Keywords: College students; Human papillomavirus (HPV); Vaccination; Religion; Sexual health
Introduction
The Human papillomavirus (HPV) is the most common sexually transmitted infection (STI) in the United States and is associated with increased cancer risks [1]. According to current data, an estimated 79 million Americans are currently infected with HPV. It is predicted that 14 million new infections will develop every year, in which nearly half will occur among young adults 15 to 24 years of age [2]. Due to the high prevalence rates of the HPV and its association with many different cancers, researchers discovered a vaccine to combat the virus. In 2006, the U.S. Food and Drug Administration (FDA) first licensed and introduced the quadrivalent Human papillomavirus(types 6, 11, 16, and 18) recombinant vaccine (qHPV), and it is now commonly recommended for females age 11 to 26 and males 11 to 21 years of age [3-6].
The HPV vaccine (Gardasil or Cervarix) is a popular method to reduce the likelihood of being affected with the virus and it is most generally administered to adolescents with an aim to protect individuals against cervical, vulvar, vaginal, penile, anal, and oropharynx cancers [7]. The vaccine was reported to be the most expensive gender-specific vaccine in U.S. history [8]. The shot is given in a series of 3 injections over 6 months. The vaccine is aimed to protect against four of the over 100 strains of HPV. Despite the prevalence and dangers of contracting and spreading HPV, previous studies have found that vaccination rates are not very high [9,10]. The Advisory Committee on Immunization Practices (ACIP) recommends catch-up HPV vaccinations for young adults who were not vaccinated during their adolescent years [2].
The National Health and Nutrition Examination Survey (NHANES) was utilized to analyze HPV DNA prevalence in cervicovaginal specimens from females age 14 to 34 years in the pre vaccine era (2003-2006) and 4 years in the vaccine era (2009- 2012) by age group. NHANES is an ongoing series of cross-sectional surveys conducted by the National Center for Health Statistics (NCHS) and the Centers for Disease Control and Prevention (CDC). Between the pre vaccine and vaccine eras, the prevalence of HPV declined from 11.5% to 4.3% among females 14 to 19 years of age, and 18.5% to 12.1% among females 20 to 24 years of age. There were no reported statistically significant decreases in receiving or not receiving the HPV vaccine among females 25 years of age and older [11].
HPV vaccination rates have been shown to be affected by perceived risks and benefits, general knowledge of the vaccine, physician recommendations, and parental attitudes and beliefs toward the vaccine [12,13]. Hesitancy of parents, health care providers, and education are the greatest obstacles to receiving the HPV vaccination [14]. Studies have also revealed the reasons for opting out of vaccination seems to differ between ethnicities and age groups [15]. The National Center for Health Statistics (NCHS) has reported that the prevalence of any and all high-risk oral and genital HPV has been shown to be lowest among non-Hispanic Asian adults and highest among non-Hispanic Black adults [16].
There seems to be little awareness spread among the college age population and less research conducted on this population who can now independently decide to be vaccinated. Not only is awareness lowest among the college population, but the relevance of the vaccine is significantly greater than that of the adolescent population given that sexual promiscuity is historically reported as a reason for opting out of vaccination for parents of adolescents [17]. It was discovered out of a sample population of 124 college students among two different universities, approximately 75% reported having heard of HPV before. Generally, females reported greater awareness than males. The greater interest in becoming vaccinated was found more so among sexually active women [18]. There seems to be an educational gap between male and female knowledge of HPV. A recent study analyzed data from the National Cancer Institute’s 2014 Health Information National Trends Survey (HINTS). Significant gender differences in awareness and knowledge of HPV and the HPV vaccine were revealed. Investigators reported lower HPV knowledge among men and some racial minorities. Women were more likely to report that a health care provider recommended vaccination. Significant predictors of general HPV and HPV vaccine knowledge included gender, education, income, race, relationship status, and other sociodemographic characteristics [19].
