- Submissions

Full Text
Advancements in Case Studies
Treatment of Supracondylar Fractures of the Humerus in Adults Using a Novel Anatomical Locking Plate on the Anterior Distal Humerus
Baoxin Zhang, Wanxiong He, Hao Wu, Ting Hao, Xiaolong Yang, Jie Cheng, Chao Ma, Guanghui Liu* and Jianzhong Wang*
The Second Affiliated Hospital of Inner Mongolia Medical University, China
*Corresponding author:Guanghui Liu and Jianzhong Wang, The Second Affiliated Hospital of Inner Mongolia Medical University, Hohhot, China
Submission:July 24, 2023;Published: August 01, 2023

ISSN 2639-0531Volume4 Issue1
Abstract
Due to its unique anatomical characteristics, supracondylar fractures of the humerus are often difficult to achieve firm fixation with internal fixation equipment, resulting in delayed functional exercise, often leaving cubitus varus deformity, elbow stiffness, contractures and other complications. Here, we report an adult patient with a supracondylar fracture of the humerus who underwent internal fixation through an anterior median incision in the humerus with our self-developed anterior anatomical locking plate of the distal humerus. During the 16-month follow-up period, the patient’s elbow range of motion was almost completely restored, functional scores were excellent, and there were no minor or major postoperative complications. We assumed this to be caused by our surgical reconstruction strategy for adult patients with supracondylar humeral fractures.
Keywords:Supracondylar fracture of humerus; Fracture of distal humerus; Open reduction and internal fixation; Locking plate
Introduction
Supracondylar fractures of the humerus are one of the most common types of fractures in the clinic. The clinical manifestations are elbow swelling, severe pain, and limited mobility. Some patients may have vascular and nerve damage [1,2]. Due to the unique anatomical characteristics of the humeral condyle, it is often difficult to achieve firm fixation with internal fixation equipment, resulting in delayed functional exercise and often left cubitus varus deformity [3-5], elbow stiffness, contractures and other complications [6,7]. At present, clinical treatment is more inclined to surgical treatment, mainly to achieve reduction and fixation, avoid complications, and restore upper limb motor function [8,9].
The previous internal fixation methods include Kirschner wire tension band fixation, traditional “Y”-shaped steel plate fixation, single steel plate and double steel plate fixation, etc [1]. However, the Kirschner wire tension band fixation method is simple and inexpensive, but the fixation strength is poor [10]. In addition, plaster external fixation is required after surgery, which is prone to loosening and fracture of internal fixation and it is difficult to ensure the smooth healing of fractures and the recovery of elbow joint function [11]. The traditional “Y”-shaped plate cannot conform to the anatomical relationship of the distal humerus due to its fixed bifurcation angle and can only be placed in the rear, which cannot form effective compression for complex intercondylar fractures. Single-plate fixation does not conform to the double-column fixation theory for supracondylar intercondylar fractures of the humerus [8]. Internal fixation with double plate, especially double locking plate, is currently recognized as an ideal method for the treatment of supracondylar and intercondylar fractures of the humerus [12]. Especially suitable for C-type fractures of the distal humerus [13,14], it can achieve the purpose of strong internal fixation and early functional exercise. The disadvantage is that it is difficult to pre-bend the steel plate, the operation is relatively complicated and the range of soft tissue stripping around the fracture is relatively wide, which affects the blood supply around the fracture end to a certain extent [1,15].
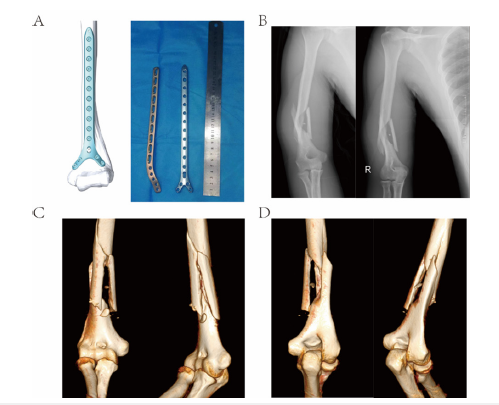
In this study, our self-developed anatomical locking plate for the anterior distal humerus (Figure 1A) was used for internal fixation of adult humeral supracondylar fractures through the anterior median incision of the humerus.
