- Submissions

Full Text
Advancements in Case Studies
The Impact of Sars-Covid19 Pandemic on Multidrug Resistant Bacteria Colonization in Stem Cell Transplantation in the Era of New Agents
Alessandra Picardi1,2,*, Mariangela Pedata1, Serena Marotta1, Tiziana Ascione3, Stefania Leone1, Ilaria Migliaccio1, Maria Esposito1, Aldo Leone1, Domenico Buonanno1, Mirella Alberti1, Mafalda Caputo1, Rosa Peluso1, Felicetto Ferrara4 and Maria Celentano1
1Stem Cell Transplant Program of AORN Cardarelli, Naples, Italy
2Biomedicine and Prevention Department of Tor Vergata University, Rome, Italy
3Health Direction of AORN Cardarelli, Naples, Italy
4Hematology Unit of AORN Cardarelli, Naples, Italy
*Corresponding author:Alessandra Picardi, Head of the Stem Cell Transplant Program of AORN Cardarelli, Naples, Italy
Submission:June 16, 2023;Published: July 05, 2023

ISSN 2639-0531Volume4 Issue1
Abstract
Infections are among the major cause of mortality in patients receiving allogeneic hemopoietic stem cell transplantation (HSCT). In the last decades, the progressive raise of Carbapenemic Resistant Enterobacteriaceae (CRE) infections was associated with a concomitant increase in terms of morbidity and mortality rates. The primary aims of our retrospective analysis were to assess the impact of SARSCOVID19 Pandemic on CRE colonization at our Transplant Program and the efficacy of new antibiotics on the 100 days and 1-yr Transplant Related Mortality in both CRE colonized and non-colonized patients. CRE colonization resulted significantly lower during SARS-COVID19 Pandemic (p<0.0001), related to the COVID-19 associated restrictions adopted at the AORN Cardarelli Hospital, in Naples. However, the outcomes of CRE colonized and non-colonized patients who underwent allogeneic Hematopoietic Stem Cell Transplant procedure were similar in terms of morbidity and mortality (p=ns).
Keywords:SARS-COVID19 pandemic; Allogeneic hemopoietic stem cell transplantation; Carbapenemic resistant Enterobacteriaceae
Abbreviations:AORN: Azienda Ospedaliera di Rilievo Nazionale; Allo-HSCT: Allogeneic Hemopoietic Stem Cell Transplantation; CRE: Carbapenemic Resistant Enterobacteriaceae; TRM: Transplant Related Mortality; GvHD: Graft Versus Host Disease; HLA: Human Leukocyte Antigens; BM: Bone Marrow; PBSC: Peripheral Blood Stem Cells; TBI: Total Body Irradiation; TBF: Thiotepa Busulphan Fludarabine; AML: Acute Myelogenous Leukemia; ALL: Acute Lymphoblastic Leukemia; PT-CY: Post-transplant Cyclophosfamide; CSA: Cyclosporine; ATG: Anti-Thymocyte Globuline; MTX: Metotrexate; MDR: Multi Drug Resistant
Introduction
Allogeneic hematopoietic stem cell transplantation (allo-HSCT) has become a widely used therapeutic strategy for many malignant and non-malignant hematologic disorders [1]. While relevant advances have been made in the field [2,3], infection still remains one of the most severe and frequent complications of allo-HSCT [4-6]. The CRE colonization represents an important risk factor predisposing allo-HSCT recipients to severe sepsis, in particular during the aplasia period after the conditioning regimen [7-10]. Moreover, beyond the conditioning regimen intensity, local epidemiological factors, type of donor, stem cell source, grade of HLA matching, occurrence of complications such as Graft versus Host Disease (GvHD), are also relevant [11,12]. In this context, while SARS-COVID19 pandemic has represented a major risk factor for letal viral infections in about 20% of allo-HSCT recipients, on the other hand, the restriction measures suggested by the World Health Organization and local authorities and worldwide adopted [13] could have played a protective role in terms of patient’s bacteria colonization. Herein, we report results from a retrospective monocentric analysis of the AORN Cardarelli Transplant Program concerning the impact of SARS COVID-19 pandemic on multidrug resistant bacteria colonization in the era of new antibiotic agents. The aims were to compare the 2 cohorts (pandemic versus non pandemic restrictions) in terms of CRE colonization rate, hospitalization’s duration, PMN/ PLTS engraftment, complications and transplant related mortality.
