- Submissions

Full Text
Advancements in Case Studies
Guttate Psoriasis in Images, A Sign of Streptococcal Tonsillopharyngitis
Ana Luísa Ribeiro1*, Carlos Magalhães Vieira1, Marta Pires Ribeiro1 and Carlos Santos2
1Family Medicine, ACeS Alto Tâmega e Barroso, Chaves, Portugal
2Family Medicine, ULS Nordeste, Bragança, Portugal
*Corresponding author: Ana Luísa Ribeiro, UCSP Montalegre, ACeS Alto Tâmega e Barroso, Portugal
Submission:January 13, 2023;Published: April 13, 2023

ISSN 2639-0531Volume3 Issue5
Abstract
This report presents two cases of systemic Kaposi’s sarcoma (KS) in HIV-positive women from Gabon and Equatorial Guinea. KS is caused by Human Herpes Virus 8 (HHV8) and is a common cancer among HIV-infected individuals in Africa. The equatorial form of KS is aggressive and affects individuals of all ages and is commonly found in Central and South Africa, including Gabon. Both patients had multifocal involvement and several localizations and were treated at the Omar Bongo Ondimba Military Hospital in Libreville, Gabon. The coexistence of HIV and HHV8 has contributed to the high prevalence of this disease in both endemic and epidemic areas.
Keywords:Guttate Psoriasis; Streptococcal Infection; Tonsillopharyngitis
Abbreviations:GP: Guttate Psoriasis; GAS: Group A Strep
Introduction
The single dermatological manifestation of group A Streptococcal tonsillopharyngitis described in literature is scarlet fever [1]. Also, according to evidence 56 to 97% of first exacerbations of GP are associated to GAS [2] pharyngitis, but it is stated to arise only 3-4 weeks following a GAS infection, often misdiagnosed as a reaction to antibiotics used to treat streptococcus [3]. This manifestation is mediated by streptococci-specific T cells that crossreact against epidermal autoantigens [2]. To our knowledge no case of concomitant GP and GAS tonsillopharyngitis was reported as in this case, only cases of GP after the pharyngeal infection.
Description
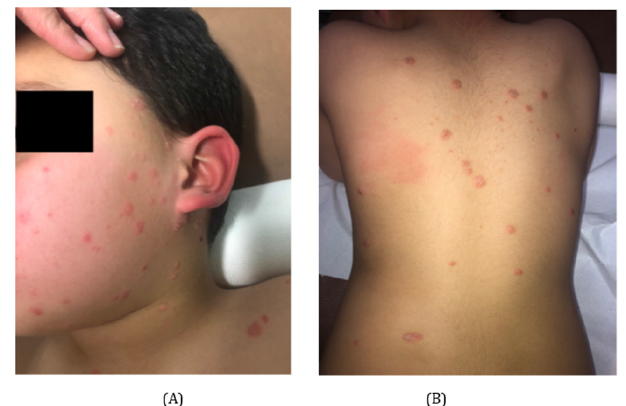
A 5-year-old male child, previously healthy, was brought by his mother to the primary care clinic with a pruriginous skin rash of 6 days duration. The rash started as two discrete erythematous plaques on the face and spread as multiple lesions to trunk and limbs. The patient also reported concomitant symptoms of sore throat and malaise, with normal body temperature according to the mother. On examination, he presented pharyngeal/tonsillar hyperemia, low grade fever and multiple drop-like well circumscribed pink erythematous papules with central scale (Figure 1), measuring between 5 to 10mm in size, localized on the face, trunk and extremities, spearing palms, soles and scalp. An oropharyngeal swab was collected and revealed positive on GAS rapid antigen test..
Figure 1:A and B: Multiple drop-like well circumscribed salmon pink erythematous papules with a fine scale, consistent with guttate psoriasis on first medical evaluation (day six after eruption).
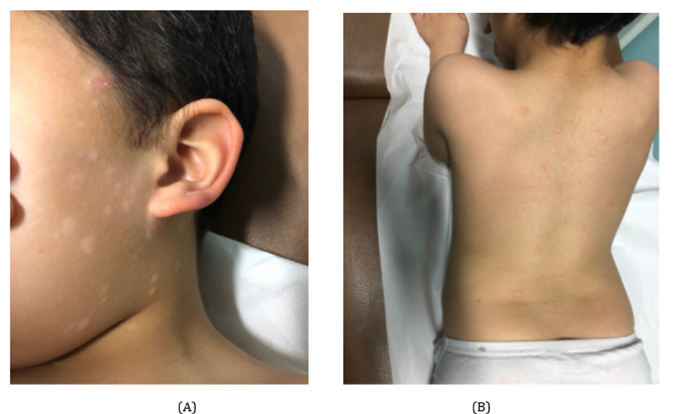
Our patient started directed treatment to GP with topical association of betamethasone dipropionate 0,05% and salicylic acid 3% twice daily on skin lesions for 1 week, and with 10 days of amoxicillin 50mg/kg/day for GAS tonsillopharyngitis infection. Absence from school was indicated until recovery. On reevaluation at day 8 of treatment, we observed full remission of symptoms and papules, persisting a residual post inflammatory hypopigmentation on previous lesion location (Figure 2), that gradually returned to normal skin pigmentation over the following 4 months.
Figure 2:A and B: Lesions after 1 week of topical treatment and oral antibiotic for GAS pharyngitis. Significant clinical improvement with residual hypopigmentation.
Patient’s Perspective
Both patient and mother stated being very satisfied with the outcome and reassured after rapid remission of skin lesions, since the child was being rejected at school stating, “they didn’t want to play with me due to my wounds”. He no longer suffered other episodes or forms of tonsillitis or psoriasis the following year and social life returned to normal.
Discussion
To non-dermatologist doctors, diagnosing GP can be complex and often mistaken for other infections or a skin reaction to treatment. A typical GP lesion is a drop like well circumscribed millimetric pink erythematous papule, typically with 2 to 15mm, with central scale, and occurs mainly in children and young adults. This condition should trigger clinical suspicion of a streptococcal infection like GAS [3,4]. GAS tonsillopharyngitis infection may have severe cardiac, renal, neurologic and suppurative complications if untreated, like acute rheumatic fever, poststreptococcal glomerulonephritis, pediatric autoimmune neuropsychiatric disorders associated with streptococcus (PANDAS), necrotizing fasciitis and peritonsillar abscess/cellulitis [1]. Early identification and timely antimicrobial therapy are important to minimize and prevent disease transmission [1] and some complications [5].
Conclusion
This case raises awareness to the fact that typical GP lesions, apart from scarlet fever rash, in a patient with clinical manifestations of GAS tonsillopharyngitis, might also be a precocious sign of the disease, allowing prompt infection investigation and treatment.
References
- Wald ER (2022) Group A streptococcal tonsillopharyngitis in children and adolescents: Clinical features and diagnosis. UpToDate.
- Prinz JC (2001) Psoriasis vulgaris-a sterile antibacterial skin reaction mediated by cross-reactive T cells? An immunological view of the pathophysiology of psoriasis. Clin Exp Dermatol 26(4): 326-332.
- Vence L, Schmitt A, Meadows CE, Gress T (2015) Recognizing guttate psoriasis and initiating appropriate treatment. W V Med J 111(4): 26-28.
- Mehlis S (2020) Guttate psoriasis. UpToDate.
- Del Mar C (1992) Managing sore throat: A literature review. II. Do antibiotics confer benefit? Med J Aust 156(9): 644-649.
© 2023 Ana Luísa Ribeiro. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