Figure 1:Patient plate with preoperative X-ray and CT-3D pictures. (A) Anterior anatomical locking plate of distal humerus, width: 13mm, thickness: 3mm, distal angle: 60°, length: 136mm, 152mm, 168mm, 184mm, 200mm, 232mm 6 models are optional. (B) Anteroposterior radiographs of the distal humerus of the patient within 6 hours after injury. (C-D) CT-3D scan pictures of the patient within 6 hours after injury.
Case Presentation
Medical history information
A 29-year-old man suffered an accidental fall that resulted in a right supracondylar fracture of the humerus with multiple soft-tissue contusions and no nerve, vascular and other injuries. Within 24 hours after injury, open and internal fixation was performed in our hospital using a new anatomical locking plate on the anterior distal humerus. Preoperative X-rays (Figure 1B), the patient was unable to cooperate due to severe pain and no lateral radiographs were taken) and 3D-CT scans (Figure 1C,1D) showed a supracondylar fracture of the humerus with a clear fracture line and significant displacement.
Surgical procedure
After successful brachial plexus block Anesthesia, the patient was placed supine on the operating table, the shoulder joint was abducted, and the upper limb was placed on the side table of the operating table. Routine disinfection with iodophor is used to disinfect the upper part of the affected limb and the affected side of the neck, above the central axis of the thorax and the level of the nipple and below the wrist joint. A sterile surgical drape is placed in the operating area, the trunk is covered with a sterile surgical drape and the affected hand is tightly wrapped with a sterile surgical drape.
The surgical approach takes the fractured end as the center and the skin and fascia layer are longitudinally incised along the anterior side of the upper arm, and the distal end of the incision reaches the cubital crease. Abdominal, the retractor pulls it to the medial side to expose and protect the musculocutaneous nerve. And along the middle of the brachialis muscle belly split longitudinally to expose the fracture and extend to the distal end to reach the coronoid fossa of the distal humerus. Continue to expose the front of the medial and lateral columns of the distal humerus down to the joint capsule. After the bone holder is reduced to the fractured end, the plate is flattened. When the anatomical locking plate on the anterior side of the distal humerus is placed, the bifurcation of the plate should be at the coronoid fossa. After it is attached to the bone surface, the sliding hole is first fixed, and the position of the plate can be adjusted up and down. The end is pressurized and fixed. The screw holes were locked at both ends of the fracture and a 3.2mm diameter drill was used to guide the drilling and the locking screws were respectively screwed in to fix the double cortex. Fixed locking screws can be selected for the medial and lateral columns of the distal humerus, up to a maximum of 4.
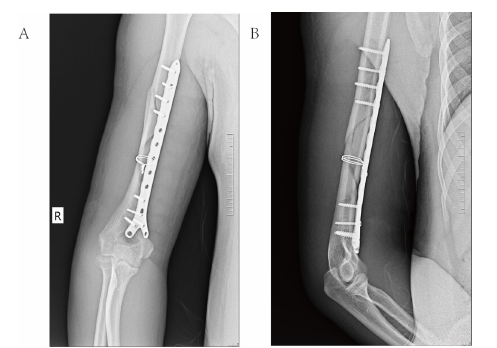
Intraoperative X-ray films (Figure 2A,2B) showed that the fracture was well reduced and fixed. Indwelling drainage tube, Figure 8 suture of the split brachialis muscle belly, reduction of the biceps belly, suture of the fascia layer, suture of the skin, sterile gauze bandage, the patient was returned to the ward.
Figure 2:Intraoperative X-ray Evaluation of the Patient. (A) Frontal radiograph of the patient after intraoperative plate placement. (B) Lateral radiograph of the patient after intraoperative plate placement.
The drainage tube was removed 48 hours after the operation and the active exercise of the hand and wrist, the isometric contraction of the biceps and forearm muscles and the active elbow flexion and extension exercise were performed on the second day after the operation.