Materials and Methods
Overall, 83 consecutive patients, (52 males and 31 females) with a median age of 48 years (20-69), underwent a first allogeneic HSCT. Fifty-nine patients (71%) were affected by high risk Acute Leukemia (Acute Myeloid Leukemia n=43, Acute Lymphoblastic n=16). The donor was HLA identical sibling, matched unrelated, haploidentical related or mismatched unrelated donor in 41%, 26.5%, 28% and 5% of cases, respectively. Stem cell source was Bone Marrow (BM) and Peripheral Blood Stem Cells (PBSC) in 33% and 67% of allo-HSCT. The conditioning regimen consisted of a myeloablative schedule in 61% of cases and was Total Body Irradiation (TBI) based or Valencia schedule (TBF) in almost all ALL (75%) and AML (82%), respectively. As GvHD prophylaxis, the combination of post-transplant Cyclophosfamide (PT-CY), mycophenolate-mofetil (MMF) and cyclosporine (CSA) was used for haploidentical or mismatched unrelated allo-HSCT while CSA and MTX with or without the anti-thymocyte globuline (ATG, Fresenius) were used in case of BM HLA-identical related donor or matched unrelated (regardless, the stem cell source) or PBSC related HSCT, respectively. CRE colonized patients reporting fever received empirical antibiotic treatment based on ceftazidime/ avibactam, meropenem/vaborbatcam and cefiderocol.
Data have been collected from a series of 83 consecutive adult patients who received an allo-HSCT at AORN Cardarelli Transplant Program in Naples, between July 2019 and November 2022. All patients signed an informed consent for the transplant procedure and data collection. Collected data included: age, status disease and infectious status at allo-HSCT, date of allo-HSCT, conditioning regimen, type of donor and HLA matching, source of stem cell, GvHD prophylaxis, complications after allo-HSCT, date and status at last follow up. Moreover, the germ causing sepsis in case of fever and the antibiotic therapy were also recorded. The patients were divided into 2 groups according to the non-pandemic versus pandemic SARS-COVID19 period with associated restrictions (March 2020-July 2021).
For the comparison of categorical data, the Chi-Square test has been applied in contingency tables. Differently, for continuous variables with a normal distribution, the T-test for independent variables has been used. To evaluate the cumulative risk of mortality due to transplantation complications (Transplant Related Mortality- TRM), the Kaplan-meier method has been used. In addition, to compare the TRM rate between different cohorts of patients the long-rank test has been used. Statistical significance is accepted with a p<0.05. All the statistical evaluations and the graphical production have been performed with the software SPSS.
Results and Discussion
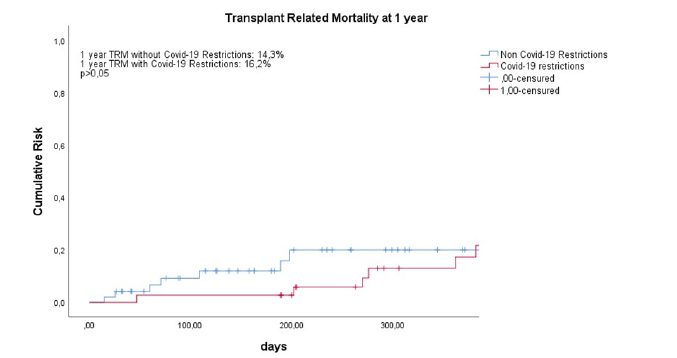
Overall, 35 out of 83 (42%) patients were colonized by CRE. Worthy of note, CRE colonization was significantly higher (p<0.0001) in absence of COVID-19 associated restriction with a rate of 61% (29/47) versus 19% (7/36) in presence of COVID-19 associated restrictions. On the contrary, comparing the outcomes of the 2 cohorts in terms of infectious complications (p=0.69), early (p=0.146) and late TRM (p=0.55), no significant difference was observed. Figures 1 & 2 show early and late TRM of the patients who underwent allo-HSCT during the COVID-19 associated restrictions (2,7%, 16,2%) versus who have not COVID19 associated restrictions (10,2%, 14,3%).
