- Submissions

Full Text
Advancements in Case Studies
HIV-Related Kaposi’s Sarcoma at the Omar Bongo Ondimba Military Hospital in Libreville: Two Clinical Cases
Iroungou Berthe A2*, Nzenze Jean Raymond1 and Mangouka Guignali Laurette1
1Internal Medicine Service-Omar Bongo Ondimba Armed Forces Training Hospital (HIA OBO, Libreville, Gabon
2Joint Research Unit International Center for Medical Research of Franceville-Military Health Service (UMR CIRMF-SSM), Libreville, Gabon
*Corresponding author: Iroungou Berthe Amélie, Joint Research Unit International Center for Medical Research of Franceville - Military Health Service (UMR CIRMF-SSM), BP: 20404, Libreville, Gabon
Submission:February 20, 2023;Published: March 01, 2023

ISSN 2639-0531Volume3 Issue5
Abstract
This report presents two cases of systemic Kaposi’s sarcoma (KS) in HIV-positive women from Gabon and Equatorial Guinea. KS is caused by Human Herpes Virus 8 (HHV8) and is a common cancer among HIV-infected individuals in Africa. The equatorial form of KS is aggressive and affects individuals of all ages and is commonly found in Central and South Africa, including Gabon. Both patients had multifocal involvement and several localizations and were treated at the Omar Bongo Ondimba Military Hospital in Libreville, Gabon. The coexistence of HIV and HHV8 has contributed to the high prevalence of this disease in both endemic and epidemic areas.
Keywords:Kaposi’s Sarcoma; HIV; ART; Lymphocyte TCD4; Gabon
Introduction
Kaposi’s sarcoma (KS) is the most prevalent cancer among HIV-infected individuals in Africa and is caused by the Human Herpes Virus 8 (HHV8). The coexistence of both viruses (HIV and HHV8) has contributed to the explosion of this disease in endemic and epidemic areas, with KS being particularly recurrent in Central and South Africa [1]. Gabon, a small country in Central Africa, exhibits the equatorial form of KS, which is endemic and affects all age groups (endemic KS). This form of the disease is typically aggressive and can affect both adults and children [2]. In this report, we describe two cases of systemic Kaposi’s sarcoma in HIV-positive women from Gabon and Equatorial Guinea. The disease was found to have multifocal involvement and several localizations, and both patients received treatment at the Omar Bongo Ondimba Military Hospital in Libreville.
Case Presentation
First case: A 30-year-old woman from Equatorial Guinea, who was HIV-positive and taking Tenofovir-Emtricitabine and Efavirenz (TDF+FTC/EFV) for antiretroviral therapy (ART) was admitted to the department of internal medicine due to a tumor syndrome. She was experiencing impaired general condition and progressive loss of autonomy.
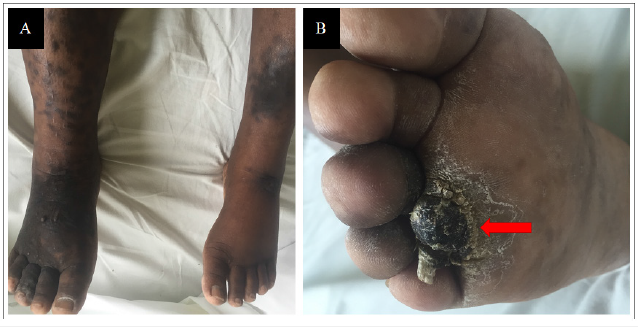
Physical examination revealed Kaposi’s sarcoma lesions on the soft palate (Figure 1), infiltrated and nodular lesions on the lower limbs (Figures 2A and 2B), cervical and axillary adenopathy and respiratory distress. The patient was also presented with edema of the lower limbs, resembling lymphedema and a poorly tolerated clinical anemic syndrome.
Figure 1: displays Kaposi’s sarcoma lesions on the soft palate. Images sourced from the internal medicine department of HIA OBO.

