- Submissions

Full Text
Advancements in Case Studies
Wound Treatment Assessment with Three-Dimensional Planimetry Scanning and Images in Multifrequency Light- A Case Report
Rita I Sharma1*, Jacek Kot1#, Piotr Tojza2#, Leszek S Litzbarski2# and Grzegorz Redlarski2,3#
1National Centre for Hyperbaric Medicine, Institute of Maritime and Tropical Medicine in Gdynia, Medical University of Gdansk, Poland
2Department of Electrical and Control Engineering, Gdansk University of Technology, Poland
3BioTechMed Center, Gdansk University of Technology, Poland
#These authors contributed equally to this work
*Corresponding author:Rita I Sharma, National Centre for Hyperbaric Medicine, Institute of Maritime and Tropical Medicine in Gdynia, Medical University of Gdansk, 80-210 Gdansk, Poland
Submission:March 21, 2024;Published: April 02, 2024

ISSN 2639-0531Volume4 Issue2
Abstract
Chronic wounds as a problem touching mostly elderly people leads to movement disability and gradual loss of life quality. In this group of wounds, we can differentiate i.a. diabetic foot and ischemic ulcers. Treatments consists of special dressings, regular surgical debridement, antibiotic therapy, hyperbaric oxygen therapy and if possible, removing the cause of circulatory malfunction. Wound assessment is problematic in outside outpatient clinic and still remains challenging with human vison objectification. Simple, low cost and repeatable method is photographic documentation. Visible light, infrared light and ultraviolet light pictures together with three-dimensional planimetry give the opportunity to compare wound size before and after treatment and easily assess its effectiveness.
Keywords:Chronic wound; Planimetry; Diabetic foot; Visible light; Infrared light; Ultraviolet light
Introduction
Non-healing wound defined as a failure in healing process remains an underestimated factor diminishing life quality of worldwide population [1]. The definition of non-healing wounds states a failure in healing lasting for over 4 weeks, despite multimodal treatment as surgical procedures, antibiotic therapy, hyperbaric oxygen therapy (HBOT). Among reasons disturbing proper healing process we can enlist diabetes, circulation malfunctioning, immunology insufficiencies and malnutrition. Most patients are elderly people with many comorbidities, often suffering from all mentioned above risk factors [2]. The complications and treatment failures leading to mortality are comparable to cancer mortality [3]. Proper wound assessment, multimodal treatment with dedicated dressings, etc. leads to wound healing acceleration. However, in chronic wounds the decision taking about amputation versus continuing the therapy may cause difficulties. Decision making may be eased by transcutaneous oximetry [4-6] and wound surface assessment including area, volume and wound content [7,8]. Still visual assessment, especially due to staff rotations, sunlight, etc. does not bring objective conclusions.
Transcutaneous oximetry is a minimally invasive, painless method assessing tissue perfusion and oxygenation degree [9,10]. The oxygen partial pressure (pO2) of tissues surrounding the wound refers to perfusion and blood vessels functioning. Tissue hypoxia is defined as pO2< 40mmHg in non-diabetic patients and as pO2< 50mmHg in diabetic patients. It refers to circulation malfunctioning and poor outcomes in healing process supported by HBOT.
Assessment with photographic documentation eases comparison [11-13] in vision (wavelength 380-790nm), ultraviolet (100-400nm) and infrared (780nm-1mm) light. Fluorescence imaging with ultraviolet light can detect bacteria species producing porphyrins or pyoverdins like Staphylococcus aureus, Pseudomonas aeruginosa, β-hemolytic Streptococci group B. Produced by mentioned above species porphyrins fluorescence as red light, pyoverdins fluorescence as cyan light, while skin collagen fluorescence as green light [14]. According to reports ultraviolet light penetrating less skin layers, indicated wound-healing process and wounds already healed [15,16].
Infrared light indicates areas with higher temperature what refers to well-perfused tissues and vessels functioning, what eases vascular assessment. Sowa et al. [17] underlines the usefulness of infrared light as a technology to observe healing process to optimize the outcomes of the therapy.
Methods
Three-dimensional scans were performed with Artec Eva Light hand scanner, which utilizes white light irradiation, considered safe for most individuals (except epileptics) and video camera triangulation. This highly precise device, designed for various applications, including medical uses, enables measurements with a maximum accuracy of 0.1mm, leading to the creation of highquality 3D models. The accuracy of the device was validated before conducting measurements on the patients and it exceeded 99.27%. Each patient has signed informed consent for using wound pictures with anonymized data. The final body model was generated through a series of graphic processing methods applied to the collected images employing the dedicated Artec Studio 11 Professional software. The calculations of wound surface and volume has been done with differential method. However, total volume and surface of each wound has been calculated basing on tissue models created from obtained scans. Then the wound is being cut from the model by filling the cavity and completing the surface. The final result is a subtraction of volume and surface area of the model with and without the wound. Described method has its limitations as in patients with amputated limbs, wound mapping is difficult due to lack of reference. The second method of analyzing the collected data involved direct distance measurements in an appropriately scaled model using the Autodesk Mesh-mixer software.