Follow-up results
Routine follow-up was performed, and the fracture was healed 3 months after the operation and the X-ray photograph (Figure 3) showed a continuous callus crossing the fracture line; 9 months after the operation, the X-ray photograph showed the recanalization of the medullary canal at the fracture site; After 12 months, the patient’s elbow was pain-free and almost fully recovered (125° elbow flexion, 0° elbow extension, 90° supination of the forearm, 65° pronation) and the Mayo Elbow Performance Score (MEPS) was 100 points (excellent). 14 months after the operation, the patient came to our department for implant removal due to psychological factors. He had no pain in the elbow on the injured side, with a range of flexion-extension motion of 130°-0° and a supination-pronation rotation range of 90°-80°. The MEPS score was 100 and the patient was very satisfied.
Figure 3:Postoperative X-ray follow-up results of the patient. (A-C) X-ray pictures of the patient at 3 months, 6 months, and 12 months after operation. (D) X-ray pictures of the patient after removal of implants such as plates and screws at 14 months after operation.
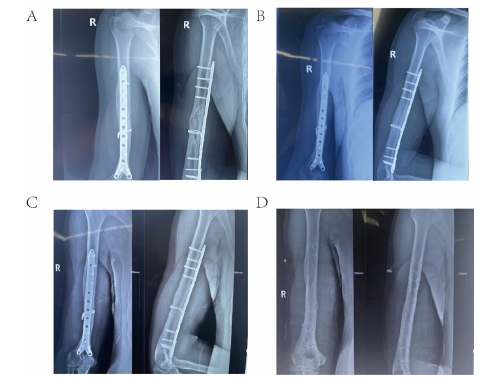
No secondary displacement or loss of reduction, implant loosening or internal fixation rupture and significant joint degeneration were observed after 16 months of routine followup. After the initial fixation procedure, no other postoperative complications such as infection, nonunion, delayed union, ulnar nerve symptoms, or donor site pain occurred. After hardware removal, the overall bony structure of the affected elbow joint remained intact and function recovered well.
Discussion and conclusion
Our self-developed anterior anatomical locking plate for distal humerus is suitable for fractures from the middle and lower humerus to 2cm above the coronoid fossa of the humerus. Anterior median incision of the humerus can be used, blunt longitudinal median separation of the brachialis muscle and retractor to pull it medially to protect the radial nerve, median nerve and brachial artery and the radial nerve does not need to be exposed during the operation. When drilling, it is recommended to limit the length of the drill bit to the length that just breaks through the contralateral cortex, so as to avoid damage to the contralateral blood vessels and nerves by the drill bit too long..
Advantages of this study
A. Two more plates are needed for the treatment of
supracondylar fractures of the humerus [1]. Now, only one
plate is needed to fix the anterior anatomical locking plate of
the distal humerus and the operation is simpler.
B. The radial nerve needs to be exposed during surgery for
supracondylar fractures of the humerus. Now it is not necessary
to expose the radial nerve through the anterior incision, which
can reduce the risk of radial nerve injury.
C. The distal end of the anterior anatomical locking plate of
the distal humerus is laid flat on the medial and lateral columns
of the humerus, avoiding the coronoid fossa and the olecranon
fossa, and promoting the early exercise of the flexion and
extension of the elbow joint, which is beneficial to the patient
The recovery of bone and joint function, shorten the fracture
healing time. And the distal end of the plate can be fixed with 4
screws, and the screw can be fixed to a length of about 20mm,
without hurting the distal blood vessels and nerves, and the
fixation is safer and more reliable.
D. In line with the anatomical characteristics of the distal
humerus, fixing the inner and outer columns of the distal
humerus can maximize the stability of the distal humerus
triangle and achieve firm fixation.
In conclusion, we propose a standardized surgical approach for adult patients with fractures of the middle and lower humerus, especially those located 2cm above the proximal humeral coronoid fossa. Using the anterior median incision of the humerus, open reduction and internal fixation with an anatomic locking plate on the anterior side of the distal humerus to restore and fix the structure of the distal humerus. Satisfactory clinical results have been achieved in our case, and it is worthy of clinical promotion and use. However, studies with longer follow-up periods are still needed to further assess long-term clinical outcomes, especially with regard to the development of post-traumatic osteoarthritis.
