- Submissions

Full Text
Advancements in Case Studies
Stent Embolization
Kourtis Konstantinos* , Christou Apostolos, Kollokas Aggelos and Patsilinakos Sotirios
Cardiology Department, Konstantopoulio General Hospital, Greece
*Corresponding author:Konstantinos T Kourtis, Cardiology Department, Konstantopoulio General Hospital, Nea Ionia, Athens, Greece
Submission:January 18, 2024;Published: February 06, 2024

ISSN 2639-0531Volume4 Issue2
Abstract
Although the number of PCI procedures has significantly increased over the years, the severe complications are rare. Stent embolization is a rare complication of coronary stenting, at a rate of 0.2%. We report on a case with a 64-year-old man admitted to the emergency department with unstable angina and stent embolization during the coronary angiography and successful retrieval of a coronary stent from the left anterior descending (LAD) artery, which migrated to the left popliteal artery. The stent was finally removed surgically.
Keywords:Stent embolization; Coronary complication; Popliteal artery
Introduction
Although the number of PCI procedures has significantly increased over the years, the incidence of stent loss has decreased and remains at a rate of 0.2%, as a result to the greater experience of interventional cardiologists and improvements in equipment, especially due to utilization of pre-mounted stents [1,2]. Systemic and coronary embolization’s are the consequences of stent dislodgement and can lead to serious complications such as acute closure of the affected vessel, coronary thrombosis and subsequent myocardial infarction.
Case Report
A 64-year-old man admitted to the emergency department with unstable angina. Symptoms begun 4 hours later and lasted for 30 minutes, but there was no chest pain at the time of admission. Resting ECG showed T inversion in the precordial leads but there was no rise in cardiac troponin serum levels. His coronary risk factors include dyslipidaemia and smoking. Next day the patient was taken to the cardiac catheterization laboratory. Coronary angiography revealed a long, heavily calcified lesion in the mid-left anterior descending (LAD) artery.
After an initial balloon dilatation, a 2nd generation drug eluting stent (Nobori 3x30 mm) was delivered to the LAD. Guideliner mother and child technique was used. The attempt to pass through the stenosis was failed and the stent was dislodged from its delivery balloon. The delivery balloon was drawn back without the stent, which moved to the left main (LM) coronary artery. Another balloon (2x10mm) was delivered distally through the stent, which inflated up to 2 atm. The stent could not be withdrawn into the guide catheter, probably due to stent malformation (damage). So, we decided to try “en block” retrieval of the inflated balloon, the dislodged stent, the guide wire and the catheter as far as the common femoral artery. Unfortunately, the stent could not insert into the lumen of the sheath in the femoral artery, so it was released in the peripheral circulation. Fluoroscopy revealed that it was migrated to the left popliteal artery.
The patient was stable during the procedure, without chest pain and without signs of limb ischemia. The PCI attempt was abandoned and a decision for CABG was taken. During the CABG procedure the stent from the left popliteal artery was removed surgically (Figures 1-3). Close examination of the removed stent revealed disruption and malformation, which could explain the difficulty encountered while attempting to retrieve it into the guide catheter or into the femoral artery sheath (Figure 4).
Figure 1:
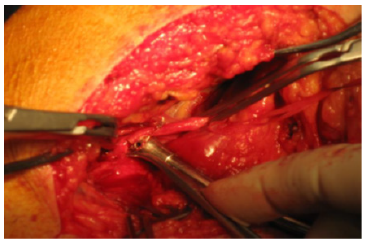
Figure 2:
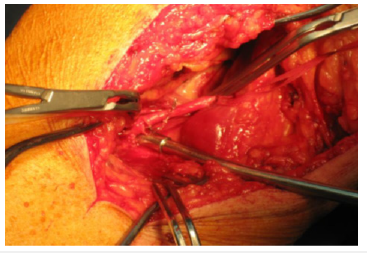
Figure 3:

Figure 4:

Discussion
Stent loss and its migration is a rare complication of coronary stenting, probably due to advances in equipment design and worldwide utilization of pre-mounted stents. However, anatomical circumstances, such as arterial tortuosity in the location proximal to the lesion and significant calcification of the lesion, increase the frequency stent dislodgement and embolization [1]. It is wellknown that direct stenting may be associated with a higher risk of this complication, presumably due to the increased resistance to stent advancement through the lesion, but in our case an initial balloon dilatation was performed. Angulated coronary arteries may also cause difficulties during stent procedures [3,4]. In this specific case, the calcification of the lesion was the main determinant, which was responsible for the stent dislodgement.