Figure 1:Transplant Related Mortality (TRM) evaluated in the first 100 days after transplantation in the two cohorts, in presence and in absence of Covid-19 restrictions. An event is defined as a death caused by a transplant related complication. Censured are patients who have stopped the follow up, because of death or others personal decision. The cumulative risk of death due to transplantation has been compared with the Kaplan-Meier method and the long-rank test. Statistical significance is accepted with a p> 0,05.
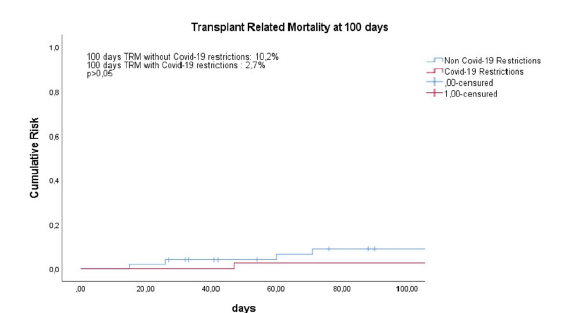
Figure 2:Transplant Related Mortality (TRM) evaluated at one year after transplantation in the two cohorts, in presence and in absence of Covid-19 restrictions. An event is defined as a death caused by a transplant related complication. Censured are patients who have stopped the follow up, because of death or others personal decision. The cumulative risk of death due to transplantation has been compared with the Kaplan-Meier method and the longrank test. Statistical significance is accepted with a p> 0,05.
Moreover, there were no significant differences in terms of median hospitalization duration, median time to PMN and PLTS recovery and aGVHD occurrence, 39 (20-75) vs 43 days (25-109) (p=ns), 21 (8-97) vs 21 days (6-53) (p=ns) and 18 (11-25) vs 17 (10-27) days (p=ns) and 4.32 vs 9.5 % (p=ns) in patients who underwent allo-HSCT during the COVID-19 associated restrictions versus who have not subjected to COVID19 associated restrictions.
COVID-19 associated restrictions significantly reduced the CRE colonization rate at our Transplant Program. Conceivably, the effective restrictive measures adopted during the pandemic period such as social distancing, limitations of the outpatient visits, forbidden access to visitors in the ordinary hospitalization ward, the dedicated staff to a COVID-19 free clinical transplant unit, the familiar care givers’ use of facial masks and more careful hands washing represented a pivotal factor in terms of reduction of CRE colonization of patients to undergo allo-HSCT [13].
Although CRE colonized patients are considered at high risk of an unfavourable outcome, in our case-series, an empiric schedule considering novel anti-MDR antibiotics for febrile cases allowed the disappearance of the difference in terms of poor outcome of CREcolonized patients in respect to non-colonized cases.
Conclusion
Our retrospective case-series analysis highlights the impact of a rigorous application of hygienic restrictions, such as during COVID19 pandemic, on the incidence of CRE colonization in HSCTs. This data should be taken into account at Transplant Programs in order to adopt the best measures for minimizing CRE colonization. Indeed, multi-resistant bacterial colonization represents the major cause of mortality in patients receiving allogeneic HSCT for sepsis mainly in the early post-transplantation period [10]. The recent introduction of novel anti-MDR antibiotics is progressively changing the epidemiology and outcome of CRE infections. The absence of difference in terms of outcome during non-pandemic versus pandemic SARS-COVID19 period, with associated restrictions, represents indirect evidence of the efficacy of the empirical use of antibiotic treatment, based on ceftazidime/avibactam, meropenem/vaborbatcam and cefiderocol, in febrile colonized patients. Thus, in HSCT setting, an empirical and aggressive antimicrobial strategy could balance the well-known unfavourable outcome of CRE colonization. However, the retrospective nature and the small sample size represent the limits of this analysis but is worth to note that also a catastrophic event, such as pandemic SARS-COVID 19, may introduce better clinical practices for the patient’s management.