Conflict of Interest
There are no financial or other relations that could lead to a conflict of interest.
Acknowledgement
This work was supported by Inner Mongolia Autonomous Region Higher Education Scientific Research Project (NJZY21615), Science and Technology Planning Project of Inner Mongolia Science and Technology Department (2020GG0195 and 2022YFSH0021), Inner Mongolia Natural Science Foundation Project (2019MS08158 and 2020MS08164), Inner Mongolia Science and Technology Million Project (YKD2018KJBW(LH)002).
References
- Popkin CA, Rosenwasser KA, Ellis HB (2017) Pediatric and adolescent T-type distal humerus fractures. J Am Acad Orthop Surg Glob Res Rev 1(8): e040.
- Hope N, Varacallo M (2023) Supracondylar Humerus Fractures. In: StatPearls. Treasure Island (FL); StatPearls Publishing.
- Chagou A, Bassir RA, Rhanim A, Lahlou A, Berrada MS, et al. (2016) [Cubitus varus: external subtraction osteotomy, should it still be recommended? Retrospective study of 25 cases]. Pan Afr Med J 23: 263.
- Belthur MV, Iobst CA, Bor N, Segev E, Eidelman M, et al. (2016) Correction of cubitus varus after pediatric supracondylar elbow fracture: Alternative method using the Taylor spatial frame. J Pediatr Orthop 36(6): 608-617.
- Solichin I, Sandjaya G, Prabowo I, Dwi Putra NH, Rhatomy S (2021) The lateral curved osteotomy for cubitus varus deformity in children: A case report and literature review. Ann Med Surg (Lond) 65: 102315.
- Alrabaa RG, Simhon M, Kadiyala RK (2020) Outerbridge-Kashiwagi procedure for the treatment of a supracondylar humerus fracture malunion (O-K Procedure). Arthrosc Tech 9(3): e339-e344.
- Oura K, Shigi A, Oka K, Tanaka H, Murase T (2018) Corrective osteotomy for hyperextended elbow with limited flexion due to supracondylar fracture malunion. J Shoulder Elbow Surg 27(8): 1357-1365.
- Shih CA, Su WR, Lin WC, Tai TW (2019) Parallel versus orthogonal plate osteosynthesis of adult distal humerus fractures: A meta-analysis of biomechanical studies. Int Orthop 43(2): 449-460.
- Guven MF, Kaynak G, Inan M, Caliskan G, Unlu HB, et al. (2015) Results of displaced supracondylar humerus fractures treated with open reduction and internal fixation after a mean 22.4 years of follow-up. J Shoulder Elbow Surg 24(4): 640-646.
- Iobst CA, Bunhor D, Skaggs DL, Frick SL (2018) Intra-Operative bone stability test. Tech Orthop 33(4): 279-282.
- Pierreux PA, Moungondo F, Schuind FA (2020) Treatment of supracondylar humeral non-union by bone autograft and Hoffmann II external fixation. Orthop Traumatol Surg Res 106(2): 371-376.
- Salvador J, Castillón P, Fuentes I, Bernaus M, Anglès F (2017) Double plating as treatment for supracondylar humeral fractures. Rev Esp Cir Ortop Traumatol 61(5): 324-330.
- Zha Y, Hua K, Gong M, Jiang X (2021) Chronic type C3 distal humeral fracture associated with massive bone defects treated by open reduction and internal fixation with iliac crest autografts: A case report. BMC Musculoskelet Disord 22(1): 338.
- Wang C, Zhu Y, Long H, Lin Z, Zhao R, et al. (2021) Three-dimensional mapping of distal humerus fracture. J Orthop Surg Res 16(1): 545.
- Zaidenberg EE, Juarez Cesca F, Pastrana MJ, Zaidenberg CR (2018) Pedicled vascularized bone graft of the distal radius for recalcitrant nonunion of the distal humerus. J Orthop Trauma 32(10): e394-e399.
© 2023 Guanghui Liu and Jianzhong Wang. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 





.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