A recent investigation found that the uptake of the HPV vaccine is much lower within the college population compared to the adolescent population [20]. Their research stated only 10% of females age 18 to 26 had had been vaccinated and 37% of females age 13 to 17 received the vaccination when Gardasil recommendations were first published. Among their sample population, 29% of their participants reported not getting the vaccine because they did not feel at risk for STIs. Some respondents had reported being in a monogamous relationship as a reason for non-vaccination as well indicating a lack of education on the virus. Many of the respondents who were sexually active had commented they felt it was too late to receive the vaccine which may also indicate a strong need to provide more education on sexual health to this population, as receiving the vaccine later in age may still protect from strands an individual has not been exposed to yet. Surya devera and colleagues (2016) discovered that the majority of their sample population of college students reported a lack of physician recommendation as the main reason for choosing not to be vaccinated. They also found that the likelihood of vaccination decreased as patients transitioned to nonpediatric health care. Additionally, more than 10% of the college students who were surveyed stated they did not have a health care provider [21].
While it is widely recommended for females to receive the HPV vaccination, male vaccination is still encouraged; however, male vaccination rates remain significantly lower in comparison to females [22,23]. There has been a great deal of confusion as to whether or not males should receive the HPV vaccine among patients. A recent study found that only 14% of male adolescents had been vaccinated among their sample population while 44% of females reported being vaccinated. When parents were asked to give the main reason for choosing not to vaccinate their son against HPV, parents of sons were more likely than those of daughters to report not having received a healthcare provider’s recommendation or not knowing the vaccine was available for their son. Moreover, parents of sons were not as likely to report concern about safety; 44% of unvaccinated sons were not vaccinated due to parents not being aware that the vaccine was available for males. However, this study collected data in 2010, which was before the HPV vaccine was recommended by the U.S. Centers for Disease Control and Prevention (CDC) [23].
In a recent cross-sectional online survey distributed to 383 university students by Barnard and colleagues (2017), data showed that only 34% of males agreed that they needed to be vaccinated even if they had a steady long-term sexual partner. Meanwhile, female results showed that 58% strongly agreed with receiving vaccination even if they were in a monogamous relationship. The perception of vaccine safety does seem to differ between male and female college students as well. It was reported 59% of the females surveyed believed that the vaccine is overall safe, while 51% of males believed it was safe. This slight difference could potentially be attributed to the educational gap and the initial marketing of HPV vaccines being mainly targeted toward females. Their research also reported a difference in awareness of the HPV vaccine in general among male and female students. They indicated that 92% of females were aware that there was an HPV vaccine, while 83% of males had heard of the vaccine. Additionally, their data revealed that 90% of male students reported never having seriously thought about getting vaccinated, while only 63% of females reported the same. This study discovered that the vast majority of college students are still not vaccinated [2].
Religiosity has also been a factor shown to influence HPV vaccine acceptance and vaccination rates. According to a recent study of 20,495 adolescents from 50 U.S. states using the Teen National Immunization Survey (NIS), significant state-level predictors of receiving the HPV vaccine included sex education policy, religiosity, and HPV vaccine mandates. States with the lowest HPV vaccination rates were found to be the states considered to be the most conservative and highly religious [24]. One study of a diverse sample of females age 9 to 17 years revealed parents with frequent attendance at religious services were more likely to not have vaccinated their daughters with the HPV vaccine, compared with parents who did not attend religious services [25]. Another recent investigation using a random sample telephone survey of parents with an eligible daughter found five main reasons for nonacceptance of the HPV vaccine: concerns about effects on sexual behavior, specific HPV concerns, moral objections to sexual involvement, general vaccine concerns, and denial of need [26].
Similar findings relative to religion and HPV vaccination rates have been shown among the college population. A sample of single college students age 18 to 25 years found those who were the most highly religious were also the students who demonstrated the lowest knowledge of HPV and the HPV vaccination. High religious beliefs were associated with lower HPV vaccination rates [27]. Another study among college students found more frequent religious attendance and higher degree of parental monitoring were associated with a greater likelihood of deciding against HPV vaccination [28]. Among a sample of female college students, those who reported themselves as atheist or not religious were more likely to support HPV vaccination mandates [29].
