- Submissions

Full Text
Advancements in Case Studies
Prevalence and Characteristics of Orthorexia Nervosa in a Sample of University Students in Poland
Izabela Łucka1* and Anna Łucka2
1Department of Developmental Psychiatry, Psychotic Disorders and Old Age Psychiatry, Medical University of Gdansk, Poland
2Faculty of Law and Administration, University of Gdansk, Poland
*Corresponding author:Izabela Łucka, Department of Developmental Psychiatry, Psychotic Disorders and Old Age Psychiatry, Medical University of Gdansk, Poland
Submission:August 14, 2023;Published: August 23, 2023

ISSN 2639-0531Volume4 Issue1
Abstract
Aim: The aim of the study was to determine the prevalence of orthorexia nervosa (ON) among young
adults from Poland as well as search for factors which enhance the risk of orthorexia nervosa.
Material and Method: The study group consisted of 136 subjects (95 females, 3 non-binary and 38 males).
The mean age of female participants was 20.21+/-3.27 years, and of male participants–18.93+/-3.67
years. In the study, we used a proprietary questionnaire to collect patient data, as well as following
diagnostic questionnaires: ORTO-15 by Donini et al. (score of 35 was considered as cut-off point) and
EAT-26 by Garner and Garfinkel. The results were statistically analyzed.
Results: Among the overall surveyed respondents, the proportion of those found to be at risk for orthorexia
was 26.5% (36 subjects). Eating disorders were found in a total of 15.4% (21) of the respondents. The
risk of orthorexia occurred significantly more often in those who had an eating disorder, 71.4% (15), than
in those who did not, 18.3% (21). A statistically significant association was found between the presence
of an eating disorder and the occurrence of orthorexia risk (chi square=25.790 p <0.001). Depression
was present (according to respondents’ self-assessment and evaluation) in 57.3% (78) of respondents
or their families. The highest score of risk was observed in the group of students when the respondent
experienced depression. A statistically significant association was found between the presence of
depression and the occurrence of orthorexia risk (chi square=3.924 p =0.048). There were no statistically
significant differences in the risk of orthorexia in groups from big cities and small towns. The studied
social factors did not show impact on the risk of orthorexia as well as gender and BMI.
Conclusion: The prevalence of orthorexia nervosa (ON) among young adults from Poland was 26%.
A statistically significant association was found between the presence of eating disorders and the risk
of orthorexia, confirming that ON is most likely a slightly different clinical manifestation of the eating
disorder. The respondent’s depressive disorders were the only statistically significant factor increasing
the risk of orthorexia.
Keywords:Orthorexia; Eating disorders; Prevalence; Young adults
Introduction
Eating disorders have risen to become a major concern of our time, we are observing an increasing number of people struggling with complications arising from poor nutrition. As the role of food is not only to satisfy hunger by providing the right amount of calories required, but also to regulate emotions and communicate in social relationships-we are witnessing significantly more people with underweight, obesity and other eating disorders - such as a pathological fixation on healthy eating, first named and described by S. Bratman in 1997 as orthorexia [1,2]. The underlying causes of eating problems lie in substantial disturbances in self-perception, as well as in pursuit of unrealistic goals for one’s body image, self-imposed strict dieting leading eventually to changes in the functioning of the appetite regulating mechanisms and cachexia. From psychodynamic and developmental perspectives, maladaptive patterns of resolving internal conflict as well as the hardships of the separation and individualization process accompanying adolescence are particularly relevant factors in eating disorders. Rather than resolving the aforementioned issues in interpersonal relationships they are “ shifted to food and the body.” These problems are usually the result of disruptions in early childhood relationships with primary attachment objects-the relationship with the mother, as the primary nurturing object, plays a special role. The importance of this very relationship and the early childhood pattern of it, linked to the feeding relationship, is an essential determinant in the life of a particular person for the development of later dysfunctions in self-perception and approaches to food and eating [7-11].