Patient 1 Presentation
A 48-year-old male reported to Outpatient Clinic in National Centre of Hyperbaric Medicine with chronic wound of his left foreleg. Undergoing hematologic treatment because of II factor hyperactivity, no other comorbidities. In 2021 he suffered a deep wound caused by impact of concrete element during housework. Since that time, the wound did not heal despite local treatment with specialist dressings. On 13th July 2023 he was consulted in our outpatient clinic, the limb was reddened due to inflammatory reaction on half of its length. The skin was dry and exfoliating, the wound itself looked like a deep crater covered with necrotic tissues inside.
After being referred to the surgeon, he got back after debridement for re-consultation. The patient was qualified for hyperbaric oxygen therapy consisting of 30 sessions (2.5 ATA. 100% oxygen plus air breaks). The wound was documented with three-dimensional scanner and images in ultraviolet and infrared light (Table 1).
Table 1:presenting wound photographs before (A) and after (B) the treatment in multifrequency light.
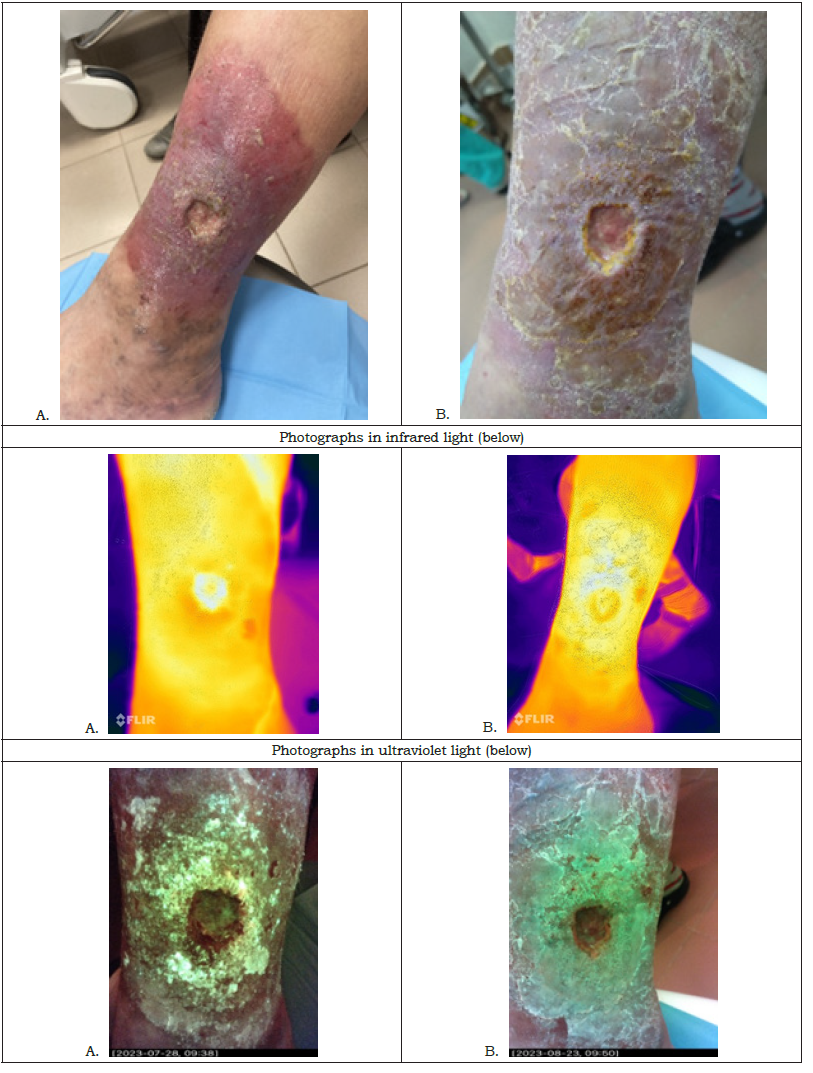
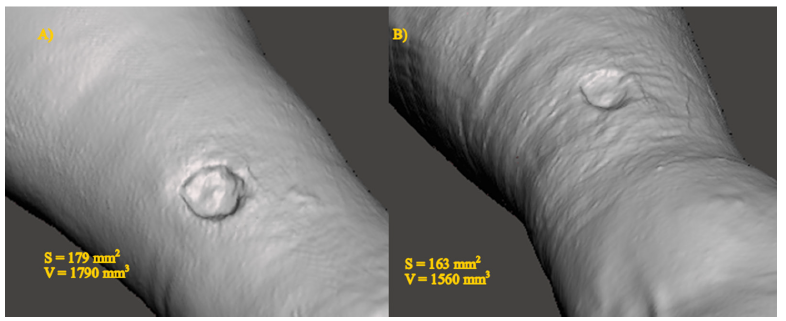
3D scans performed with Artec Eva Light hand scanner measured wound surface. The measurements showed limb swelling (right foreleg circumference 287,47mm compared to left foreleg circumference 271,13mm). Moreover, thanks to the scans, exact dimensions of the wound were available and made easier comparison in aim to assess effect of hyperbaric oxygen therapy (Chart 1).