It should be noted that with every vaccine or medication there exists potentially dangerous side effects. The U.S. Centers for Disease Control and Prevention (CDC) and the Federal Drug Administration (FDA) maintains the Vaccine Adverse Events Reporting System (VAERS). It was reported that the VAERS reporting rate for the HPV vaccine was triple the rate for all other vaccines combined from June 2006 until December 2008 [30]. After relatively 23 million doses total, serious adverse side effects included venous thromboembolism, Guillain-Barre syndrome (paralysis lasting for years or permanently – sometimes causing suffocation), lupus, seizures, blood clots, brain inflammation, autoimmune disorders, pancreatitis, anaphylaxis, transverse myelitis, motor neuron disease, and death [31-33].
Dr. Diane Harper was the lead researcher in the development of the human papilloma virus vaccines, Gardasil and Cervarix. In 2009 at the 4th International Public Conference on Vaccination in Reston, Virginia she presented unexpected information regarding the HPV vaccine. Her speech was anticipated to promote the Gardasil and Cervarix vaccines for Merek & Co. pharmaceuticals, however that was not the case. She stated relatively eight in every ten women who have been sexually active will have HPV at some stage in their life. There are typically no symptoms, and in most cases the virus clears itself. These two vaccines only target four strains out of over 100 for a specific ailment that usually dies on its own. She noted that cervical cancer can be most curable if detected early through normal Pap Smear screenings [32,34].
Purpose of the study
The purpose of the present study was to assess, compare, and contrast variables which predict college students who have received the HPV vaccine and those who have not received the HPV vaccine. This study attempts to extend past research by including measures of religiosity, which may impact vaccination decisionmaking. Understanding how religiosity influences sexual behavior may be of value in developing effective programs aimed at reducing sexual risk-taking among young adults. We hypothesized that age, gender, race, relationship status, and religiosity variables would help to distinguish between those who had and those who had not received the HPV vaccine for both male and female college students.
Methods
Participants
Data were collected from a random convenience sample of undergraduate and graduate students enrolled in several different courses at a large public southeastern university. These classes were utilized for the study as they attract a cross-section of both male and female college students from diverse majors and years in college. Participants voluntarily completed a questionnaire concerning demographic variables, religious data, and information about the HPV vaccine. All participants signed a “yes” or “no” agreement prior to completion of the survey, which indicated implied consent. Two undergraduate students from the College of Medicine and one undergraduate student from the College of Nursing assisted the researchers in recruiting students to participate in the investigation. Participation rate was approximately 95%. Institutional Review Board (IRB) approval was granted prior to the implementation of the study.
Instrumentation
The testing instrument was a questionnaire that included demographic characteristics, religiosity items, selected sexual behavior items, as well as questions addressing HPV. Demographic variables included age, gender, race, sexual orientation, and relationship/marital status. Religiosity questions addressed an item concerning their current belief system and an item relative to the degree of their current religious involvement. These religiosity items have been validated in previous research among college students [35,36]. Selective sexual behavior items were included. Additionally, questions concerning HPV knowledge, as well as a variety of behavioral questions concerning reasons for choosing to receive or not to receive the HPV vaccine were included in the questionnaire.
Data analysis
Researchers utilized version 23.0 of SPSS programs to complete the data analysis. Data were analyzed using frequency counts, confirmatory factor analysis, and multivariate logistic regression. Data for males and females were analyzed collectively. The level of significance was set at p<.05.
Results
Demographics of respondents
Total participants in the research investigation were N=257 (females n=194; males n=63). Most of the sample reported they were born in the United States (n=208, 81%). Almost half of the sample reported their race as White (n=124, 48%); while 22% (n=56) indicated they were Hispanic; 19% (n=48) indicated they were Black; 5% (n=12) reported they were Asian; and 6% (n=17) reported themselves as “other”. The majority of participants indicated they were 21-23 years of age (n=123, 48%); 19% (n=48) were 18-20 years old; 19% (n=48) were 24-27 years of age; and the remainder reported their age as 28 and older (n=36; 14%). Relative to sexual orientation, most of the respondents were heterosexual (n=234, 91%); while 5% (n=9) reported to be bisexual; and 4% reported to be homosexual (n=8). When questioned about their relationship/marital status, the majority reported being in a committed relationship (n=118, 46%); while 22% (n=56) indicated they were single and not dating; 20% (n=50) were single and casually dating; 6% (n=15) were married; 4% (n=9) were divorced; and the remainder reported their relationship/marital status as either separated or widowed (2%, n=3).