Occasionally, a significant factor sustaining eating disorders consists of undisclosed problems of the family or individual family members, such as bereavement, addictions, crisis in the parental relationship, thus the symptoms of eating disorders perform an adaptive function and protect the family from confronting situations that are challenging to resolve. Typically, eating disorders cluster all the family’s problems as if through a lens, with no proper understanding and support given not only to the person delegated by the system to the role of patient but also to the entire family, treatment becomes very troublesome and ineffective. Relying on both the theoretical basis for understanding eating disorders and clinical experience, the authors of the study attempted to estimate the prevalence of orthorexia, its affiliation with eating disorders, and an analysis of factors that could increase its risk.
Material and Method
The study group consisted of 136 subjects (95 females, 3 nonbinary persons and 38 males). The mean age of female participants was 20.21+/-3.27 years, and of male participants–18.93+/-3.67 years. In the study, we used a proprietary questionnaire to collect patient data, as well as following diagnostic questionnaires: ORTO- 15 by Donini et al. [12] (score of 35 was considered as cut-off point) and EAT-26 by Garner and Garfinkel. We believe that for more effective diagnosis it would be advisable to adopt a cut-off point for orthorexia in the ORTO-15 at the level of 35 points, as postulated in prior study as well as by other researchers due to the cut-off point suggested by the author of the questionnaire artificially inflates the results (threshold is associated with considerable overdiagnosis of the phenomenon). We believe so based on our previous studies and the observations of other researchers [2-5]. The survey was conducted online, respondents completed it voluntarily, and received no compensation for their time. The data were statistically analyzed.
Statistical methods
Describing the normality of quantitative characteristics, the arithmetic mean was used to assess the average level and the standard deviation was used to assess dispersion. Verification of the hypothesis of normality of the distribution of the studied variables was carried out with the W Shapiro-Wilk test. For comparisons of the level of the studied variables between groups, due to the lack of normality of the distribution of the variables, the non-parametric Mann-Withney U test (for two variables) and the Kruskal-Wallis test (for comparisons of three variables) were used. Structure indices were used to show the regularity of qualitative data (categorized characteristics), and chi-square independence was used to compare distributions and assess relationships between variables. Correlation intensity was assessed using Spearman’s rho correlation coefficient. The odds ratio (OR) was used along with a 95% confidence interval to assess how far greater or lesser the chance of orthorexia risk is in one group compared to another group. In all statistical tests, p≤0.05 was taken as the level of statistical significance. Statistical analysis was performed using IBM SPSS Statistics vs.27 and Statistica 13.1.
Results
Orthorexia nervosa and eating disorders are heavily intertwined, this provides evidence that ON belongs to the spectrum of eating disorders, it is only distinguished by a specific manifestation in terms of clinical symptoms.
Risk: Orthorexia vs. eating disorders
We examined whether there was an association between the
risk of orthorexia (ORT-15 scale) and the
presence of eating disorders (EAT-26 scale). The results are
shown in Table 1.
Table 1:Risk of orthorexia vs. onset of eating disorders.