Nonsurgical removal or peripheral deployment is the best option for this complication, but surgery may be indicated if percutaneous retrieval attempts fail [5]. Different percutaneous retrieval techniques have been described to retrieve embolized stents from the coronary system and the peripheral circulation. Low-profile angioplasty balloon catheters, loop snare biliary forceps, twirling two wires around the stent, cook retained fragment retriever and basket retrieval devices have been successfully used [1].
In our case the first care was to withdraw the stent from the LM artery and to avoid embolization to the cerebral circulation. Snare loop is often the device of first choice due to its effectiveness and safety [6]. However, there was no snare loop available in our department in order to use it for the retrieval of the stent. The use of low-profile balloon catheters was an alternative choice, which is also very effective, especially in this case where the stent was still riding on the guide wire and was deployed enough to advance a balloon catheter through its lumen. Unfortunately, the stent was lost and migrated with the blood stream to the left popliteal artery. There are many reports of stent embolization and successfully percutaneous retrieval from peripheral vessels, such as from renal artery, pedal artery or abdominal aorta [7-9]. However, in our case the non-surgical retrieval from the left popliteal artery was impossible, because the stent was already damaged and it has been migrated far enough below the aortoiliac bifurcation.
References
- Donini LM, Marsili D, Graziani MP, Imbriale M, Cannella C (2004) Orthorexia nervosa: A preliminary study with proposal for diagnosis and attempt to measure the dimension of the phenomenon. Eat Weight Disord 9(2): 151-157.
- Dunn TM, Bratman S (2016) On orthorexia nervosa: A review of literature and proposed diagnostic criteria. Eat Behav 21: 11-17.
- Stochel M, Janas-Kozik M, Zejda JE, Hyrnik J, Jelonek I, et al. (2015) Validation of the ORTO-15 questionnaire in a group of urban youth aged 15-21. Psychiatrist Pol 49(1): 119-134.
- Clifford T, Blyth C (2019) A pilot study comparing the prevalence of orthorexia nervosa in regular students and those in university sports teams. Eat Weight Disord 24(3): 473-480.
- Łucka I, Janikowska-Hołoweńko D, Domarecki P, Plenikowska-Ślusarz T, Domarecka M (2019) Orthorexia nervosa-a separate clinical entity, a part of eating disorder spectrum or another manifestation of obsessive-compulsive disorder? Psychiatr Pol 53(2): 371-382.
- Łucka I, Janikowska HD, Domarecki P, Plenikowska ŚT, Domarecka M (2019) The prevalence and risk factors of orthorexia nervosa among school-age youth of Pomeranian and warmian-masurian voivodeships. Psychiatr Pol 53(2): 383-398.
- Segura-Garcia C, Ramacciotti C, Rania M, Aloi M, Caroleo M, et al. (2015) The prevalence of orthorexia nervosa among eating disorder patients after treatment. Eat. Weight Disord 20(2): 161-166.
- Segura-Garzia C, Papaianni MC, Caglioti F, Procopio L, Nistico CG, et al. (2012) Orthorexia nervosa: A frequent eating disordered behavior in athletes. Eat Weight Disord 17(4): e226-233.
- Gramaglia C, Brytek-Matera A, Rogoza R, Zeppegno P (2017) Orthorexia and anorexia nervosa: Two distinct phenomena? A cross-cultural comparison of orthorexic behaviors in clinical and non-clinical samples. BMC Psychiatry 17(1): 75.
- Parra-Fernandez ML, Rodriguez-Cano T, Perez-Haro MJ, Onieva-Zafra MD, Fernandez-Martinez E, et al. (2018) Structural validation of ORTO-11-ES for diagnosis of orthorexia nervosa, Spanish version. Eat Weight Disord 23(6): 745-752.
- Domingues RB, Carmo C (2021) Orthorexia nervosa in yoga practitioners: Relationship with personality, attitudes about appearance, and yoga engagement. Eat Weight Disord 26(3): 789-795.
- Barnes MA, Caltabiano ML (2017) The interrelationship between orthorexia nervosa, perfectionism, body image and attachment style. Eat Weight Disord 22(1): 177-184.
- Kiss-Leizer M, Rigó A (2019) People behind unhealthy obsession to healthy food: The personality profile of tendency to orthorexia nervosa. Eat Weight Disord 24(1): 29-35.
- Jayson J, Nassim Tabri (2022) The association of perfectionism, health-focused self-concept and erroneous beliefs with orthorexia nervosa symptoms: A moderated mediation model. International Journal of Eating Disorders 55(7): 892-901.