Frequency/percentages of religiosity variables
Study participants were questioned about their chosen religious belief systems and religious practices. Almost half of the respondents reported themselves as Christian (n=112, 44%); 21% (n=52) were Catholic; 8% (n=21) were Jewish; 6% (n=16) were Agnostic; 5% (n=12) were Atheist; 2% (n=6) were Muslim; 1% reported themselves as Buddhist (n=2) and Mormon (n=1); some participants indicated “other” (n=18, 7%); and the remainder reported they preferred not to respond (n=12, 5%). Religious involvement revealed relatively close percentages among the sample population. The greatest number of students indicated moderate religious involvement (n=60, 24%); followed by minimal religious involvement (n=54, 21%); some religious involvement (n=50, 20%); no religious involvement (n=40, 16%); high religious involvement (n=39, 15%); and extreme religious involvement (n=8, 4%).
Frequency/percentages of sexual behaviors & HPV knowledge
Study participants were asked about their current sexual behaviors. The majority of the sample indicated they were currently sexually active (n=210, 82%). When asked about the age bracket in which they became sexually active, more than half of the sample indicated 17-20 years of age (n=117, 59%); the remainder indicated 13-16 years of age (n=57, 28%); followed by 21-26 years of age (n=27, 13%). Almost half of the sample revealed they have had 1-3 sexual partners (n=99, 49%); the remainder indicated 4-6 sexual partners (n=33, 16%); 7-10 sexual partners (n=23, 11%); 11-15 sexual partners (n=19, 9%); 16-20 sexual partners (n=9, 4%); 21 or more sexual partners (n=7, 3%); and 8% (n=15) preferred not to respond. Concerning preventative sexual health of female respondents, 36% (n=69) of the sample reported they have undergone a Pap Smear within the last six months; 30% (n=58) have never had a Pap Smear; 20% (n=38) had a Pap Smear within the last year; 12% (n=22) had a Pap Smear within the last two years; and 2% (n=5) did not recall the last time they had a Pap Smear.
Participants were questioned about their overall knowledge and selective behaviors concerning the HPV vaccine. Relative to overall knowledge of the HPV vaccine, 36% (n=90) revealed they had discussed the HPV vaccine with a medical professional; 34% (n=87) had heard of the HPV vaccine; 17% (n=43) had discussed the HPV vaccine casually; 8% (n=21) reported having extensive knowledge about the HPV vaccine; and 5% (n=11) had never heard of the HPV vaccine before taking the study questionnaire. Nearly half of the respondents (n=105, 42%) reported that everyone at a specific age bracket may obtain the HPV vaccine; 33% (n=85) indicated that everyone at any age could receive the vaccine; 14% (n=37) believed only females at a specific age bracket may receive the HPV vaccine; 7% (n=19) thought that only females could receive the vaccine; 2% (n=2) believed only males at a specific age bracket may receive the HPV vaccine; and 2% (n=2) reported they believed only males could receive the HPV vaccination.
Participants were asked whether or not they have been diagnosed with a Human papillomavirus(HPV) infection. The majority of the sample indicated they have not been diagnosed with HPV (n=213, 88%); 10% (n=24) revealed they have been diagnosed with HPV; and 2% (n=6) revealed they were not sure whether or not they have been diagnosed with HPV. Nearly half of the sample indicated they had received the HPV vaccine (n=110, 43%); more than a quarter reported not receiving the vaccine (n=87, 34%); and less than a quarter reported they do not recall whether or not they received the HPV vaccination (n=56, 23%).