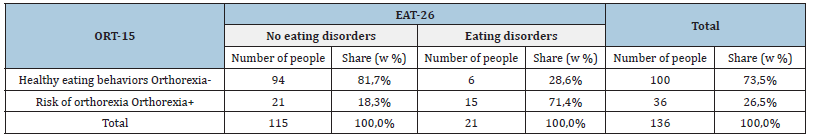
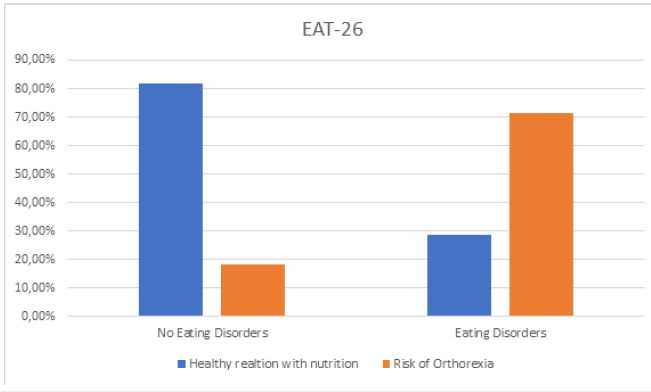
Among the overall respondents, the proportion of those identified as being at risk for orthorexia was 26.5% (36 people). Eating disorders were observed in a total of 15.4% (21) of the respondents. The risk of orthorexia occurred significantly more frequently in those who had an eating disorder, 71.4% (15), than in those who did not, 18.3% (21). A statistically significant association was found between the presence of an eating disorder and the risk of orthorexia (chi square=25.790 p<0.001). Using the odds ratio, it was determined what is the likelihood of occurrence of the risk of orthorexia in those diagnosed with an eating disorder. The obtained result OR [95% CI] =11,190[3,883;32,247] indicates that the chance of occurrence of the orthorexia in the group with an eating disorder is over 11 times higher than in the group without an eating disorder. In addition, a statistically significant correlation was found between the EAT-26 and ORT-15 scores (Spearman’s rho=- 0.482 p<0.001), the higher the EAT-26 score, the lower the ORT-15 score on average, that is, the higher the level of eating disorder, the higher the risk of orthorexia on average (Chart 1).
Chart 1:Risk of orthorexia vs. occurrence of eating disorders.
Risk: Orthorexia vs. studying health sciences An attempt was made to investigate whether health sciences students are more likely to have orthorexia; unfortunately, it was not possible to collect a sufficiently large group; survey replies were made by respondents from both medical, technical and humanities universities, as well as those with no university education.
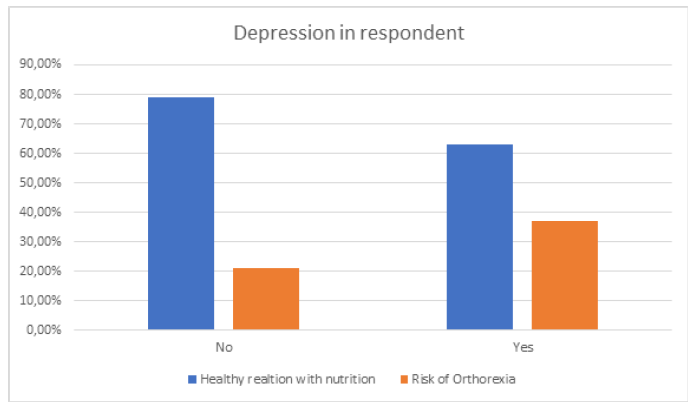
Risk: orthorexia vs. depression We examined whether there was an association between the risk of orthorexia (ORT-15 scale) and the presence of depression in the subjects or their families. The results are shown in Table 2.
Table 2:Orthorexia risk vs. depression occurrence in study subjects.
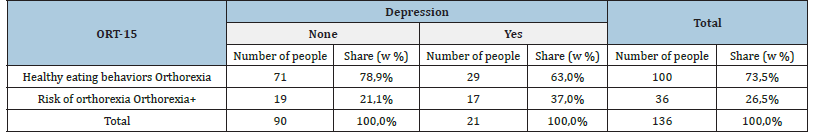
Depression was prevalent (according to self-assessment) in 33.8% (46) of the subjects. The risk of orthorexia occurred more often in those who had depression - 37.0% (17) than in those who did not - 21.1% (19). A statistically significant association was found between the presence of depression and the occurrence of orthorexia risk (chi square=3.924 p =0.048). Using the odds ratio, it was determined what the chance of orthorexia risk was for those who had depression. The resulting OR[95% CI]=2.191[1,000;4,798] indicates that the chance of orthorexia risk in the depressed group is 2.2 times higher than in the group without the disorder (Chart 2), Table 3.