- Noebel NA, Oberle CD, Marcell HS (2022) Orthorexia nervosa and executive dysfunction: Symptomatology is related to difficulties with behavioural regulation. Eating and Weight Disorders 27(6): 2019-2026.
- Eriksson L, Baigi A, Marklund B, Lindgren EC (2008) Social physique anxiety and sociocultural attitudes toward appearance impact on orthorexia test in fitness participants. Scan J Med Sci Sports 18(3): 389-394.
- Costanzo G, Marchetti D, Manna G, Verrocchio MC, Falgares G (2022) The role of eating disorders features, psychopathology, and defence mechanisms in the comprehension of orthorexic tendencies. Eating and Weight Disorders 27(7): 2713-2724.
- Kinzl JF, Hauer K, Traweger C, Kiefer I (2006) Orthorexia nervosa in dieticians. Psychother Psychosom 75(6): 395-396.
- Mutluer G, Yilmaz D (2023) Relationship between healthy eating fixation (Orthorexia) and past family life and eating attitudes in young adults. American Journal of Health Education 54(2): 155-167.
- Lasson C, Raynal P (2021) Personality profiles in young adults with orthorexic eating behaviours. Eating and Weight Disorders 26(8): 2727-2736.
- Barnes MA, Caltabiano ML (2017) The interrelationship between orthorexia nervosa, perfectionism, body image and attachment style. Eat Weight Disord 22(1): 177-184.
- Vuillier L, Robertson S, Greville-Harris M (2020) Orthorexic tendencies are linked with difficulties with emotion identification and regulation. J Eat Disor 8: 15.
- Reynolds R (2018) Is the prevalence of orthorexia nervosa in an Australian university population 6.5%? Eat Weight Disord 23(4): 453-458.
- Brytek-Matera A, Fonte ML, Poggiogalle E, Donini LM, Hellas C (2017) Orthorexia nervosa: Relationship with obsessive-compulsive symptoms, disordered eating patterns and body uneasiness among Italian university students. Eat Weight Disorders 22(4): 609-617.
- Duran S, Çiçekoğlu P (2020) Relationship between orthorexia nervosa, muscle dysmorphic disorder (bigorexia), and self-confidence levels in male students. Perspectives in Psychiatric Care 56(4): 878-884.
- Messer M, Liu C, McClure Z, Mode J, Tiffin C, et al. (2022) Negative body image components as risk factors for orthorexia nervosa: Prospective findings. Appetite 178: 106280.
- Sfeir M, Malaeb D, Obeid S, Hallit S (2022) Association between religiosity and orthorexia nervosa with the mediating role of self-esteem among a sample of the Lebanese population-short communication. Journal of Eating Disorders 10(1): 151.
- Eriksson L, Baigi A, Marklund B, Lindgren EC (2008) Social physique anxiety and sociocultural attitudes toward appearance impact on orthorexia test in fitness participants. Scan J Med Sci Sports 18(3): 389-394.
- Rudolph S (2018) The connection between exercise addiction and orthorexia nervosa in German fitness sports. Eat Weight Disord 23(5): 581-586.
- Clifford T, Blyth C (2019) A pilot study comparing the prevalence of orthorexia nervosa in regular students and those in University sports teams. Eat Weight Disord 24(3): 473-480.
- Valera JH, Acuña Ruiz P, Valdespino BR, Visioli F (2014) Prevalence of orthorexia nervosa among ashtanga yoga practitioners: A pilot study. Eat Weight Disord 19(4): 469-472.
- Bóna E, Szél Z, Kiss D, Gyarmathy VA (2019) An unhealthy health behaviour: Analysis of orthorexic tendencies among Hungarian gym attendees. Eat Weight Disord 24(1): 13-20.
- Dittfeld A, Gwizdek K, Jagielski P, Brzęk A, Ziora K (2017) Evaluation of the relationship between orthorexia and vegetarianism with use BOT (Bratman Test for Orthorexia). Psychiatr Pol 51(6):1133-1144.
- Guglielmetti M, Ferraro OE, Gorrasi ISR, Carraro E, Bo S, et al. (2022) Lifestyle-related risk factors of orthorexia can differ among the students of distinct university courses. Nutrients 14(5): 1111.
- Voglino G, Bert F, Parente B, Lo Moro G (2020) Orthorexia nervosa, a challenging evaluation: Analysis of a sample of customers from organic food stores. Psychology Health and Medicine 26(3): 1-9.