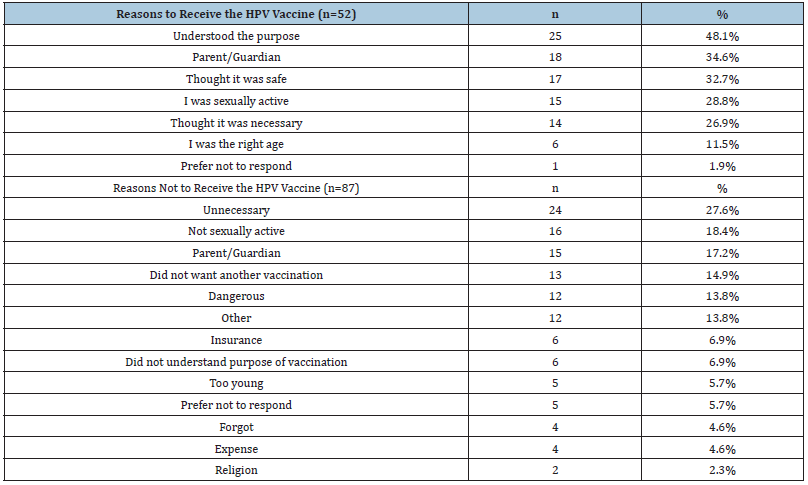
Participants were asked if their parent(s) or guardian(s) influenced their decision to receive the HPV vaccine. Of the respondents who received the vaccine, 64% revealed their parent(s) or guardian(s) wanted them to have the vaccine; 30% indicted their parent(s) or guardian(s) did not want them to have the HPV vaccine; and 6% preferred not to respond. Most respondents revealed they were offered the HPV vaccine at the age of 13-16 (n=64, 25%). The remainder of the participants reported they did not recall the age in which they were offered the HPV vaccine (n=52, 20%); 20% (n=50) reported they have never been offered the HPV vaccine; 18% (n=44) indicated 17-20 years of age; 9% (n=22) indicated 8-12 years of age; 4% (n=11) indicated 21-26 years of age; and 4% (n=10) reported they were offered the HPV vaccine at 27 years of age and older. Of the respondents who reported they had received the HPV vaccine, 8% (n=10) indicated they experienced negative consequences due to the HPV vaccination. The main side effects reported were pain, redness, or swelling in the arm where the shot was given. The top five reasons provided for choosing to receive the vaccination were: (1) understood the purpose, (2) parent/guardian, (3) thought it was safe, (4) currently sexually active, and (5) thought it was necessary. The top five reasons provided for choosing not to receive the vaccine were: (1) thought it was unnecessary, (2) not currently sexually active, (3) parent/guardian, (4) did not want another vaccination, and (5) thought it was dangerous. Please see Table 1.
Table 1:Reasons provided for receiving and not receiving the HPV vaccine.
Confirmatory factor analysis
Construct validity was examined by performing principal component factor analysis on all subscales included in the testing instrument. Separate factor analyses were conducted for each subscale under investigation. Factor-based scores were obtained from variables that demonstrated meaningful loadings for each component under examination. Factor loading subscales ranged from .61 to .99, indicating that the magnitudes for every construct under investigation were strong (>.60).
Multivariate logistic regression
Table 2:Multivariate logistic regression: No HPV vaccination and HPV vaccination.