Table 3:Risk of orthorexia vs. occurrence of depression in family of subjects.
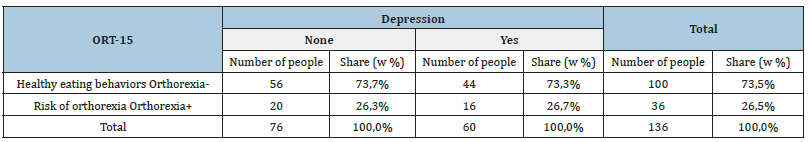
Chart 2:Risk of orthorexia vs. occurrence of depression in study subjects.
Depression was present (according to respondents’ assessment) in 44.1% (60) of respondents’ families. The risk of orthorexia occurred almost as often when there was and wasn’t depression in the family. The proportion of subjects who were found to be at risk for orthorexia was 26.7% (16) and 26.3% (20), respectively. There was no statistically significant association between the presence of depression in the family and the occurrence of orthorexia risk (chi square=0.002 p =0.963). The odds ratio indicating what the chance of orthorexia risk is in those with a history of depression is OR[95% CI]=1.018[0.473;2.192] and indicates that the chance of orthorexia risk in those with a family history of depression is the same in the group without the disorder (Table 4).
Table 4:Risk of orthorexia vs. occurrence of depression in subjects or in their family.
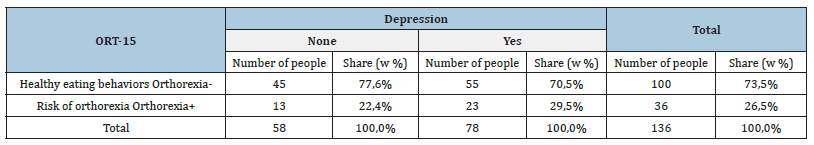
Depression was present (according to respondents’ selfassessment and evaluation) in 57.3% (78) of respondents or their families. The risk of orthorexia occurred more often if the respondent or his family had depression. The proportion of subjects who were found to be at risk for orthorexia was 29.5% (23), respectively, which was 7.1 percentage points higher than when there was no depression. There was no statistically significant association between the presence of depression in the subjects or in their family and the occurrence of orthorexia risk (chi square=0.855 p =0.355). The odds ratio indicating what the chance of orthorexia risk is in subjects with or in their families with depression is OR[95% CI]=1.447[0.660;3.177], and reports that the chance of orthorexia risk in this group of subjects is more than 44.7% higher than in the group without the disorder.
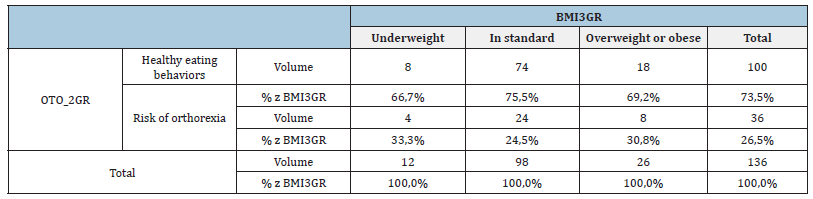
Risk: Orthorexia vs. BMI The survey showed that those who were observed to be at risk for orthorexia had a mean body mass index (BMI) of 22.07 (±4.78), while the group in which healthy behavior was observed had a mean BMI of 23.06 (±4.50). There was no statistically significant difference between the values (Mann-Whitney U=1673.5 p=0.533). No statistically significant correlation was found between the level of body mass index and ORT-15 score (Spearman’s rho= 0.042, p=0.626). The chart below shows the frequency of orthorexia depending on BMI (Table 5).
Table 5:Cross table OTO_2GR*BMI Chi kwadrat=0,735 p=0,693
Risk: orthorexia vs. addiction in the respondent and/or family member
We examined whether there was an association between the risk of orthorexia (ORT-15 scale) and the use of psychoactive substances by the subjects or their family members. The results are shown in Table 6.