Chart 1:MRI findings of the right shoulder (January 2024).
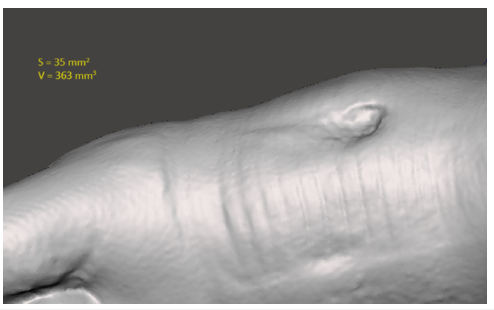
Results of transcutaneous oximetry showed pO2 60 mmHg with an increase during HBOT to 1150mmHg, what proves satisfying tissue response to hyperoxia and relates to high-healing potential (Chart 2,3). First data taken on 28th July 2023 at the begging of hyperbaric oxygen therapy documented primary wound dimensions. After almost one moth of HBOT we documented again patient’s wound. The results showed that wound length and its surface are reduced. The wound surface reduced by 5.6%, while the wound volume decreased by 12,8%. However, basing just on macroscopic assessment, we made a conclusion that insignificant difference is noticeable.
Chart 2:(TcPO2- transcutaneous pO2 [mmHg]; time [min]; TCOM 1- electrode near the wound, TCOM 2- reference electrode placed in subclavian area).
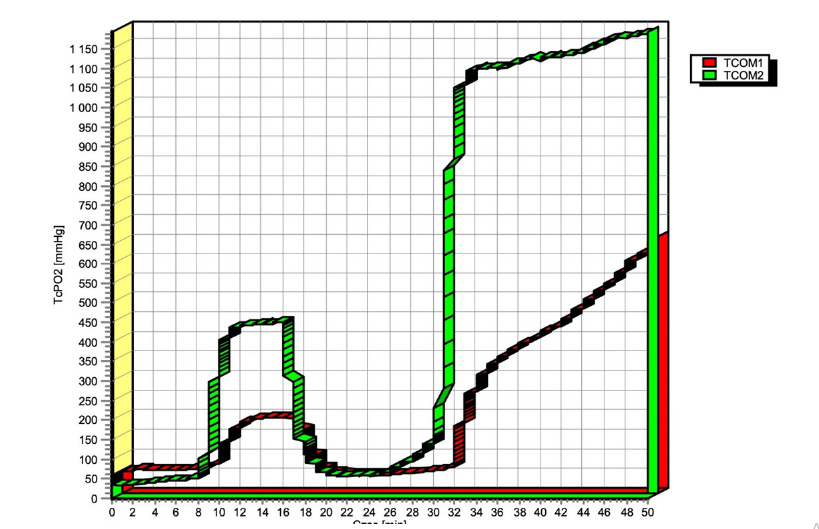
Chart 3:Wound mapping before (A) and after HBOT (B). S- surface, V- volume.
Patient 2 Presentation
A 55-year-old woman reported to our clinic on December 2023 with left foot phlegmon after surgical treatment. Her main comorbidity is good, controlled diabetes mellitus type 1 that was diagnosed 25 years ago. In July 2023 due to left foot swelling and redness she had a surgeon consultation. In diagnostic imaging Charcot’s foot was described as an effect of neuropathic changes in soft tissues, small joints articular surface destruction localized mainly in tarsometatarsal joint. Despite conservative treatment, she suffered from phlegmon that was surgically incised and underwent targeted antibiotic therapy. As the wound did not heal, she was referred for hyperbaric consultation. The wound was estimated with the size 4x2cm located on the medial part of left forefoot; no necrotizing tissues observed. The patient used dedicated dressings including silver dressings. During first consultation photographic documentation was done (Table 2).