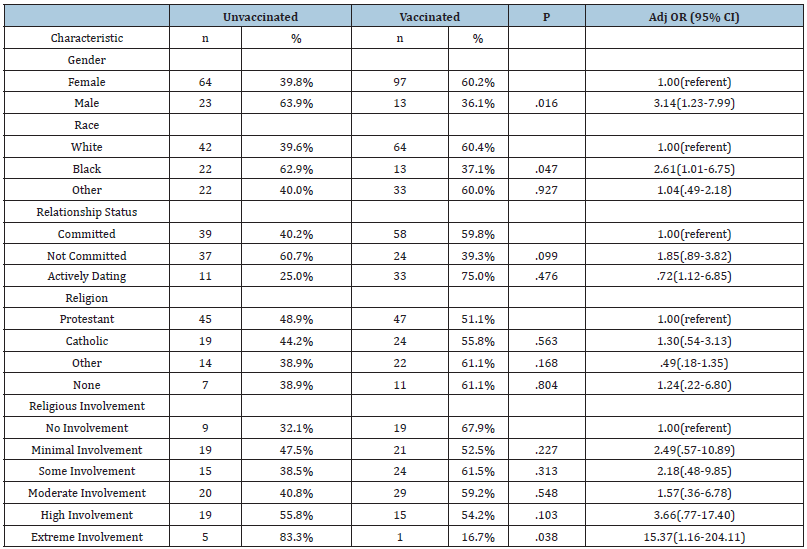
Age, gender, race, relationship status, and religious variables were entered into a multivariate logistic regression model to assess predictors of not receiving the HPV vaccination. Male gender [AOR=3.1; 95% CI=1.2-7.9; p<.02], extreme religious involvement [AOR=15.4; 95% CI=1.2-204.1; p<.04], and Black race [AOR=2.6; 95% CI=1.0-6.8; p<.05] were the identified statistically significant variables to predict lack of receiving the HPV vaccine. Male gender and extreme involvement in religious practices were each more likely to not be vaccinated against HPV. Of those reporting their race, Blacks were significantly 2.6 times less likely to be vaccinated against HPV compared to the other races reported. Please see Table 2.
Discussion
The results of the present study partially supported our research hypothesis. As theorized, findings of our study confirmed the association of gender, race, and religiosity variables relative to distinguishing between those who had and those who had not received the HPV vaccine for both male and female college students. Age and relationship status did not significantly impact the prediction of receiving or not receiving the HPV vaccination for all participants.
Overall findings of our investigation support the data of previous research. General knowledge of the HPV vaccine seems to be lacking among the college age population [12-14,18,20]. Congruent with similar studies, our data supports that race/ethnicity impacts HPV vaccination rates. Non-Hispanic Black adults have been continually reported to be the majority who have not received the HPV vaccine [15,16,19]. Additionally, rates of receiving the HPV vaccination have been reported to be significantly lower among male college students as compared to female college students [22,23].
This study adds to the literature in evaluating selective items regarding the impact of religion as related to receiving the HPV vaccination. Many religious groups have considerations, concerns, and restrictions relative to governmental vaccinations. Our sample found that participants who indicated extreme religious involvement were also less likely to receive the HPV vaccine. These findings are congruent with previous investigations in that more religious involvement was predictive of less likelihood in the uptake of the HPV vaccination [24-29]. Religiosity continues to have an impact on many facets of sexuality and sexual behaviors, including the decision to receive or not to receive certain vaccinations.
Limitations
Interpretation of these results should take the limitations of the study into account. Participants consisted of a convenience sample of undergraduate college students enrolled at one university. Thus, these results may not apply to non-college populations. The percentage of females in the sample is greater than the percentage of males, indicating the sample may not be representative of the university population as a whole. Additionally, the study instrument consisted of a self-report questionnaire. There is a possibility of response bias due to false or socially desirable responses. A crosssectional research design was employed, indicating that correlates of behavior were assessed rather than antecedents of behavior. Future research should attempt to include a greater percentage of males, other racial and ethnic groups, as well as participants with different sexual orientations. Longitudinal research examining a multitude of religiosity factors and changes in sexual behaviors over time may prove beneficial to further understanding why young adults choose or not choose to receive the HPV vaccine.
Conclusion
From past to current research it appears that misconceptions, knowledge gaps, and a failure to educate relevant populations about HPV and the opportunities to vaccinate are still influencing the significantly low vaccination rates across gender, race, and age groups. Much of the literature points to a need for more education about sexual health among college students, as health care providers do not always seem to recommend vaccines based on their own judgements and beliefs. Religion also appears to impact vaccination decision-making. Interventions could be developed to provide sexual education to college students as well as opportunities to be vaccinated, since the window to prevent the spread of HPV does not immediately close after adolescence. It should be noted that a multitude of side effects, including autoimmune illnesses have been reported in several research studies and reports.