Table 6:Psychoactive substance use by respondents and their family members.
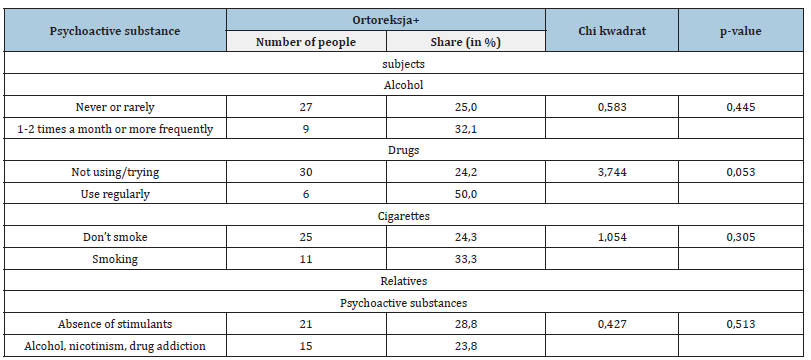
No statistically significant relationship was found with the use of stimulants by the subjects or in their families and the incidence of orthorexia risk. In the case of drug use, a p-value of 0.053 was obtained with the very small size of this group-12 people, so no statistically significant relationship between the variables should be found.
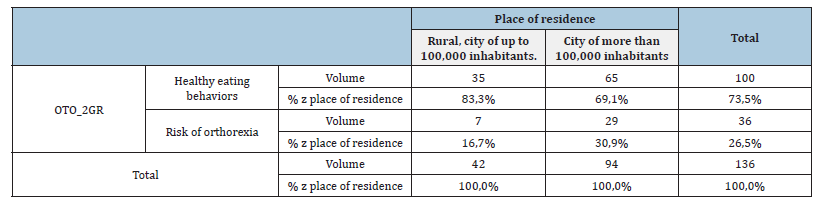
Risk: orthorexia vs. place of residence (large/small city/rural) It was analyzed whether the place of residence in relation to the size of its population, (defined in the questionnaire as a village, a city with a population of less than 100,000 people, a city with a population of more than 100,000 people), could somehow influence the development of ON, and no evidence was found for the importance of this parameter (Table 7). Risk: orthorexia vs. gender of the person surveyed
Table 7:Cross table OTO_2GR * Place of residence Chi kwadrat=3,001 p=0,083
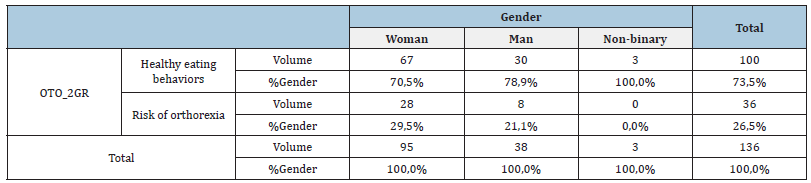
In the study group of 136 people, 95 women, 38 men and 3 non-binary people completed questionnaires. Gender had no statistically significant effect on the development of orthorexia nervosa (Table 8).
Table 8:Cross table OTO_2GR * Gender Chi kwadrat=2,093 p=0,351
Risk: orthorexia vs. respondent age
There was no statistically significant effect of age on the risk of orthorexia. Similarly, factors such as age, education, parents’ occupational status; having siblings, a life partner or remaining single are not significant.
Discussion
The prevalence score for orthorexia in the present study, set at 26.5%, is significantly higher than the prevalence studied by Donini, the author of the original publication on orthorexia and the most widely used diagnostic worksheet. In the original study, the risk of orthorexia was set at 6.9% [12]. Nevertheless, it is similar to our previous study involving a group of 864 people, at which time the prevalence of the disorder was estimated at 27% [6].