Table 2:presenting wound photographs before the treatment in multifrequency light.
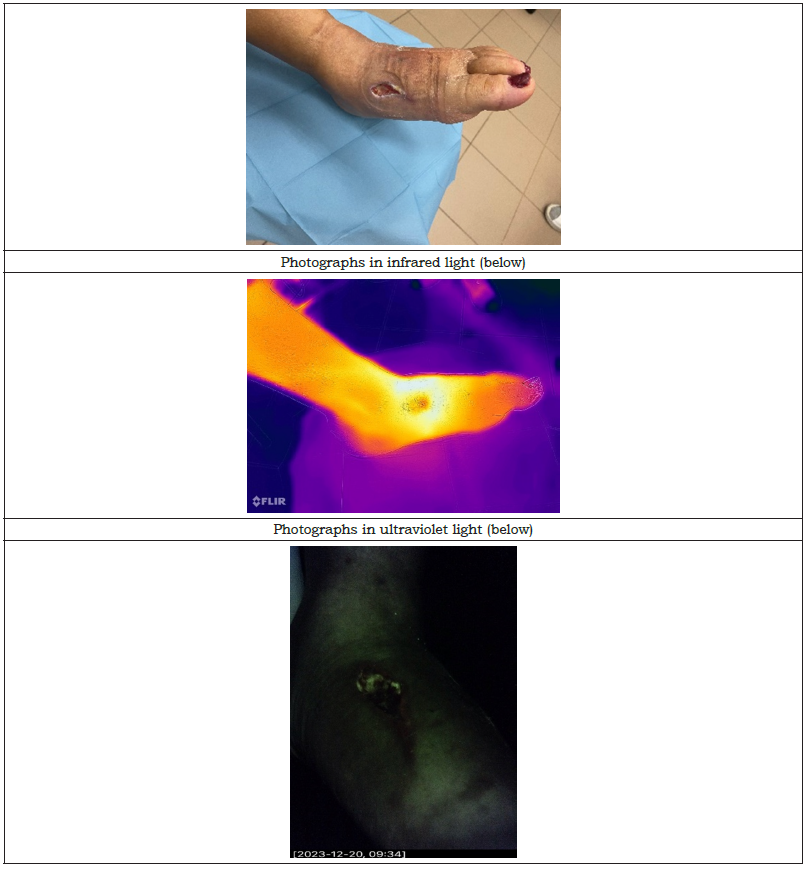
The patient was primarily qualified to 30 sessions of HBOT (2.5 ATA, 100% oxygen, 60 minutes plus air breaks). Also, we assessed transcutaneous oxygen measurements that showed local pO2 69mmHg with an increase to 950mmHg, what relates to satisfying tissue response to HBOT (Chart 4). However, after having completed 14 sessions, the patient resigned due to satisfying healing acceleration.
Chart 4:Patient’s transcutaneous oximetry result. (TcPO2- transcutaneous pO2 [mmHg]; time [min]; TCOM 1- electrode near the wound, TCOM 2- reference electrode placed in subclavian area).

After HBOT, the wound had smaller size, was shallow with ongoing healing process. After 3 months we received photographs from the patient showing therapeutic success as the wound has been completely closed as final stage of healing process. The patient was not able to come for check-up to our outpatient clinic due to private reasons. However, according to her relation and delivered photography, outcomes in reference to wound healed are successful.
Discussion
Comparing wound images in vision, infrared and ultraviolet light we are able to more precisely assess healing process. As non-invasive, easily available and painless for the patient method could be used in regular wound treatment assessment. Quick and comparable results could also make therapeutic decision more accurate leading to quicker recovery. According to increasing life expectancy, ageing society with more and more comorbidities leading directly to skin lesions, chronic wounds lead to life quality lowering. More research is needed to assess usefulness of planimetry and different types of imaging [18] in outpatient clinic practice as it may bring us a new look in the future of chronic wound management.
Conclusion
Non-healing wound management needs a holistic treatment including reversible causes elimination, surgery, antibiotics if needed and in some cases hyperbaric oxygen therapy. Effects cannot be assessed immediately due to prolonged process of healing. In visible light we can see macroscopic changes, but without capturing wound images in medical documentation comparisons and conclusions may be challenging. Infrared light showing different temperature areas translated into circulation quality that is crucial for anti-inflammatory processes in wound-healing [19,20]. Undoubtedly, medical technologies development seems to be the future of improving outcomes assessment. Particularly in non-healing wounds that diminish patients’ life quality and life expectancy. Multimodal treatment is necessary as together with advanced technology, we can reduce human factors influencing non-healing wounds therapy.