- Dell Osso L, Carpita B, Muti D, Cremone IM, Massimetti G, et al. (2018) Prevalence and characteristics of orthorexia nervosa in a sample of university students in Italy. Eat. Weight Disord 23(1): 55-65.
- Kalika E, Egan H, Mantzios M (2022) Exploring the role of mindful eating and self-compassion on eating behaviours and orthorexia in people following a vegan diet. Eat Weight Disord 27(7): 2641-2651.
- Miley M, Egan H, Wallis D, Mantzios M (2022) Orthorexia nervosa, mindful eating, and perfectionism: An exploratory investigation. Eat Weight Disord 27(7): 2869-2878.
- Bundros J, Clifford D, Silliman K, Neyman Morris M (2016) Prevalence of orthorexia nervosa among college students based on Bratman's test and associated tendencies. Appetite 101: 86-94.
- Plichta M, Jezewska-Zychowicz M, Gębski J (2019) Orthorexic tendency in Polish students: Exploring association with dietary patterns, body satisfaction and weight. Nutrients 11(1): 100.
- Dell’Osso L, Abelli M, Carpita B, Pini S, Castellini G, et al. (2016) Historical evolution of the concept of anorexia nervosa and relationship with orthorexia nervosa, autism, and obsessive-compulsive spectrum. Neuropsychiatr Dis Treat 12: 1651-1660.
- Karniej P, Pérez J, Vela RJ, Arnedo IS, Caballero VG, et al. (2023) Orthorexia nervosa in gay men-the result of Spanish polish eating disorders study. BMC Public Health 23: 58.
- Dittfeld A, Gwizdek K, Koszowska A, Nowak J, Puzoń AB, et al. (2016) Assessing the risk of orthorexia in dietetic and physiotherapy students using the BOT (Bratman Test for Orthorexia). Pediatr Endocrinol Diabetes Metabol 22(1): 6-14.
- King E, Wengreen H (2023) Associations between level of interest in nutrition, knowledge of nutrition, and prevalence of orthorexia traits among undergraduate students. Nutr Health 29(1): 149-155.
- Aktürk U, Gül E, Erci B (2019) The effect of orthorexia nervosa levels of nursing students and diet behaviors and socio-demographic characteristics. Ecol Food 58(4): 397-409.
- Bo S, Zoccali R, Ponzo V, Soldati L, Carli LD, et al. (2014) University courses, eating problems and muscle dysmorphia: Are there any associations? J Transl Med 12: 221.
- Erkin Ö, Kocaçal E (2022) Health perceptions and orthorexia nervosa tendencies among academics. Perspect Psychiatr Care 58(4): 2782-2790.
- Aksoydan E, Camci N (2009) Prevalence of orthorexia nervosa among Turkish performance artists. Eat Weight Disord 14(1): 33-37.
- Turner PG, Lefevre CE (2017) Instagram use is linked to increased symptoms of orthorexia nervosa. Eat Weight Disord 22(2): 277-284.
- Villa M, Opawsky N, Manriquez S, Ananias N, Rodriguez ML, et al. (2022) Orthorexia nervosa risk and associated factors among Chilean nutrition students: A pilot study. J Eat Disord 10(1): 6.
- Yılmaze G (2021) Orthorexia tendency and social media addiction among candidate doctors and nurses. Perspect Psychiatr Care 57(4): 1846-1852.
- Valente M, Renckens S, Aelen JB, Syurina EV (2022) The #orthorexia community on Instagram. Eating and Weight Disorders - Studies on Anorexia, Bulimia and Obesity 27: 473-482.
- Sanlier N, Yassibas E, Bilici S, Sahin G, Celik B (2016) Does the rise in eating disorders lead to increasing risk of orthorexia nervosa? Correlations with gender, education, and body mass index. Ecol Food Nutr 55(3): 266-278.
- Martins IJ (2017) Single gene inactivation with implications to diabetes and multiple organ dysfunction syndrome. J Clin Epigenet 3(3): 24.
- Martins IJ (2016) Anti-aging genes improve appetite regulation and reverse cell senescence and apoptosis in global populations. Advances in Aging Research 5(1): 9-26.
- Martins IJ (2018) Sirtuin 1, a diagnostic protein marker and its relevance to chronic disease and therapeutic drug interventions. EC Pharmacology and Toxicology 6(4): 209-215.
- Strahler J, Hermann A, Walter B, Stark R (2018) Orthorexia nervosa: A behavioral complex or a psychological condition? J Behav Addict 7(4): 1143-1156.
© 2023 Izabela Łucka. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 





.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