The gender of respondents in our observations is not a risk factor for orthorexia. Both previous and current studies do not support the widespread view that women, as people who are more focused on taking care of their health and are more likely to choose healthy lifestyles and diets, are more prone to a pathological fixation on eating, and are not consistent with the fact that eating disorders are significantly more common in women. Perhaps orthorexia is that clinical variant of eating disorders that is equally common in both sexes. Donini showed a higher prevalence of orthorexia among men [1], while a 2011 Turkish study showed a female preponderance among orthorexics in the population there [13] and our previous study in a younger age group, also found no difference regarding gender [6].
Another observation from the study is a lack of correlation of orthorexia with demographic and social characteristics of the subjects. A Polish study by Hrynik showed a significantly higher prevalence of orthorexia among children of working parents [14], while our study showed no significant correlation with occupational status or parental education. Similarly, orthorexia was not shown to correlate with having siblings, having a life partner or remaining single. Thus, social factors seem to have a negligible impact on the occurrence of orthorexia risk in adolescents and young adults.
The effect of psychoactive substance use among the subjects and their parents on the risk of orthorexia was not proven. Other results were presented by Hrynik, noting a higher rate of orthorexia among adolescents who smoke [14]. This information leads one to wonder whether the survey sufficiently identified the phenomenon of abuse or addiction to psychoactive substances and whether respondents gave honest answers. It seems that in eating disorders as well as in abusers or addicts-there is a similar problem with the recognition and regulation of emotions, so theoretically there could be coincidence between these disorders.
The present study has not proven a correlation of orthorexia with body mass index. In our previous study, as well as that of other authors-a significantly higher risk of orthorexia appeared with increasing BMI [6,14,15]. Among the studies referenced in this article, only Donini et al. [12] did not support the thesis of a connection between orthorexia and BMI. In contrast, other authors identify low BMI as a risk factor for the disorder [16,17]. It seems that this parameter requires further observation.
The current research found a statistically significant association between the presence of depression and the occurrence of orthorexia risk. Herpertz-Dahlmann and Remschmidt [18,19] conducted a study in which they compared the co-occurrence of eating disorder symptoms and depression, the results confirmed the conjecture regarding the reciprocal relationship between eating disorders and depression. Depressed patients were significantly more likely to have one form of eating disorder: anorexia or bulimia nervosa. Leassle et al. [20] point out that one of the most important aspects of eating disorder psychopathology is specific cognitive processing disorders and irrational self-esteem beliefs. In their study, they found positive correlations between the severity of depression and cognitive functioning - the higher the level of eating disorders, the higher the scores on the depression scale. Striving to maintain a slim figure, as well as perfectionism - correlated with the occurrence of depression. In the study, the authors proved the influence of cognitive impairment, characteristic of eating disorders, on the development and maintenance of depressive disorders. The correlation found in the current study confirms the cited observations.
Conclusion
The current findings seem to confirm reports by other researchers highlighting the high correlation between orthorexia and eating disorders [21]. We believe that in the absence of particularly significant and unequivocally identified risk factors specific to orthorexia-it should be included in the spectrum of eating disorders. All the more so because the factors indicated in the studies-dissatisfaction with one’s appearance and weight, striving for a slim figure, preoccupation with dieting and intense exerciseas statistically significant for the development of orthorexia, are equally significant in other eating disorders, especially for anorexia nervosa. Further research, of course is needed and the refinement and standardization of research tools to objectify observations.
Funding Statement
Funding sources: No financial support was received for this study.
References
- Donini LM, Marsili D, Graziani MP, Imbriale M, Cannella C (2004) Orthorexia nervosa: A preliminary study with proposal for diagnosis and attempt to measure the dimension of the phenomenon. Eat Weight Disord 9(2): 151-157.
- Dunn TM, Bratman S (2016) On orthorexia nervosa: A review of literature and proposed diagnostic criteria. Eat Behav 21: 11-17.
- Stochel M, Janas-Kozik M, Zejda JE, Hyrnik J, Jelonek I, et al. (2015) Validation of the ORTO-15 questionnaire in a group of urban youth aged 15-21. Psychiatr Pol 49(1): 119-134.