Acknowledgements
To all patients and nurse’s staff.
Conflict of Interest
No conflict of interest to declare.
List of Individuals Who Contributed in the Work
AP and TA designed the retrospective observational study, MP, SM, IM, RP MC, DB, MA, MC, RP took care of patients, FF revised the paper, SL performed the statistical analysis, ME and AL collected data.
References
- Balassa K, Danby R, Rocha V (2019) Haematopoietic stem cell transplants: principles and indications. Br J Hosp Med 80(1): 33-39.
- Norkin M, Wingard JR (2017) Recent advances in hematopoietic stem cell transplantation. F1000Research 6: 870.
- Bittencourt MCB, Ciurea SO (2020) Recent advances in allogeneic hematopoietic stem cell transplantation for acute myeloid leukemia. BBMT 26(9): e215-e221.
- Wingard JR, Hsu J, Hiemenz JW (2010) Hematopoietic stem cell transplantation: An overview of infection risks and epidemiology. Infect Dis Clin N Am 24(2): 257-272.
- Bjorklund A, Aschan J, Labopin M, Remberger M, Ringden O, et al. (2007) Risk factors for fatal infectious complications developing late after allogenic stem cell transplantation. Bone Marrow Transplant 40(11): 1055-1062.
- Mikulska M, Del Bono V, Bruzzi P, Raiola AM, Gualandi F, et al. (2012) Mortality after bloodstream infections in allogenic haematopoietic stem cell transplant (HSCT) recipients. Infection 40(3): 271-278.
- Garnica M, Maiolino A, Nucci M (2009) Factors associated with bacteremia due to multidrug-resistant gram-negative bacilli in hematopoietic stem cell transplant recipients. Braz J Med Biol Res 42(3): 289-293.
- Pouch SM, Satlin MJ (2017) Carbapenem-resistant Enterobacteriaceae in special populations: Solid organ transplant recipients, stem cell transplant recipients and patients with hematologic malignancies. Virulence 8(4): 391-402.
- Satlin MJ, Chavda KD, Baker TM, Chen L, Shashkina E, et al. (2018) Colonization with levofloxacin-resistant extended-spectrum β-Lactamase-producing Enterobacteriaceae and risk of bacteremia in hematopoietic stem cell transplant recipients. Clin Infect Dis 67(11): 1720-1728.
- Yuan W, Xu J, Guo L, Chen Y, Gu J, et al. (2022) Clinical risk factors and microbiological and intestinal characteristics of carbapenemase-producing Enterobacteriaceae colonization and subsequent infection. Microbiol Spectr 10(6): e0190621.
- Anasetti C (2008) What are the most important donor and recipient factors affecting the outcome of related and unrelated allogeneic transplantation. Best Pract Res Clin Haematol 21(4): 691-697.
- Picardi A, Sacchi N, Miotti V, Lorentino F, Oldani E, et al. (2021) Alleic HLA matching and pair origin are favourable prognostic factors for unrelated hematopoietic stem cell transplantation in neoplastic hematologic diseases: An Italian analysis by the GTIMO, IBMDR and AIBT. Transplant Cell Ther 27(5): 406.e1-406.e11.
- Ljungman P, Mikulska M, Styczynski J, De la Camara R (2021) Coronavirus disease COVID-19: EBMT recommendations version 14, pp. 1-14.
© 2023 Alessandra Picardi. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