References
- Sen CK (2021) Human wound and its burden: Updated 2020 compendium of estimates. Adv Wound Care 10(5): 281-292.
- Gould L, Abadir P, Brem H, Carter M, Conner-Kerr T, et al. (2015) Chronic wound repair and healing in older adults: Current status and future research. J Am Geriatr Soc 63(3): 427-438.
- Armstrong DG, Swerdlow MA, Armstrong AA, Conte MS, Padula WV, et al. (2020) Five-year mortality and direct costs of care for people with diabetic foot complications are comparable to cancer. J Foot Ankle Res 13(1): 16.
- Catella J, Long A, Mazzolai L (2021) What Is currently the role of TcPO2 in the choice of the amputation level of lower limbs? A comprehensive review. J Clin Med 10(7): 1413.
- Mayrovitz HN, Soontupe LB (2009) Wound areas by computerized planimetry of digital images: Accuracy and reliability. Adv Skin Wound Care 22(5): 222-229.
- Fuller FW, Mansour EH, Engler PE, Shuster B (1985) The use of planimetry for calculating the surface area of a burn wound. J Burn Care Rehabil 6(1): 47-49.
- Foltynski P, Ladyzynski P (2022) Digital planimetry with a new adaptive calibration procedure results in accurate and precise wound area measurement at curved surfaces. J Diabetes Sci Technol 16(1): 128-136.
- Foltynski P, Ladyzynski P, Ciechanowska A, Migalska-Musial K, Judzewicz G, et al. (2015) Wound area measurement with digital planimetry: Improved accuracy and precision with calibration based on 2 rulers. PLoS One 10(8): e0134622.
- Trinks TP, Blake DF, Young DA, Thistlethwaite K, Vangaveti VN (2017) Transcutaneous oximetry measurements of the leg: Comparing different measuring equipment and establishing values in healthy young adults. Diving Hyperb Med 47(2): 82-87.
- Kmiec MM, Hou H, Lakshmi Kuppusamy M, Drews TM, Prabhat AM, et al. (2019) Transcutaneous oxygen measurement in humans using a paramagnetic skin adhesive film. Magn Reson Med 81(2): 781-794.
- Williams KJ, Sounderajah V, Dharmarajah B, Thapar A, Davies AH (2017) Simulated wound assessment using digital planimetry versus three-dimensional cameras: Implications for clinical assessment. Ann Vasc Surg 41: 235-240.
- Bohannon RW, Pfaller BA (1983) Documentation of wound surface area from tracings of wound perimeters. Clinical report on three techniques. Phys Ther 63(10):1622-1624.
- Li S, Mohamedi AH, Senkowsky J, Nair A, Tang L (2020) Imaging in chronic wound diagnostics. Adv Wound Care 9(5): 245-263.
- DaCosta RS, Kulbatski I, Lindvere-Teene L, Starr D, Blackmore K, et al. (2015) Point-of-Care autofluorescence imaging for real-time sampling and treatment guidance of bioburden in chronic wounds: First-in-Human results. PLoS One 10(3): e0116623.
- Radowsky JS, Neely R, Forsberg JA, Lisboa FA, Dente CJ, et al. (2018) Preclosure spectroscopic differences between healed and dehisced traumatic wounds. PLoS One 13(9): e0204453.
- West M, Barsley RE, Frair J, Stewart W (1992) Ultraviolet radiation and its role in wound pattern documentation. J Forensic Sci 37(6): 1466-1479.
- Sowa MG, Kuo WC, Ko ACT, Armstrong DG (2016) Review of near-infrared methods for wound assessment. J Biomed Opt 21(9): 091304.
- Moller F, Hoffmann U, Dalecki M, Drager T, Doppelmayr M, et al. (2021) Physical exercise intensity during submersion selectively affects executive functions. Hum Factors 63(2): 227-239.
- Mota Rojas D, Ogi A, Villanueva-García D, Hernández-Ávalos I, Casas-Alvarado A, et al. (2024) Thermal imaging as a method to indirectly assess peripheral vascular integrity and tissue viability in veterinary medicine: Animal models and clinical applications. Animals 14(1): 142.
- Li WW, Carter MJ, Mashiach E, Guthrie SD (2017) Vascular assessment of wound healing: A clinical review. Int Wound J 14(3): 460-469.
© 2024 Rita I Sharma. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 





.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