- Clifford T, Blyth C (2019) A pilot study comparing the prevalence of orthorexia nervosa in regular students and those in university sports teams. Eat Weight Disord 24(3): 473-480.
- Łucka I, Janikowska-Hołoweńko D, Domarecki P, Plenikowska-Ślusarz T, Domarecka M (2019) Orthorexia nervosa-a separate clinical entity, a part of eating disorder spectrum or another manifestation of obsessive-compulsive disorder? Psychiatr Pol 53(2): 371-382.
- Łucka I, Janikowska-Hołoweńko D, Domarecki P, Plenikowska-Ślusarz T, Domarecka M (2019) The prevalence and risk factors of orthorexia nervosa among school-age youth of Pomeranian and Warmian-Masurian voivodeships. Psychiatr Pol 53(2): 383-398.
- Bruch H (1971) Death in anorexia nervosa. Psychosom Med 33(2): 135-144.
- Bruch H (1983) Psychotherapy in primary anorexia nervosa. W: Esman HA, red. The psychiatric treatment of adolescents. Int Universities Press, New York, USA.
- Emmet SW (1980) Theory and treatment of anorexia nervosa and bulimia. Brenner/Mazel, New York, USA.
- Sours J (1985) Starving to death in the sea of objects. Jason Aronson, New York, USA.
- Barnes MA, Caltabiano ML (2017) The interrelationship between orthorexia nervosa, perfectionism, body image and attachment style. Eat Weight Disord 22(1): 177-184.
- Donini LM, Marsili D, Graziani MP, Imbriale M, Cannella C (2005) Orthorexia nervosa: Validation of a diagnosis questionnaire. Eat Weight Disord 10(2): 28-32.
- Bağci Bosi AT, Camur D, Güler C (2007) Prevalence of orthorexia nervosa in resident medical doctors in the faculty of medicine (Ankara, Turkey). Appetite 49(3): 661-666.
- Hyrnik J, Janas-Kozik M, Stochel M, Jelonek I, Siwiec A, et al. (2016) The assessment of orthorexia nervosa among 1899 Polish adolescents using the ORTO-15 questionnaire. Int J Psychiatry Clin Pract 20(3): 199-203.
- Bundros J, Clifford D, Silliman K, Neyman Morris M (2016) Prevalence of orthorexia nervosa among college students based on Bratman’s test and associated tendencies. Appetite 101: 86-94.
- Dell’Osso L, Abelli M, Carpita B, Pini S, Castellini G, et al. (2016) Historical evolution of the concept of anorexia nervosa and relationship with orthorexia nervosa, autism, and obsessive-compulsive spectrum. Neuropsychiatr Dis Treat 12: 1651-1660.
- Karniej P, Pérez J, Juárez‑Vela R, Santolalla‑Arnedo I, Gea‑Caballero V, et al. (2023) Orthorexia nervosa in gay men—the result of spanish-polish eating disorders study. BMC Public Health 23(1): 58.
- Herpertz-Dahlmann BM, Remschmidt H (1993) Depression in anorexia nervosa at follow-up. Int J Eat Dis 14(2): 163-169.
- Herpertz-Dahlmann BM, Wcwctzcr C, Rcmschmidt H (1995) The predictive value of depression in anorexia nervosa. Results of a seven-year follow-up study. Acta Psychiatr Scand 91(2): 114-119.
- Leassle RG, Fichter MM, Pirke KM (1988) Cognitive correlates of depression in patients with eating disorders. Int J Eating Dis 7(5): 681-686.
- Kiss-Leizer M, Rigó A (2019) People behind unhealthy obsession to healthy food: the personality profile of tendency to orthorexia nervosa. Eat Weight Disord 24(1): 29-35.
© 2023 Izabela Łucka. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 





.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