Providing college students with accurate knowledge of the risks and benefits associated with the HPV vaccine will equip them to make independently informed decisions relative to receiving or not receiving the HPV vaccine. Data from both governmental and nongovernmental sources contribute to the increasing body of knowledge regarding all available vaccinations [37]. Ongoing research provides important information that will continue to impact health insurance coverage and vaccine policy changes in the United States and abroad.
Acknowledgement & Conflict of Interest
This data was presented internationally at the Society for the Scientific Study of Sexuality (SSSS) conference in Montreal, Canada. There is no financial or other conflict of interest.
References
- Centers for Disease Control and Prevention (CDC) (2019) Genital HPV infection: Fact sheet.
- Barnard M, George, Perryman M, Wolff L (2017) Human papillomavirus (HPV) vaccine knowledge, attitudes, and uptake in college students: Implications from the precaution adoption process model. Journal of Adolescent Health 12: 1-9.
- Mac Arthur K (2017) Beyond health beliefs: the role of trust in the HPV vaccine decision making process among American college students. Health Sociology Review 26(3): 321-338.
- Markowitz L, Dunne, Saraiya, Lawson, Chesson, et al. (2007) Centers for Disease Control and Prevention (CDC). Advisory Committee on Immunization Practices (ACIP). Morbidity and Mortality Weekly Report (MMWR) 56: 1-24.
- Romanowski B (2011) Long term protection against cervical infection with the Human papillomavirus: Review of currently available vaccines. Journal of Human Vaccines 7(2): 161-169.
- Slade, Leidel, Vellozzi, Woo, Hua, et al. (2009). Postlicensure safety surveillance for quadrivalent Human papillomavirus recombinant vaccine. Journal of the American Medical Association 302(7): 750-757.
- Saraiya, Unger, Thompson, Lynch, Hernandez, et al. (2015) US assessment of HPV types in cancers: Implications for current and 9 valent HPV vaccines. Journal of the National Cancer Institute 107(6):
- Bryan J (2007) Developing an HPV vaccine to prevent cervical cancer and genital warts. Vaccine 25(16): 3001-
- Fontenot, Fantasia, Charyk, Sutherland (2014) Human Papillomavirus (HPV) risk factors, vaccination patterns, and vaccine perceptions among a sample of male college students. American Journal of College Health 62(3): 186-192.
- Manikandan, Behera, Naidu, Angamuthu, Mohammed, et al. (2019) Knowledge and awareness toward cervical cancer screening and prevention among the professional college female students. Journal of Pharmacy and Bioallied Sciences 11(Supp2): S314-S320.
- Markowitz, Lui, Hariri, Steinau, Dunne, et al. (2016) Prevalence of HPV after introduction of the vaccination program in the United States. Pediatrics 137(2).
- Winger, Christy, Mosher (2015) Association of health behaviors with human papillomavirus vaccine uptake, completion, and intentions among female undergraduate students. Journal of Health Psychology 21(9): 1949-1955.
- Ziemer, Hoffman (2012) Beliefs and attitudes regarding the Human papillomavirus vaccination among college-age women. Journal of Health Psychology 18(10): 1360-1370.
- Hernandez, Daley, Young, Kolar, Wheldon, et al. (2019). HPV vaccine recommendations: Does a health care provider’s gender and ethnicity matter to unvaccinated Latina college women. Ethnicity & Health 24(6): 645-661.
- Ylitalo, Lee, Mehta (2013) Health care provider recommendation, Human papillomavirus vaccination and race/ethnicity in the U.S. National Immunization Survey. American Journal of Public Health 103(1): 164-169.
- McQuillan, Kruszon M, Markowitz, Unger, Paulose (2017) Prevalence of HPV in Adults Aged 18-69: United States, 2011-2014. National Center for Health Statistics (NCHS).