Figure 2:Shows nodular Kaposi’s sarcoma lesions, predominantly located on the right lower limb as seen in Figure 2A. The lesion on the upper third of the right plantar arch, shown in Figure 2B (Red Arrow), is also indicative of Kaposi’s sarcoma. Images from the internal medicine department of HIA OBO.
Laboratory analyses showed anemia (9g/dl), thrombocytopenia (125000/mm3) and inflammatory biological syndrome (CRP: 108mg/l). Co-infections with Hepatitis B or C were ruled out. The lymphocyte TCD4 count was 307/mm3, and the patient had impaired renal function, which could be attributed to either HIV-related nephropathy (HIVAN) or Tenofovir-related toxicity. The thoraco-abdomino-pelvic CT scan revealed bilateral alveolo-interstitial infiltration with mediastinal and abdominal adenomegaly and bilateral pleural effusion of medium abundance. Upper digestive endoscopy revealed grade III esophagitis, and the staged biopsies were suggestive of diffuse gastric Kaposi’s sarcoma, which was also confirmed on cutaneous biopsies.
Following a multidisciplinary consultation, we started chemotherapy with Bleomycin and switched the initial ART to a combination therapy of Abacavir-Emtricitabine/Lopinavir ritonavir (ABC+FTC/LPV/r). Despite this treatment, the patient’s condition deteriorated, and she passed away after completing the fifth cycle of chemotherapy.
Second case: A 27-year-old Gabonese woman, who had been HIV-positive for five years and non-compliant with ART for one year, was admitted for a tumoral syndrome with diffuse edematous infiltration and voluminous lymphedema of the lower limbs, predominantly on the right. The patient presented with numerous pustules and diffused infiltrated lesions on the lower right limb, specifically at the root levels of the right thigh, indicative of Kaposi’s sarcoma lesions with evidence of bacterial superinfection with Pseudomonas aeruginosa (Figure 3A and 3B).
Figure 3:Showing purplish and infiltrating nodular lesions on the anterior surfaces of the root of the right thigh. Figure 3A is indicative of Kaposi’s sarcoma lesions ten days prior to admission, while Figure 3B shows lesions of the right thigh on admission that are also indicative of Kaposi’s sarcoma. Additionally, Figure 3A (white arrow) shows evidence of bacterial superinfection with Pseudomonas aeruginosa on the right thigh. Images sourced from the internal medicine department of HIA OBO.

The biological workup revealed severe microcytic anemia (5g/dl) and active inflammation (CRP: 114mg/l). The thoracoabdomino- pelvic CT scan showed bilateral alveolar interstitial infiltration with mediastinal and diaphragmatic adenomegaly. Cutaneous biopsies favored a diagnosis of systemic Kaposi’s sarcoma, which was uncontrolled due to HIV. However, the patient’s condition did not improve with chemotherapy, and she ultimately died due to her illness.
Discussion
HHV8 antibody assays and HHV8 (Human Herpes Virus Type 8) PCR tests, which are used to detect the virus, were not performed in our hospital due to the high cost of these tests and the lack of a suitable technical platform. However, the strong association between HHV8 and Kaposi’s sarcoma in AIDS patients is widely recognized based on numerous studies conducted worldwide [2- 5]. Therefore, the inability to perform these tests may have limited our ability to fully characterize the viral component of our patients’ Kaposi’s sarcoma.
In addition, it is worth noting that Kaposi’s sarcoma can occur in HIV-positive individuals who have a permanently controlled viral load and a high CD4 cell count, as observed in our first case [3,4]. This highlights the fact that Kaposi’s sarcoma is not solely a consequence of advanced HIV disease but can also arise in patients with well-controlled HIV infection. Additionally, these two case reports highlight the importance of regular monitoring and early detection of Kaposi’s sarcoma in all HIV-positive individuals, regardless of their CD4 cell count or viral load. These findings provide insight into the difficulties of treating HIV-positive patients with Kaposi’s sarcoma in a clinical setting, particularly given the disease’s grim prognosis and its occurrence in 38% of initial AIDS cases, as reported in the 2013 Morlat report [6].
Conclusion
Kaposi’s sarcoma is a significant public health concern in Africa, especially among HIV-positive individuals. However, despite receiving appropriate treatment, the two reported cases of systemic Kaposi’s sarcoma in HIV patients had poor outcomes. Our findings highlight the urgent need for improved access to diagnostic tests and optimized treatment strategies for Kaposi’s sarcoma in the African context. Therefore, continued research into the pathogenesis and management of Kaposi’s sarcoma in the region are necessary to improve patient outcomes and reduce the burden of the disease.
References
- Institut Pasteur (2011) Kaposi's sarcoma.
- Kaposi’s Sarcoma. Union for International Cancer Control. 2014 Review of Cancer Medicines on the WHO List of Essential Medicine.
- Robert Dubrow, Li Qin, Haiqun Lin, Wendy Leyden, Keri N Althoff, et al. (2017) Association of CD4+ T-cell Count, HIV-1 RNA Viral Load, and Antiretroviral Therapy with Kaposi Sarcoma Risk Among HIV-infected Persons in the United States and Canada. J Acquir Immune Defic Syndr 75(4): 382-390.
- Vanda Akico Ueda Fick De Souza, Ligia Camera Pierrotti, Laura Masami Sumita, Wilton Santos Freire, Aluisio Augusto Cotrim Segurado, et al. (2007) Sero-reactivity to Kaposi's sarcoma-associated herpesvirus (human herpesvirus 8) latent nuclear antigen in AIDS-associated Kaposi's sarcoma patients depends on CD4+ T-cell count. J Med Virol 79(10): 1562-1568.
- Lucia Brambilla, Giovanni Genovese, Emilio Berti, Ketty Peris, Franco Rongioletti, et al. (2021) Diagnosis and treatment of classic and iatrogenic Kaposi's sarcoma: Italian recommendations. Ital J Dermatol Venerol 156(3): 356-365.
- Morlat P (2013) Medical care for people living with HIV. Recommendations of the expert group report 2013. Ministry of Social Affairs and Health, Paris, France.
© 2023 Iroungou Berthe A. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