- Best A, Thompson E, Adamu A, Logan, Delva, et al. (2019). Examining the influence of religious and spiritual beliefs on HPV vaccine uptake among college women. Journal of Religion and Health.
- Gerend, Majloire (2008) Awareness, knowledge, and beliefs about Human papillomavirus in a racially diverse sample of young adults. Journal of Adolescent Health 42: 237-242.
- Bride, Singh (2017) Predictors of adults’ knowledge and awareness of HPV, HPV associated cancers, and the HPV vaccine: Implications for health education. Health Education and Behavior 45(1).
- Patel, Zochowski, Peterman, Dempsey, Ernst, et al. (2012) Human papillomavirus vaccine intent and uptake among female college students. Journal of American College Health 60(2): 151-161.
- Suryadevara, Bonville, Kline, Magowan, Domachowske, et al. (2016) Student HPV vaccine attitudes and vaccine completion by education level. Human Vaccines & Immunotherapeutics 12(6): 1491-1497.
- Cooper, Zellner L, Mubasher, Banerjee, Hernandez (2018) Examining HPV awareness, sexual behavior, and intent to receive the HPV vaccine among racial/ethnic male college students 18-27 years. American Journal of Men’s Health 12(6): 1966-1975.
- Gilkey, Moss, McRee, Brewer (2012) Do correlates of HPV vaccine initiation differ between adolescent boys and girls. Vaccine 30(41): 5928-5934.
- Franco, Mazzucca, Padek, Brownson, (2019) Going beyond the individual: How state-level characteristics relate to HPV vaccine rates in the United States. BMC Public Health 19.
- Shelton, Snavely, De Jesus, Othus, Allen, et al. (2013) HPV vaccine decision-making and acceptance: Does religion play a role? Journal of Religion and Health 52(4): 1120-1130.
- Constantine, Jerman (2007) Acceptance of human papillomavirus vaccination among Californian parents of daughters: A representative statewide analysis. Journal of Adolescent Health 40(2): 108-115.
- Birmingham, Macintosh, Vaughn, Graff (2019) Strength of belief: Religious commitment, knowledge, and HPV vaccination adherence. Psycho-Oncology.
- Quinn, Lewin, (2019) Family factors associated with emerging adults’ human papillomavirus vaccine behavior. Journal of American College Health.
- Rosen, Thompson, Kelly, Mathew Lee (2017) Do political and religious affiliations impact HPV vaccine mandate support? Health Behavior and Policy Review 4(5): 472-483.
- Eberth, Kline, Moskowitz, Montealegre, Scheurer (2014) The role of media and the Internet on vaccine adverse reporting: A case study of HPV vaccination. Journal of Adolescent Health 54(3): 289-295.
- Chao, Klein, Velicer, Sy L, Slezak, et al. (2012) Surveillance of autoimmune conditions following routine use of quadrivalent human papillomavirus Journal of Internal Medicine 271(2): 193-203.
- Harper (2009) Gardasil needs a new consent form. Vaccines 8(12): 1613-1614.
- Souayah, Michas Martin, Nasar, Krivitskaya, Yacoub, et al. (2011) Guillain Barre syndrome after gardasil vaccination: Data from the vaccine adverse event reporting system (VAERS) 2006-2009. Vaccine 29(5): 886-889.
- Corriher (2009) The lead vaccine developer comes clean about Gardasil and Cervarix. The Health Wyze Report, USA.
- Penhollow, Young, Denny, (2012) Impact of personal and organizational religiosity on college student sexual behavior. American Journal of Health Studies 27: 13-2.
- Young, Denny, Penhollow, Palacios, Morris (2015) Hiding the word: Examining the relationship between a new measure of religiosity and sexual behavior. Journal of Religion and Health 54(3): 922-942.
- Petrosky, Bocchini, Hariri, Chesson, Curtis, et al. (2015) Use of 9-valent human papillomavirus (HPV) vaccine: Updated HPV vaccination recommendations of the advisory committee on immunization practices. Morbidity and Mortality Weekly Report (MMWR) 64(11): 300-304.
© 2019 Tina M Penhollow. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






